Red Cell Teaching Cases: Anemia Evaluation and Differential Diagnosis
Course Directors Breakfast session at ASH 2012 highlighting various aspects of red cell disorders, including case discussions, laboratory findings, and clinical considerations. Case 1 involves a 35-year-old woman presenting with anemia symptoms, requiring detailed evaluation and management. The session covers a range of topics from anemias to hemostasis and thrombosis, emphasizing disease recognition, differential diagnosis, and understanding pathophysiology.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
RED CELL TEACHING CASES Alice Ma, MD University of North Carolina Course Directors Breakfast ASH 2012
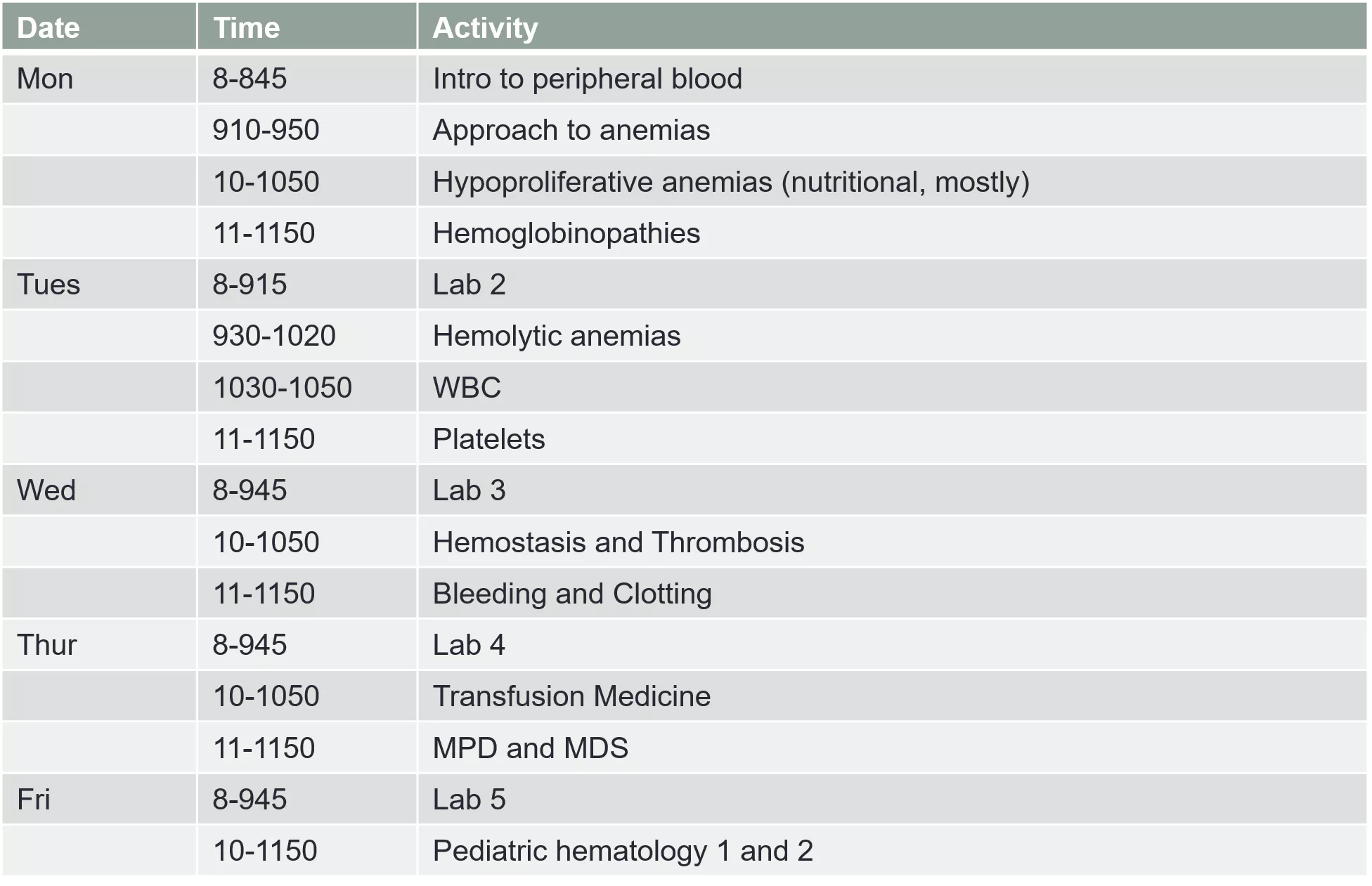
Overview Date Time Activity Mon 8-845 Intro to peripheral blood 910-950 Approach to anemias 10-1050 Hypoproliferative anemias (nutritional, mostly) 11-1150 Hemoglobinopathies Tues 8-915 Lab 2 930-1020 Hemolytic anemias 1030-1050 WBC 11-1150 Platelets Wed 8-945 Lab 3 10-1050 Hemostasis and Thrombosis 11-1150 Bleeding and Clotting Thur 8-945 Lab 4 10-1050 Transfusion Medicine 11-1150 MPD and MDS Fri 8-945 Lab 5 10-1150 Pediatric hematology 1 and 2
Course Plan Large group lecture Small group case discussion the morning after Exam Q s based mostly on material gone over in small group and emphasized in lecture Focus on disease recognition and differential diagnosis, understanding of pathophysiology, pharmacology.
LAB 2: Cases 1-5
Case 1 Hx: A 35 year old Greek woman presents to the emergency room with abdominal pain. She is the mother of seven children, all in good health, and has had no previous medical problems. On physical examination, she is noted to be extremely pale. She appears to be short of breath with exertion. She denies dizziness or syncope.
Case 1 Px: Blood pressure is 130/85 with a pulse of 120. Her physical examination reveals pallor of the conjunctivae and buccal mucosa. Examination of the chest reveals a prominent impulse over the precordial area and a grade 2/6 systolic murmur at the base of the heart. The lungs are clear to auscultation. Her abdomen is soft, but there is tenderness in the mid-epigastric region. Her extremities are unremarkable.
Case 1 Labs: Hemoglobin 8.2 (normal 12-15), WBC of 9,000 (normal 5-10) and platelets of 500,000 (nl 150-450).
Case 1 Q1. What additional hematologic test would be useful in the initial evaluation of her anemia? Q2. What else would you want to know about her red blood cells?
Case 1 Q3. Why is it important to know how many children she has? What impact does breast feeding have on iron stores? Q4. What other questions would you like to ask about her history?
Case 1 Q5. What additional facet(s) of the physical exam would be useful in her evaluation?
Case 1 Q6. Discuss the significance of the following terms with your instructor: a) shock b) rales c) melena d) hematochezia e) flow murmur f) nail spooning g) ice pica h) orthostasis
Case 1 On further evaluation, the patient is found to have a duodenal ulcer on endoscopy. It is not actively bleeding Q7. Should she be given a transfusion? Q8. What are the indications for RBC transfusions? Q9. What additional laboratory tests would be helpful in defining the cause of her anemia? Q10. She has an elevated RDW at 14 (nl 10-12) Why is her RDW elevated? Q11. What should the MCV do after iron therapy is started?
Case 1 She is started on proton pump blockade therapy and her symptoms gradually disappear. The patient is started on oral iron therapy and initially does well with improvement in her Hemoglobin and Hct. However, those values plateau after 3 months, with Hgb of 11 g/dl and a Hct of 33%. The MCV remains low at 70 (nl 80-95)
Case 1 Q12. Give some potential explanations for the failure of her hemoglobin and hematocrit to rise to normal.
Case 1 The patient denies medical noncompliance. Her stools are now negative for occult blood. She gives a family history of Mediterranean anemia Q11. What test can be sent to detect thalassemia? What does it show if it is abnormal? What kind of thalassemia can it detect?
Case 2 Hx: A 19 year old African American woman presents with extreme pain in her back and legs. She has had a few episodes like this in the past, but this is the most severe pain that she has ever experienced. Her last menstrual cycle was 3 months ago.
Case 2 Px: Her physical examination was remarkable for a fever of 102.5 F, a rapid pulse and normal blood pressure. She had a systolic ejection murmur. Her abdomen had normal bowel sounds. She had costovertebral tenderness on the left and left flank pain.
Case 2 Her Hct was 18%, Hemoglobin 6 grams/dl, MCV 99. Her peripheral blood smear showed marked polychromasia and many sickled RBCs. Her WBC was 18,000 and her platelet count was 520K. Reticulocytes were 18%. Her urine had WBC that were too numerous to count and many bacteria. Her Urine HCG was positive.
Case 2 Q1. What is the molecular basis of this woman's disorder? Q2. What are some potential etiologies for this woman's painful crisis? Q3. What specific laboratory tests could you order to diagnose the cause of the anemia?
Case 2 Q4. How would you treat this patient? Q5. Would you give her a transfusion? Q6. Would you treat this woman with hydroxyurea? Q7. What factors go into the decision to treat with hydroxyurea?
Case 2 Q8. What therapy has been shown to be curative for this disorder? Q9. The woman's partner has sickle trait. What are the chances that the patient's baby will be born with sickle cell disease?
Case 2 The patient remains in the hospital. She has gotten a lot of IV fluids and pain medication overnight, and the next morning, her hemoglobin is 4.8 g/dl, and she is very sleepy and short of breath. Her oxygen saturation is only 75% on room air, and she has a new infiltrate on CXR. Q10. What complication has she developed? Q11. How should this be treated?
Case 3 Hx: A 16 y.o. girl presents to the emergency room with complaints of syncope. Her parents note that she has been very pale. She exercises vigorously, running at least 6-10 miles daily, but she has been complaining of becoming more winded. She worried that she was getting out of shape, so increased her distances. She passed out at the track this afternoon. She has been on a self-prescribed Ultra Atkins diet and has been eating only broiled fish and chicken breast with no carbs (including vegetables) at all.
Case 3 PEx: A pale, very thin girl. HR 110, BP normal. No nail spooning, 2/6 flow murmur, clear lungs, no peripheral edema. Breath smells like juicy fruit gum. She has lanugo hair and has no apparent body fat. Labs: Hgb 6.3 (nl 12-14), MCV 102, WBC 3.8 (nl 4.5- 10), platelets 120 (nl 150-450). Retic count low at 0.5%
Case 3 Q1: What additional laboratory data would you like to see?
Case 3 Further laboratory studies show a normal B12 level, but the folate level was 1.2 (nl 4-20). Q2. How can patients get folate deficient? Q3. What underlying disorder does this girl appear to have?
Case 4 A 25 y.o. African-American woman presents for evaluation of anemia found on routine physical examination. She has no medical problems and takes only birth control pills. She has never been pregnant. Her menses last 3 days and she uses no more than 6 pads daily on the heaviest day. There is no known family history of anemia in her parents. Physical examination (including pelvic exam) is normal
Case 4 Labs show a Hemoglobin of 10.2 (nl 12-14) MCV is 76. Absolute reticulocyte count is 48,000 (1%). Question 1. What other studies would you like to order?
Case 4 Iron studies are normal. Ferritin is normal. Hemoglobin electrophoresis is normal with a normal HbA2 level. Question 2. What is the most likely diagnosis?
Case 4 Question 3. What is the most likely genotype? Question 4. She marries a man with the same genotype as hers. What are the chances she will have a child with hydrops fetalis?
Case 5 A 25 y.o. woman from Laos presents for evaluation of anemia found on routine physical examination. She has no medical problems and takes only birth control pills. She has never been pregnant. Her menses last 3 days and she uses no more than 6 pads daily on the heaviest day. Her mother was told she was mildly anemic. Physical examination (including pelvic exam) is normal
Case 5 Labs show a Hemoglobin of 10.2 (nl 12-14) MCV is 76. Absolute reticulocyte count is 48,000 (1%). Iron studies and ferritin are normal. Hemoglobin electrophoresis is normal with a normal HbA2 level. Question 1. What is the most likely diagnosis and genotype?
Case 5 The patient marries an Asian man with the same laboratory studies as hers. Question 2: What is the likelihood of having a child with hydrops fetalis? Question 3: What if she married an African American man with the same genotype as the woman in the previous case? What would be the potential genotypes of their children?
LAB 3: Cases 6-11
Case 6 Hx: A 68 year old African American man with a history of poorly treated hypertension presents with the acute onset of inability to speak or move the right side of his body. Two weeks ago, he went to his doctor and got a refill of his normal BP meds since he had been out for 5 weeks. He has noted some blood in his urine for the past 3 days. PEx: aphasic man, unable to move right side. BP of 130/85. HR 85. No fever. Some bruises over his arms and legs.
Case 6 Labs: Hgb 8.5 (13-15), MCV 99, WBC nl, Plts 5 (150- 450) BUN 60 (nl 18-28), Cre 4.5 (nl 0.7-1.2) Q1. What other laboratory tests would be particularly helpful at this point? Q2. What radiological studies should be done at this point?
Case 6 The peripheral smear shows schistocytes. The T Bili is 3.0 (nl 0.3-1.2). The LDH is 5000 (nl 480-680). PT and PTT are normal. Q3. Does the patient have DIC? Why not? Q4. What does the patient have?
Case 6 Q5. Should the patient be given a platelet transfusion? Q6. How should the patient be treated?
Case 10 A 16 y.o. girl presents with fever, sore throat, sinus congestion, and abdominal pain in the left upper quadrant for the past 3 days. Pex shows T 102, HR 118, BP 110/65. Swollen red tonsils with a white exudate. Tender left maxillary sinus. Spleen tip is palpable in LUQ. No hepatomegaly. Slight jaundice noted. Lungs are clear.
Case 10 Labs show Hgb 7.5 (nl 12-14) WBC 13 (nl 5-10) Plts 350 (150-450). Q1. What else would you like to know about her labs?
Case 10 LDH 900 (nl 350-600) Tbili 2.1 (nl .1-1.0) Retic count 8% (absolute 200,000) Normal renal function MCV 99 (nl 80-100) Q2. Is this a disorder of red cell destruction or underproduction? Q3. What else do you want to know about her labs and her red cells?
Case 10 The MCHC is 37 (30-36) Q4. What else would you like to know about her red cells?
Case 10 Q5. What other lab studies would you order now? Q6. What else do you want to know about her history?
Case 10 The patient s 3 brothers, mother, and maternal grandfather have all had recurrent episodes of anemia, jaundice and splenomegaly. Many of them have had cholecystectomies before the age of 30 Q7. What is the most likely diagnosis and mode of inheritance? Q8. Should she have her spleen removed at this time?
Case 10 The patient is given antibiotics for her upper respiratory infection and recovers from her febrile illness. Her baseline hemoglobin is checked repeatedly over the next 2 years and is initally 108, falling over time to 9.2. She becomes more fatigued and cannot participate in basketball any more due to exertional dyspnea. Her spleen becomes progressively tender. She also develops recurrent RUQ pain. She and her parents wish to pursue splenectomy.
Case 10 Q9. What should be done for this patient prior to splenectomy?
Case 10 6 years later, the patient develops a sore throat and a fever to 102. Everyone in her family has been sick with the flu. Q10. She calls her PCPs office. What should she be told to do?
Case 10 She takes the antibiotics she has at home but still does not feel well. She goes to her local ER where she rapidly develops cough, chest pain, pneumonia, hypotension respiratory failure and requires intubation, mechanical ventilation, and blood pressure support with pressor agents. Q11. What rare complication has she developed?
Case 10. Review the Direct Coomb s test and the osmotic fragility test with your instructor.