Quality Improvement Methods and Domains for Better Healthcare Outcomes
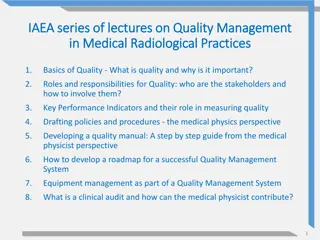
This content introduces Quality Improvement (QI) processes, methods, and domains essential for enhancing healthcare outcomes. It covers the significance of continuous efforts by healthcare professionals, patients, researchers, and other stakeholders to improve patient outcomes, system performance, and professional development. Various frameworks such as Deming's Profound Knowledge, Microsystems approach, and Theory to Measurement systems are discussed to emphasize the importance of quality improvement in healthcare settings.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Chapter 1 Introducing Quality Improvement @SAFE_QI
Chapter 1: Introducing Quality Improvement S.A.F.E uses quality improvement (QI) as a core methodology. This chapter will focus on understand QI methods. @SAFE_QI
Resources Plan Do Study Act Checklist and Log Driver Diagram Measurement Plan Stakeholder Map @SAFE_QI
Domains of Quality CROSSING THE QUALITY CHASM: A New Health System for the 21st Century INSTITUTE OF MEDICINE NATIONAL ACADEMY PRESS Person centred Safe Effective Equitable Timely Efficient Do we harm patients? Do we give the right treatment every time all the time? Are the services and outcomes equal for all Is there good access? Do we get value? What matters to me @SAFE_QI
What is Quality Improvement? Quality Improvement can be defined as the: combined and unceasing efforts of everyone healthcare professionals, patients and their families, researchers, payers, planners and educators to make the changes that will lead to better patient outcomes (health), better system performance (care) and better professional development Batalden and Davidoff @SAFE_QI
Demings Profound Knowledge System where you work Variation in the system Psychology - the people Theory of knowledge @SAFE_QI Deming
Microsystems Strong Leadership Great Organizational Support Focus on Staff (Professionals) Leadership Staff Education and Training of Staff Interdependence of Care Team Performance Result Focused Process Improvement Focused Performance Patients Patient-Centered (Patient Focus) Community and Market Focus Information & Information Technology Orientation Reference Nelson et al 2008 @SAFE_QI Reference Dartmouth
Theory to method to measurement Systems Variation Theory Theory of knowledge Method Psychology Measure @SAFE_QI
The Model for Improvement Plan Do What changes can we make that will result in improvement? How will we know if the change is improvement? Study Act What are we trying to accomplish? @SAFE_QI
Change in the Microsystem The individual Network district regional Clinical skills Self management Personal development Whole patient journey Across organisations Macro organisation Clinical Micro system Connects meso systems and micro systems Individual team and patient Where improvement takes place Meso system Supports micro system @SAFE_QI
5 Ps to Assess Improvement in a Microsystem Purpose - Our aim and mission. Patients - Our reason for doing our work. People - Our staff who take care of patients. Processes - Our interrelated process that make up the micro system. Patterns The way we work and measure what we do (Measurements, Data, Run Charts) @SAFE_QI Reference Dartmouth
Model for Improvement What change can we make that will result in an improvement ? The PDSA Cycle @SAFE_QI Langley Nolan et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance, 2nd Edition April 2009, Jossey-Bass P 89
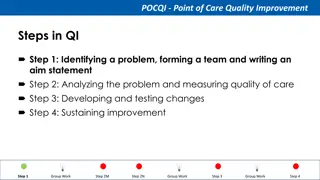
Where to start? Implement changes Test changes Establish measures Set aims Define area for change @SAFE_QI
S.A.F.E Driver Diagram Outcomes Primary Drivers Secondary Drivers To reduce avoidable error and harm to acutely sick children through the introduction of a culture based on safety. This will be demonstrated by: A 50% reduction in unsafe transfers. 95% compliance at each site with the locally parameters for huddles. Increased understanding in clinical teams of the concepts of situation anticipation, containment and reliability. Increased awareness of local safety through Sexton Safety Survey scores. Introduction of the huddle intervention and development of scripts appropriate for local settings. Introduction and reinforcement (where appropriate) of the use of SBAR. Introduction and development of other appropriate tools and interventions. Development of a flexible intervention model to improve situation awareness. Improved Situation Awareness agreed Educating teams in concepts of situation awareness, anticipation, containment and reliability. Introduction of both the Sexton Safety Attitudes Survey (comparative) and MaPSaf (developmental) tools as mechanisms for assessing safety attitudes. Developing an open approach to working as clinical teams Developing a culture based on safety awareness, improved Attitudes Introducing patients, parents and carers are key components of the team. Engaging patients, parents and carers in the development of local projects. Introduction of PREMS and a patient/parent safety awareness survey. Introduction and development of tools, techniques and interventions with a patient/parent engagement focus. Improved experience scores and awareness of safety from patients, parents and carers through the Safety Awareness survey. Improved engagement with patients and their parents and carers in delivering care recognised as being safe. PREMS and @SAFE_QI
PDSA Paper Aeroplane Activity Quality Improvement in Action Aim: Design a paper plan that will fly the furthest distance Think of the areas you need to consider: Design Construction Measurement Run your tests a few times: What are you learning? How will you factor your learning into the next test? Did your change result in improvement ? @SAFE_QI
Spreading Change through Collaboration The success of S.A.F.E has been in establishing, encouraging, and supporting networks to share learning, experiences, and ultimately, change. What networks can you engage with to help spread your improvements? @SAFE_QI