Proposed Model for Medicalized First-Line Health Services in Kigali
The proposed model for the development of medicalized first-line health services in Kigali, Rwanda, addresses challenges in access to care, urban health issues, and the concept of first-line health units. It aims to provide comprehensive healthcare services to the growing population of Kigali, emphasizing collaboration between public and private healthcare facilities.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
A proposed Model for the development of medicalized first line health services for the City of Kigali in Rwanda: striving for excellence BE-CAUSE HEALTH ANNUAL CONFERENCE, BRUSSELS 15THTO 16THOCTOBER 2019 TAKING THE URBAN TURN KHN
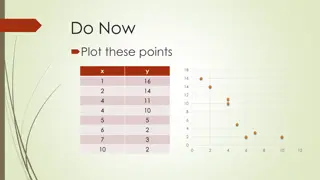
URBAN HEALTH CHALLENGES ACCESS TO CARE: Geographical: Overloaded health facilities Financial: Private facilities Uncovered needs in eye care, dental care, physiotherapy, palliative care, chronic diseases care Mental Health City of Kigali population growth 1962-2040 (proj) EXPONENTIAL POPULATION GROWTH 4500000 4200000.0 4000000 3500000 3000000 Population 2500000 2000000 2000000.0 1500000 1133000.0 1000000 765000.0 500000 115000.0 235000.0 0 6000.0 1962 1978 1991 2002 2012 2027 2040 Years EPIDEMIOLOGIC TRANSITION: High Blood pressure Diabetes Overweight Alcohol and smoking HEALTH FACILITIES 4 referral hospitals 4 District Hospitals 5 Private hospitals 200 Private facilities, 59 Public and 22 FBO 1 MD / 2,120 inhabitants 1 bed / 417 inhabitants 1 ambulance for 50,000 NUMEROUS ACTORS: City of Kigali and administrative districts, DHMT, DHU Public Health Facilities Private Health facilities Ministry of Health and RBC Civil Society Enabel URBAN CONTEXT Water and sanitation Waste management pollution Road accidents Mental Health
CONCEPT OF FIRST LINE HEALTH UNIT (FLHU) One management unit PFP NGO PFP Entry point: PFP, NGO, HP Medicalized Day care health centre Day care health centre Medicalized HP Mentored by: Health Center (public finality but mix public and private actors) HP Urban district hospital HP NGO Optimal Division of labor Medicalized Medicalized Day care health centre Day care health centre NGO HP PFP HP: Health Post PF: Private For Profit NGO Non Governmental Organization
City coverage plan Centre de sant Centre de sant HP HP H pital de district urbain HP Centre de sant Centre de sant Centre de sant Centre de sant HP HP HP H pital de district urbain HP Centre de sant Centre de sant Centre de sant Centre de sant HP HP HP H pital de district urbain HP Centre de sant Centre de sant HP Centre de sant Centre de sant HP HP Centre de sant Centre de sant H pital de district urbain HP HP HP Centre de sant Centre de sant H pital de district urbain HP HP Centre de sant Centre de sant Centre de sant Centre de sant HP HP HP H pital de district urbain HP Centre de sant Centre de sant HP
Medicalized first line health unit model for CoK UHC: MD, Nurses, admin staff HP: A1 Nurse with private MD Note: MD might work at both levels
Package of Care at Urban Health Center Revalidation services handicap care Mental Health, epilepsy (diagnosis and follow up) Diagnostic Services (Labo, US) NCD: Eye clinic (incl. Production of glasses) Follow-up clinics for STI/HIV Hypertension, diabetes, CVA MNCH Services (ANC, Under-Five cl, Delivery, etc.) Dental care Minor surgery Administration and finance
Ongoing pending questions HR: availability of MD, tasks of (private) MD Division of labor within the unit: ? Concentrate promotional and preventive services at HP level? Financial sustainability: How to cover the costs of MD while maintaining social protection Consider various funding sources: health insurance, government subsidies, Out-of- Pocket payments, contracting for preventive services, conditionalities, separate fee system for specific users (i.e. external visitors, tourists, ), evening or weekend on call system at higher fee, etc.; Scale up: estimated need of 30-40 FLHU based on norm of 30-50,000 inhabitants per center Next steps: continue the debate, develop coverage plan, involve private sector, analyze the costs and financial modalities, define model of contracting, e-patient filing, develop budget proposal and involve other partners
UPGRADED (MEDICALIZED) HEALTH CENTER- GATENGA Thank you Murakoze cyane