Overview of Cohort Studies in Epidemiology
Cohort studies are a type of observational study where a group of healthy subjects is followed over time to investigate relationships between exposures and outcomes. They provide valuable insights into disease development and risk factors, offering advantages like assessing multiple exposures and endpoints. However, cohort studies also have limitations such as being unsuitable for rare diseases, requiring long follow-up durations, and facing possible changes in exposure and disease diagnoses over time. Examples like the Women's Lifestyle and Health Cohort Study further illustrate the application of cohort studies in epidemiological research.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Epidemiological Studies Part 2 Nina Gunnes October 8, 2020 10/08/2020 Lecture 4 1
Types of epidemiological studies Two main types of epidemiological studies Observational studies Experimental studies Four types of observational studies Ecological studies Cross-sectional studies Case-control studies Cohort studies 10/08/2020 Lecture 4 2
Cohort studies Based on a group of healthy subjects (cohort) followed over time Prospective (moving forward in time: present future) Several advantages Easy to understand Several exposures and endpoints possible Changes in exposure measured along the way as the study progresses Estimation of incidence rate possible Exposure measured before disease has occurred recall bias avoided 10/08/2020 Lecture 4 3
Cohort studies, cont. Some disadvantages Unsuited for very rare diseases Long duration of follow-up may be required May be expensive Exposure and disease diagnoses may change over time Exposed subjects may receive closer follow-up Susceptible to withdrawal and loss to follow-up Incidence rate ratio (IRR) as a common effect measure 10/08/2020 Lecture 4 4
Cohort studies, cont. Exposed Unexposed ?? ?0 Number of diseased (new cases) ?? ?0 Number of person-years ???= ???? ??0= ?0?0 Incidence rate Point estimate of IRR: ??? =??? ???? ?0?0 ??0= 1 ??+ 1 ??+ 95% CI of IRR: ??? ? 1.96 1 ?0,??? ?1.96 1 ?0 10/08/2020 Lecture 4 5
Example 10.8 in Aalen et al. (2006) 10/08/2020 Lecture 4 6
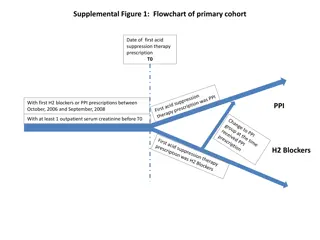
Example 10.8 in Aalen et al. (2006), cont. The Women s Lifestyle and Health Cohort Study (1991/92 1999) Norwegian-Swedish study of risk factors for malignant melanoma More than 100,000 included women aged 30 50 years Women followed to the first occurring event after inclusion Emigration Death (whatever the cause) Diagnosis of malignant melanoma End of study (December 31, 1999) 10/08/2020 Lecture 4 7
Example 10.8 in Aalen et al. (2006), cont. Questionnaire on, among other things, sun exposure Defining two exposure groups Unexposed: never sunburned at age 10 19 years Exposed: sunburned two or more times per year at age 10 19 years 22,747 unexposed women 22 cases of malignant melanoma 21,273 exposed women 55 cases of malignant melanoma 10/08/2020 Lecture 4 8
Example 10.8 in Aalen et al. (2006), cont. Sunburn at the age of 10 19 years Never 2 times per year Number of cases of malignant melanoma 22 55 Number of person-years 177,537 173,216 Incidence rate 0.000124 0.000318 10/08/2020 Lecture 4 9
Example 10.8 in Aalen et al. (2006), cont. Calculating incidence rate ratio with 95% confidence interval Crude ??? = Using Poisson regression to adjust for age, residence, and hair color Adjusted ??? = 2.42 95% CI:1.46 4.02 Incidence rate almost two and a half times higher among the exposed IRR interpreted as a relative risk (RR) Approximately same result obtained by using Cox regression 55 173,216 22 177,537= 2.56 95% CI:1.56 4.20 10/08/2020 Lecture 4 10
Observational studies Table 10.1 in Aalen et al. (2006) 10/08/2020 Lecture 4 11
Experimental studies Exploring the effect of various interventions Treatments Drugs Often based on findings from observational studies Usually randomized Subjects randomly allocated to an intervention (i.e., grouped by chance) Much in common with controlled clinical trials 10/08/2020 Lecture 4 12
Example 10.9 in Aalen et al. (2006) 10/08/2020 Lecture 4 13
Example 10.9 in Aalen et al. (2006), cont. Vitamin E and beta-carotene associated with reduced risk of cancer High intake through diet and high blood levels of nutrients Findings from observational studies (especially lung cancer) Alpha-Tocopherol, Beta-Carotene Cancer Prevention Trial Randomized placebo-controlled trial conducted in 1985 1993 National Public Health Institute of Finland and US National Cancer Institute Exploring effect of alpha-tocopherol and beta-carotene supplements Reducing the risk of cancer and cardiovascular disease? 10/08/2020 Lecture 4 14
Example 10.9 in Aalen et al. (2006), cont. Including 29,133 male smokers aged 50 69 years High-risk group new cases of lung cancer within reasonable time Participants randomized into four different treatment groups Alpha-tocopherol (a form of vitamin E) Beta-carotene (a precursor of vitamin A) Both alpha-tocopherol and beta-carotene Placebo 876 new cases of lung cancer by the end of April 1993 10/08/2020 Lecture 4 15
Example 10.9 in Aalen et al. (2006), cont. Higher incidence rate among receivers of beta-carotene Change of 18% (95% CI: [3%, 36%]) as compared to non-receivers No reduction in incidence rate among receivers of alpha-tocopherol Change of -2% (95% CI: [-14%, 12%]) as compared to non-receivers Surprising results Beta-carotene not seeming to protect against lung cancer Smokers should be avoiding high doses of beta-carotene 10/08/2020 Lecture 4 16
Sources of error Three main sources of error in epidemiological studies Information bias Selection bias Confounding Information bias due to erroneous registration of exposure or disease Some information bias in almost all epidemiological studies Nearly impossible to register exposure without measurement error Important to minimize measurement error and avoid systematic errors 10/08/2020 Lecture 4 17
Sources of error, cont. Selection bias due to non-representative study sample Study sample not representative of the study population Bias in effect measures (e.g., IRR or OR) Low participation or loss to follow-up in cohort studies Controls not obtained from base population of cases in case-control studies Confounding due to variable affecting both exposure and outcome Common cause of exposure and outcome 10/08/2020 Lecture 4 18
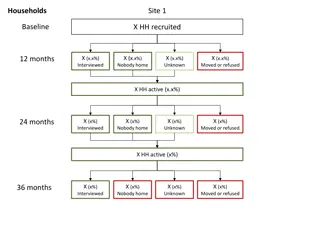
Validity Reflecting whether or not findings are reliable and generalizable Two types Internal validity External validity Internal validity relating to the design and conduct of the study Based on no substantial errors (information/selection bias, confounding) High when no errors in obtaining, analyzing, and interpreting data Prerequisite for external validity 10/08/2020 Lecture 4 19
Validity, cont. External validity relating to the generalizability of the findings Validity of applying findings to other contexts or other people Findings generalizable for subjects outside of the study population Figure 1 in Patino & Ferreira (2018). 10/08/2020 Lecture 4 20
References Aalen OO, Frigessi A, Moger TA, Scheel I, Skovlund E, Veier d MB. 2006. Statistiske metoder i medisin og helsefag. Oslo: Gyldendal akademisk. Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med. 1994;330(15):1029-1035. doi:10.1056/NEJM199404143301501. Patino CM & Ferreira JC. (2018). Internal and external validity: can you apply research study results to your patients?. Jornal Brasileiro de Pneumologia, 44(3), 183. https://dx.doi.org/10.1590/s1806-37562018000000164. Veier d MB, Weiderpass E, Th rn M, et al. A prospective study of pigmentation, sun exposure, and risk of cutaneous malignant melanoma in women. J Natl Cancer Inst. 2003;95(20):1530-1538. doi:10.1093/jnci/djg075. 10/08/2020 Lecture 4 21