Novel Insights into Somatic-Germline Variants
Workshop organized by Dr. Katie Snape aims to review data on likelihood of somatically identified variants in the germline, address challenges in referring patients for genetic testing, and define clinical pathways for consent and testing in cancer genetics. Survey results reflect limited expertise in this complex area among oncologists and geneticists.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Introduction and Survey Results Dr Katie Snape, Consultant Cancer Geneticist UKCGG and St George s University Hospitals NHS Foundation Trust K.snape@nhs.net
Background Increasing use of somatic testing in cancer tissue Use of both somatic panels and WGS (with paired germline) in test directory Increasing number of referrals into clinical genetics on basis of somatic data wondering if variants could be present in the germline Increasing number of private and DTC referrals into clinical genetics
Current Situation No clear guidance on Who is/should be eligible for referral to clinical genetics on the basis of a somatic test What the likelihood of finding a germline variant is for an identified somatic variant In associated tumour types In non associated tumour types How consent should operate for somatic testing where germline information may be identified How these novel pathways will impact on resourcing in clinical genetics
Aims of todays workshop Review novel data which gives insight into the likelihood of a somatically identified variant also being present in the germline Understand current and future policy on somatic/germline cancer gene testing from NHSE Obtain consensus (as much as possible!) on what/who should and should not be referred from oncology to clinical genetics for further assessment/testing Define/debate the novel clinical referral pathways which need to be implemented including where and how consent for germline testing should be undertaken Present our outcomes as an expert working group of clinical scientists, oncologists, pathologists, clinical geneticists and genetic counsellors
Survey Responses 23 respondents Multiple emails saying people did not feel they have enough expertise to complete the survey so were non responders At least two respondents stated they didn t feel they knew enough to answer specific questions Conclusion: difficult and complex area, with limited expertise amongst oncologists and geneticists
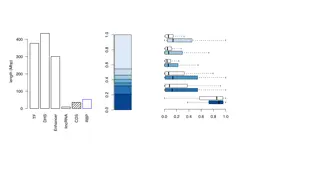
Tumour type specific age cut off Variant allele frequency is >40% in the tumour tissue Variant is within a cancer susceptibility gene with NO established constitutional (germline) association with the cancer type it was identified in Variant is within a cancer susceptibility gene with an established constitutional (germline) association with the cancer type it was identified in STRONGLY AGREE AGREE Variant is within a cancer susceptibility gene for which diagnostic constitutional (germline) testing is available currently NEUTRAL DISAGREE Variant is predicted to result in loss of function in a gene where this is established disease mechanism e.g. stop gained, frameshifting truncating variants in tumour suppressor genes STRONGLY DISAGREE Variant is predicted to result in loss of function in a gene where this is established disease mechanism e.g. stop gained, frameshifting truncating variants in tumour suppressor genes Variant is reported as pathogenic constitutional (germline) Class 4 or Class 5 with 2 or more stars on Clin Var Variant is ACMG constitutional (germline) Class 4 or Class 5 by clinical consensus 0.00% 10.00%20.00%30.00%40.00%50.00%60.00%70.00%80.00%90.00%
Take home messages Divided on whether the following should be included Age cut offs for tumour types No established germline association with cancer type Variant allele frequency of 40%
Take home messages Divided on whether the following should be included Age cut offs for tumour types No established germline association with cancer type Variant allele frequency of 40%
Take home messages Full or almost full agreement to include Variant is in gene(s) for which diagnostic germline testing is available Established germline association with cancer type Variant is class 4/5 by clinical consensus (e.g. C- VIG), 2* on Clinvar or LoF variant where that is known pathogenic mechanism of gene
Comments on additional inclusion criteria Assimilate alongside other molecular/pathological data (e.g. IHC/mutational signatures) Clinical actionability e.g. Lower threshold for testing if affects clinical trial eligibility and higher threshold if no clear change in clinical management for patient/relatives Likelihood of germline mutation being present if identified somatically
Genes in breast cancer Breast cancer 25 20 15 Breast cancer 10 5 0 TP53 BRCA1 BRCA2 PALB2 MLH1 MSH2 MSH6 PMS2 APC OTHER (SEE BELOW) Other: PTEN/STK11/CHEK2/ATM/CDH1 (lobular)
Genes in serous ovarian cancer Serous ovarian cancer 25 20 15 Serous ovarian cancer 10 5 0 TP53 BRCA1 BRCA2 PALB2 MLH1 MSH2 MSH6 PMS2 APC OTHER (SEE BELOW) Other: RAD51C, RAD51D, BRIP1
Genes in non-serous ovarian cancer Non serous ovarian cancer 25 20 15 Non serous ovarian cancer 10 5 0 TP53 BRCA1 BRCA2 PALB2 MLH1 MSH2 MSH6 PMS2 APC OTHER (SEE BELOW) Other: RAD51C, RAD51D, BRIP1
Genes in colorectal cancer Colorectal cancer 25 20 15 Colorectal cancer 10 5 0 TP53 BRCA1 BRCA2 PALB2 MLH1 MSH2 MSH6 PMS2 APC OTHER (SEE BELOW) Other: polyp panel genes
Genes in lung cancer Lung cancer 9 8 7 6 5 Lung cancer 4 3 2 1 0 TP53 BRCA1 BRCA2 PALB2 MLH1 MSH2 MSH6 PMS2 APC OTHER (SEE BELOW)
Themes of gene eligibility Preference for known CPGs in associated tumour types Multiple suggestions to include all CPGs for associated tumours But significant proportion suggesting CPGs in non associated tumour types Opting out of some tumour types which people felt less comfortable with
?Age cut off 1200.00% 1000.00% TP53 800.00% BRCA1 BRCA2 PALB2 600.00% MLH1 MSH2 MSH6 400.00% PMS2 APC OTHER (PLEASE COMMENT BELOW) 200.00% 0.00% <30 <40 <50 <60 <70 No age cut off
Comments on age cut off Tumour dependent E.g. Different age cut offs for breast and prostate cancer with BRCA Becomes complicated... Age not only factor also family history, histology etc.
Referrals Vast majority currently managing on case by case basis as small numbers Would be helpful to have agreed national standardised criteria for accepting/rejecting referrals for testing or further assessment
Other comments Haem-onc samples saliva? Paired germline-somatic testing upfront would help resolve many of these issues Need funding/staff/resources as well as clinical pathways What is currently deliverable? What extra resources do we need to implement these workflows?
Aims of todays workshop Review novel data which gives insight into the likelihood of a somatically identified variant also being present in the germline Understand current and future policy on somatic/germline cancer gene testing from NHSE Obtain consensus (as much as possible!) on what/who should and should not be referred from oncology to clinical genetics for further assessment/testing Define/debate the novel clinical referral pathways which need to be implemented including where and how consent for germline testing should be undertaken Present our outcomes as an expert working group of clinical scientists, oncologists, pathologists, clinical geneticists and genetic counsellors