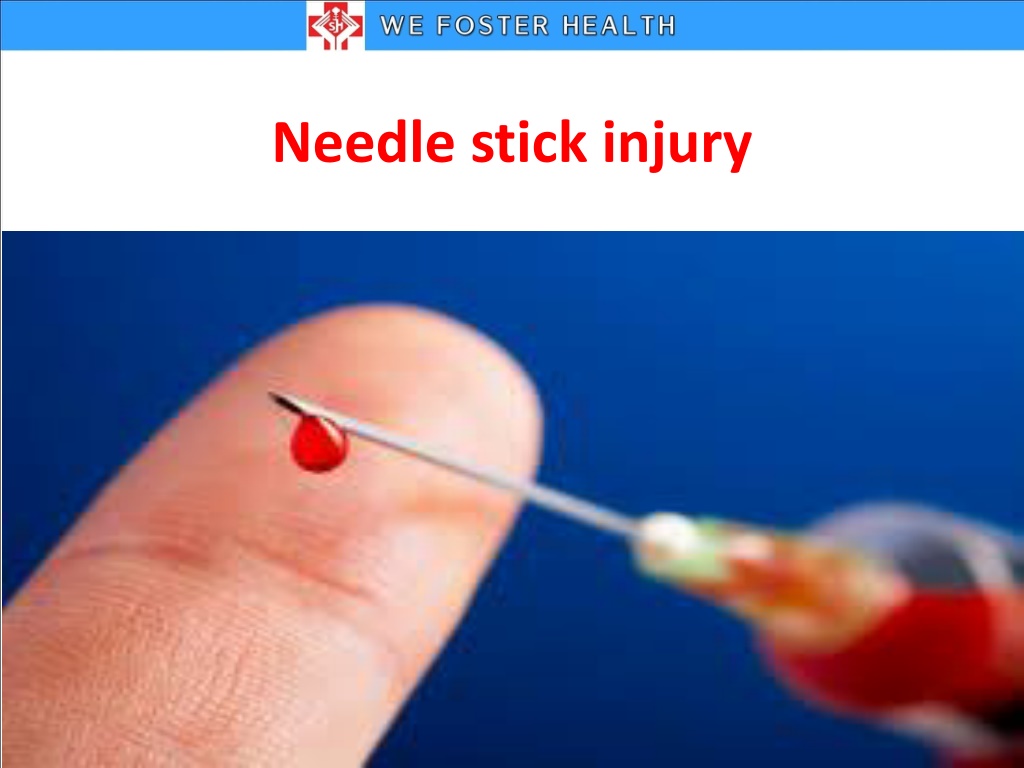
Needle Stick Injuries and Prevention
Needle stick injuries are percutaneous piercing wounds caused by needles or other sharp instruments. They pose significant risks, including exposure to blood-borne diseases. Health-care workers are particularly vulnerable, with millions experiencing such injuries annually. Proper training, safe practices, and prompt post-exposure protocols are crucial in preventing and managing needle stick injuries.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
DEFINITION A needle stick injury is a percutaneous piercing wound typically set by a needle point, but possibly by other sharp instrument or objects also.
WHO REPORTS ON NEEDLE STICK INJURIES WHO reports in the World Health Report2002, that of the 35 million health-care workers, 2 million experience percutaneous exposure to infectious diseases each year. It further notes that 37.6% of Hepatitis B, 39% of Hepatitis C and 4.4% of HIV/AIDS in Health-Care Workers around the world are due to needle stick injuries.
WHEN IT CAN HAPPEN Blood collection Recapping Surgery Discarding Segregation of waste Mishandling of sharps
WHO IS AT RISK? Doctors Nursing Staff Emergency Care Providers Labor & delivery room personnel Surgeons and operation theatre staff Lab Technicians Dentists Housekeeping staff/ mortuary staff / Waste Handlers
WHAT CAN HAPPEN? Needle stick injury may lead to . Blood-borne diseases like, HIV-AIDS Hep-B Hep-C
Our practices leading to NSI Recapping needles. Performing activities involving needles and sharps in a hurry. Handling and passing needles or sharp after use. Failing to dispose of used needles properly in puncture resistant sharps containers at the correct time. Poor healthcare waste management practices. Ignoring Universal Work Precautions.
POST EXPOSURE Don t PANIC !!! Do not squeeze (negative pressure) Wash with soap and water immediately Report it, consult doctor and inform infection control nurse. Follow the post exposure prophylaxis regime(PEP).
NEEDLE STICK INJURY (NSI)/EXPOSURE TO BLOOD &BODY FLUID (BBF) MANAGEMENT ALGORITHM HCW sustaining needle stick injury/splash For NSI-wash the area with soap & water. For splash ,flush the mucus membrane with plenty of water/saline Inform the ICN/ward incharge/ nursing superintendent as soon as possible HCW initiates incident form Case to be reviewed by CMO/Physician as per the guidelines for the treatment modality as soon as possible & maximum within 24 hours Treatment to be provided as per the guidelines follows. Post exposure prophylaxis
HOW TO DISPOSE SHARPS Workers should place needles in wide-mouth puncture proof containers. Locate disposal containers specifically where needles are used to make safe disposal possible without recapping. Replace the containers before they are completely filled. Make sure they are sealed, collected and disposed of in accordance with local regulations for biomedical waste.
TAKE HOME MESSAGES Always follow right practices Actively educate new personnel Report NSI immediately to ward incharge, ICN. Remember!!! confidentiality is always maintained Always follow up an injury Try to minimize use of needles
LETS HELP EACH OTHER TO ELIMINATE RISK OF NEEDLE STICK INJURY
PERSONAL PROTECTIVE EQUIPMENTS
DEFINITION Specialized clothing or equipment worn by an employee for protection against infectious materials
TYPES OF PPE Gloves Protect hands Gowns/aprons Protect skin and clothing Masks Protect mouth/nose Goggles Protect eyes Face shields Protect face, mouth, nose, and eyes Boots/shoe cover Protect feet Cap Prevent from hair falls
Principles for use of PPE PPE should be chosen according to the risk of exposure. Avoid any contact between contaminated PPE and surfaces or people outside the patient care area. Do not share PPE. Change PPE completely and wash hands each time you leave a patient to attend to another patient or another duty.
GLOVES Clean gloves: Wear Clean gloves while doing environmental cleaning and clean procedures When touching Blood, body fluids, secretions, When to use excretions or mucus membranes. While caring patient with skin infection. In contact precautions like MRSA, MDR, VRE etc Sterile gloves : when doing sterile procedures
GLOVES Where to keep Gloves should be kept in nurses station and in front of the isolation room. Whom to use Health care worker as per the need arises When to dispose Remove gloves and wash hands immediately after use and before attending to another patient Where to dispose Yellow cover
GOWN Wear gown while caring the patient with contact precautions like MRSA, diarrheal disease , open wounds etc. Gown should be worn when there is a risk When to use that clothing may become contaminated with blood, secretions, and excretions.
GOWN Gown should be kept in nurses station and in Where to keep front of the isolation room. Whom to be use Health care worker as per the need arises Remove the gown before leaving the patient care When to dispose area or at the nurses station. Where to dispose yellow bin
MASK Wear surgical mask when attending patients with contact, droplet and airborne precautions N95 mask for TB patients. High risk areas such as OT, ICU, and Emergency when to use dept. Risk to generate splashes of blood, body fluids, secretions or excretions. In reverse isolation (Neutropenia) While caring immunocomprised patients
MASK Where to keep Keep at the nurse s station in wards and at the entrance of the OT , ICU and isolation room. Health care worker must use in OT, ICU and emergency Whom to be use department and as per the need arises in the ward area. Doctors and OP girls in the medical OP, Paediatric OP (in epidemic Season), Pulmonology OP, Dental OP and ENT OP When to dispose Mask should be changed when they become soiled or wet. Dispose the mask at the doorway or immediately outside the patient room Where to dispose yellow bin
CAP Wear cap in areas like OT and ICU. when to use Wear cap where there is likelihood that patient s blood, body fluids, secretions or excretions may splash, spill or leak into hair
CAP Cap should be kept in nurses station in wards and at the Where to keep entrance of the OT and ICU; also in front of the isolation Health care worker must use in OT, ICU and as per the need Whom to be use arises in the ward area. Cap should be disposed after spillage exposure or when it When to dispose becomes wet. Otherwise it can be used continuously till the end of one shift. Where to dispose Yellow bin
Sequence for Donning PPE Gown first Mask or respirator Goggles or face shield Gloves
Sequence for Removing PPE Gloves Face shield or goggles Gown Mask or respirator
Final Thoughts for you.. PPE is available to protect you from exposure to infectious agents in the healthcare workplace. Know what type of PPE is necessary for the duties you perform and use it correctly.
Disinfectant Equipment Ambu bag , Airway, ET tube, ET Stillet, Trachesotomy tube Fibro optic cameras Cautery cables, ETO ICD tube, lap scissors , lap grasper, lap suction tip, lap reducer catheter introducer, biopsy forceps, connector of irrigation Pessary ventilator filters, test lung bag O2 mask and tubing , Nebulization set (OPD),
Disinfectant Equipment Thermometer BP apparatus Stethoscope Computer keyboard SPIRIT Telephone Pulse oximeter, Bed side monitors Syringe pump Medicine container
Disinfectant Equipment Mattress Pillow Mackintosh Bedside table Hypochlorite (10 ML Patient cot IN 1L OF WATER) bystander cot Patient chair Wheel chair Patient trolley
Disinfectant equipments Endoscope Colonoscope sigmoidoscope Esophagoscope CIDEX Laryngoscopes Arthroscope Laparoscope Scissors Needle holder BP handle thumb forceps
Disinfectant Equipment Decontaminating blood and body fluid spills Disposal of needle Bed Pan Urinal Sputum mug Hypochlorite Kidney tray Toilet bowls