MRSA Infections: Causes and Impacts
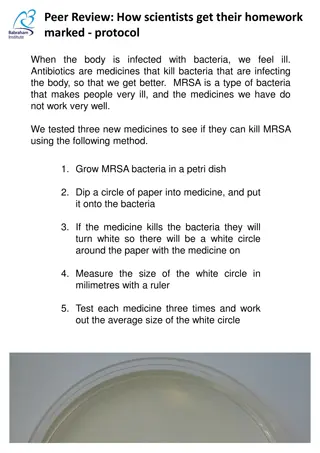
Staphylococcus aureus, commonly known as Staph, can lead to Methicillin-Resistant Staph (MRSA) infections, both in the community and healthcare settings. MRSA outbreaks are often detected in various populations like sports participants, inmates, and military recruits. The types of MRSA infections vary, with skin/soft tissue being the most common. Invasive MRSA infections have resulted in significant impacts, with older persons, blacks, and males being most affected. The prevalence of MRSA is substantial, as it can be community-associated and healthcare-associated, affecting both healthy individuals and those with weakened immune systems. Proper understanding and prevention measures are crucial in combating MRSA infections.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
MRSA MRSA
What Is MRSA? Staphylococcus aureus (Staph) Common cause of infection in the community Methicillin-Resistant Staph (MRSA) Increasingly important cause of health care associated infections since 1970s In 1990s, emerged as cause of infection in the community
How do you get MRSA? Outbreaks of MRSA in the Community Often first detected as abscesses or spider bites Various Settings Sports participants Inmates Military recruits Daycare attendees Hurricane evacuees in shelters
Types Disease Syndrome (%) Skin/soft tissue 1,266 (77%) Wound (Traumatic) 157 (10%) Urinary Tract Infection 64 (4%) Sinusitis 61 (4%) Bacteremia 43 (3%) Pneumonia 31 (2%)
People Affected The estimated number of people developing a serious MRSA infection (i.e., invasive) in 2005 was about 94,360 Approximately 18,650 persons died during a hospital stay related to these serious MRSA infections Overall rates of disease were consistently highest among older persons (age >65), blacks, and males
Most Invasive MRSA Infections are Healthcare-Associated Community-Associated 14% Healthcare-Associated 86%
Staphylococcus aureus (staph) Bacteria commonly carried on the skin or in the nose of healthy people Bacteria may be present without causing infection 25% to 30% of the population is colonized Staph bacteria are some of the most common causes of skin infections in the U.S. Pimples and boils Bloodstream infections Pneumonia
Methicillin-resistant Staphylococcus aureus (MRSA) Staph bacteria that are resistant to certain antibiotics Methicillin Penicillin Amoxicillin Occur most frequently among persons in hospitals and healthcare facilities who have weakened immune systems May also cause illness in persons outside of hospitals and healthcare facilities community-associated if acquired by a person who has not been recently (within the past year) hospitalized or has not had an invasive procedure
What does a MRSA infection look like? MRSA can cause skin infections that may look like a pimple or boil Can be red, swollen, painful or have pus or other drainage Skin monitoring important for persons returning from hospitals People with skin infections should see a healthcare provider More serious infections may cause pneumonia, bloodstream infections or surgical wound infections
Risk Factors Clusters of MRSA skin infections have been investigated among: Athletes Military recruits Men who have sex with men Prisoners Factors associated with the spread of MRSA skin infections include: Close skin-to-skin contact Crowded living conditions Cuts or abrasions of the skin Contaminated items and surfaces Poor hygiene
Prevention Keep hands clean by washing thoroughly with soap and water or using an alcohol-based hand sanitizer Keep cuts and scrapes clean and covered with a bandage until healed Avoid contact with other people s wounds or bandages Avoid sharing personal items such as towels or razors If skin is dry, use a moisturizer to prevent cracking.
Treatment Most MRSA infections are treatable with antibiotics Take all doses, even if the infection is getting better, unless your doctor tells you otherwise Do not share antibiotics with other people Some staph infections may be treated by draining the abscess or boil and may not require antibiotics Drainage should only be done by a healthcare provider If the infection does not get better after a few days, contact your healthcare provider again If other people you know or live with get the same infection, tell them to go to their healthcare provider
Control If MRSA is identified, follow these steps Cover the wound http://t2.gstatic.com/images?q=tbn:Q3qGXTcTgR9yKM:http://home.netscape.ca/~stubby/img/SuperBug.jpg Pus from infected wounds can contain staph and MRSA, so keeping the infection covered will help prevent the spread to others Keep wounds that are draining or have pus covered with clean, dry bandages Follow your healthcare provider s instructions on proper care of the wound Bandages or tape can be discarded with the regular trash
http://t3.gstatic.com/images?q=tbn:YWcbQxMnfksWSM:http://www.altham.com/assets/images/Hospital-Wash-Hands-Cartoon.jpghttp://t3.gstatic.com/images?q=tbn:YWcbQxMnfksWSM:http://www.altham.com/assets/images/Hospital-Wash-Hands-Cartoon.jpg Control Clean your hands Persons with MRSA, and others in close contact, should wash hands frequently with soap and warm water or use an alcohol-based hand sanitizer Especially important after changing the bandage or touching the infected wound Do not share personal items such as towels, washcloths, razors, clothing, or athletic equipment that may have had contact with the infected wound or bandage Wash sheets, towels, and clothes that become soiled with water and laundry detergent Drying clothes in a hot dryer, rather than air-drying, also helps kill bacteria in clothes
Should Students with MRSA Skin Infections Be Excluded From Attending School? Unless directed by a physician, students with MRSA infections should not be excluded fromattending school Exclusion from school and sports activities should be reserved for those with wound drainage ("pus") that cannot be covered and contained with a clean, dry bandage and for those who cannot maintain good personal hygiene
Environmental Control The 5 C s of Community Associated MRSA CLEANLINESS: Hand hygiene, bathing, laundering of clothing/uniforms COMPROMISED: Skin integrity - Keep wound(s) clean and covered CONTACT: Avoid contact with other people s wounds or bandages CONTAMINATION: Avoid sharing personal items (water bottles, towels, etc. Clean and disinfect environment CROWDING: Implement measures to avoid overcrowding, as appropriate

 undefined
undefined