MLTSS in PA and Other States
This informative presentation delves into MLTSS implementation in Pennsylvania and other states, exploring Community HealthChoices, coverage details, managed care plans, and the LIFE alternative. Learn about the services covered, eligibility criteria, and how individuals can navigate these programs effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
MLTSS in PA and Other States: What We Know and What We Can Learn Larke Recchie, CEO, Ohio Association of Area Agencies on Aging Pam Walz, Supervising Attorney, Community Legal Services Fran Chervenak, Senior Attorney, Pennsylvania Health Law Project 1
Implementing MLTSS in PA: Community HealthChoices SW Fran Chervenak, Senior Attorney Pennsylvania Health Law Project 2
What is Community Health Choices? 3 CHC is a new mandated Medicaid managed care program for certain people on Medicaid: Duals, those in OLTL waivers, people in nursing homes For those moving to CHC, CHC plan will cover their Medicaid physical health services and their long- term services and supports (LTSS) LTSS is a new term that includes the various services people get at home (previously through Waiver programs) or in a nursing home Not all people moved to CHC will get LTSS
CHC Coverage Coverage through managed care plans Everyone in CHC gets Medicaid physical health coverage Adult Benefit Package NOTE: Behavioral health coverage carved out If determined NFCE, also get Long Term Services and Supports (LTSS) At home or in nursing home Broad LTSS Service Package-all services covered by previous waivers + new services (pest eradication; employment supports) Specific services covered based on need; detailed in service plan Consumer/Participant direction for certain services Nursing Home Transition still available 4
CHC Managed Care Plans AmeriHealth Caritas: 1-855-235-5115; www.amerihealthcaritaschc.com PA Health & Wellness: 1-844-626-6813; www.PAHealthWellness.com UPMC Community HealthChoices: 1-844-833-0523; www.upmchealthplan.com/chc 5
LIFE as an Alternative to CHC LIFE will continue to exist as an alternative to CHC Persons in LIFE who want to stay do not go into CHC Those in CHC target population who qualify can move to LIFE To be eligible for LIFE, person must: Be age 55 or older Live in a county where LIFE is available Be NFCE and be able to be safely served in community Financially qualify or privately pay Income Limit: $2,250/month (applicant only) Resource Limit: $8,000 (spousal impoverishment rules apply) 6
CHC Replaces Certain Waivers Once CHC starts in a region, the following Waiver programs no longer exist: Aging Attendant Care CommCare Independence OBRA exists for people <21 and those who meet Intermediate Care Facility level of care ID/Autism Waivers still exist Adult Autism Consolidated Person/Family Directed Supports 7
Impact on Those in Options/ACT 150 Options and ACT 150 are not Medicaid programs They are state-funded programs that provide in-home services: Options for those age 60+; not eligible for Aging Waiver Act 150 for those < 60; not eligible for Attendant Care Waiver These programs still exist Options/Act 150 services are not changing Some people in these programs may move to CHC 8
CHC Phased Roll-out Phase - Date 1 3 January 2018 3 2 January 2019 1 2 3 3 January 2020 9
CHC Southwest Basics CHC started in 14 counties January 1, 2018 Who moved to CHC? All dual eligibles (those on Medicare and Medicaid) Everyone 21+ in the waivers managed by the Office of Long Term Living (OLTL) Anyone 21+ in nursing home whose care is covered by Medicaid 10
CHC Southwest Basics 85,000 older adults and persons with disabilities moved into CHC They either chose a plan (40%) or were auto- assigned Almost are in UPMC CHC 1/3 are in PA Health & Wellness Remainder in Amerihealth Caritas People can change their CHC plan at any time 11
Continuity of Care Protections To protect consumers transitioning to CHC, plans are required to pay for care and to pay providers for certain period: 60 days for medical care that was previously authorized or if person in a course of treatment 180 days (until 6/30/18) for those already getting waiver services when CHC started, including continued use of the same LTSS providers Ongoing for those already in a Nursing Home when CHC starts 12
General Comments on Implementation We had an erratic start-up with several delays, legal challenges to RFPs and contracts OLTL s priority and focus was on those getting LTSS and little attention paid to plain duals CHC is very nuanced and complicated program that is layered on top of already existing complicated systems of care OLTL is being very hands on in initial phase to try and quickly identify & address issues 13
CHC Participant Issues Ongoing confusion and misunderstanding about CHC-especially for those who are dual eligible Confusion over co-pays-especially Rx co-pays Misunderstanding about medical and non- medical transportation under CHC Consumers in transition along with CHC-new to LTSS, moving out of region, moving between programs 14
Provider Issues Lack of awareness/confusion about CHC by medical providers 2 of the 3 CHC plans are new to the region Slow provider network development by CHC plans Medicare provider confusion about billing CHC plans for secondary coverage Service coordinators struggling to learn new system and to work with CHC plans 15
Issues for Advocates Misunderstanding and confusion over CHC and how it affects individual consumers Insurance companies offering multiple plans/products Lack of clarity about dual eligibles and how CHC works with Medicare Understanding where to go for help with CHC problems 16
Implementing MLTSS in PA: Assessing Need for LTSS and the Appeals Process Pam Walz, Managing Attorney Community Legal Services of Philadelphia 17
InterRAI Designated tool used by MCOs for needs assessment: InterRAI-Home Care Assessment System Proprietary tool developed through University of Michigan Role in person-centered service planning? Connective relationship due to shared technical platform with proposed new functional eligibility determination tool (FED). Algorithm determines level of care
Grievances and Complaints Background: Federal managed care regulations, 42 C.F.R. 438.400 et seq. State regulations, 28 Pa. Code 9.701 Grievances appeal in federal regs For adverse actions Complaints grievance in federal regs For quality of care, treatment/violation of rights by MCO or provider, certain other issues
Grievances To challenge adverse actions : the denial, approval at a lesser amount than requested, reduction, suspension or termination of an item or service
Right to continued services If the enrollee is already getting services or items that MCO proposes to reduce, change or discontinue, enrollee can continue to receive them until appeal decision if grievance filed orally or faxed, post-marked or hand- delivered within 10 days of date of written notice of adverse action.
Step One file a grievance Call MCO to file grievance orally or Fill out Complaint/Grievance form included in denial notice or write a letter, and deliver to MCO by mail or fax. Provider can file grievance for enrollee with enrollee s written consent (but can t request continuing services).
Timing Must file grievance within 60 days of date on notice of adverse action MCO must issue decision within 30 days May request expedited resolution: Available where MCO determines (in case of a request from enrollee) or medical provider sends letter stating that taking 30 days could seriously jeopardize enrollee s life, physical or mental health, or ability to attain, maintain or regain maximum function.
Expedited Resolution Medical provider must send letter in support of expediting within 72 hours of enrollee s request for expedited decision. MCO must decide expedited grievance within 72 hours after receiving the request or within 48 hours of receiving doctor s letter, whichever is sooner.
Grievance Procedures Enrollee gets letter acknowledging grievance, with information re review process Enrollee may ask to see information MCO used to decide to take the adverse action at no cost, including medical necessity criteria and any processes, strategies or evidentiary standards used in setting coverage limits . 42 C.F.R. 438.404(b)(2).
Grievance procedures, cont. Enrollee may (but is not required to) attend grievance review in person, by phone or by videoconference if available. MCO must provide 15 days notice. MCO must provide enrollee with reasonable opportunity, in person and in writing , to present evidence and make legal and factual arguments.
Grievance committee Must include at least 3 people, including a licensed physician. DHS: physician must decide grievances. MCO staff on committee must not have been involved in or subordinate to anyone involved in the issue being grieved.
Step Two If grievance decision is unfavorable, enrollee may do either or both of the following: Request a fair hearing and/or Ask for external grievance review
Fair Hearing Must request within 120 days of date on grievance decision notice. Complete and sign fair hearing request form included in decision or write a letter. Right to continued services if fair hearing request post-marked or hand-delivered within 10 days. Enrollee must participate in fair hearing (in person or by phone).
Fair hearing procedures MCO is a party and attends to defend its actions. Must be decided within 90 days from date grievance filed, not including the days between written grievance decision and filing of fair hearing request. If not decided within 90 days, can request Interim Assistance by calling DHS.
Expedited Fair Hearing Can request on fair hearing request form or by calling or faxing letter to DHS. BHA will schedule telephone hearing within 3 business days. Doctor or dentist must fax signed letter explaining why standard time frame would harm enrollee s health OR doctor/dentist must testify about this at hearing. If not, decision will not be expedited and another hearing will be scheduled using standard time frame.
External Grievance Review Request by calling or writing MCO within 15 days of grievance decision. MCO will send request to Department of Health (DOH). Review by doctor who must be independent of both MCO and state. 42 CFR 438.402(c)(1)(i)(B)(2) DOH will notify enrollee of external reviewer s name and contact info. MCO must send grievance file to reviewer.
External grievance review (cont.) Enrollee must send any additional information within 15 days. Decision must be issued within 60 days. May be appealed to court of competent jurisdiction . Right to expedited external grievance review
Complaints Either 1 or 2 levels of complaint review, depending on complaint subject. If enrollee incorrectly labels a complaint or grievance, MCO is supposed to correct the categorization.
Complaint types with 1 level of review Failure of MCO to timely provide services it has approved, Denial of service/item on ground that it is not covered service Denial of payment to provider after service has been delivered Denial of enrollee request to dispute financial liability, including cost-sharing. Failure to timely decide complaint or grievance
Two levels of complaint review Quality of care or services provided Rudeness by MCO staff or provider Violation of enrollee s rights All other complaints.
Time frame to decide first level complaint MCO has 30 days to decide complaint. May be extended by up to 14 days at enrollee s request.
Options after First Level Complaint For issues for which there is only 1 level of internal complaint, enrollee may: Request fair hearing within 120 days, Request external complaint review by either DOH or Insurance Department (PID) within 15 days or both For all other complaints, enrollee may request 2nd level complaint review. MCO has 45 days to decide 2nd level complaint.
Options after 2nd Level Complaint Request external review by either DOH or PID within 15 days. DOH reviews complaints involving care or services, while PID reviews complaints about MCO s policies and procedures. DOH and PID will determine appropriate agency to do the external review.
PAELA MyCare Ohio: February 24, 2018 Larke Recchie recchie@ohioaging.org (614) 481-3511 Lessons Learned from the Demonstration for Integrated Care Ohio Association of Area Agencies on Aging www.ohioaging.org Facebook: o4aadvocacy Twitter: @o4aadvocacy
A Little About Ohio AAAs 12 AAAs cover all 88 counties in Ohio--non-profit orgs Diverse population with seven urban centers and rural Appalachian areas Plan, coordinate, and administer federal state and local programs promoting independence at home Act as front door to LTSS Case manage older adults and people with disabilities Advocate on a federal, state and local level for older adults MyCare Ohio
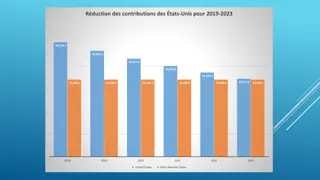
Medicaid / Long-term care penetration Long Term Care Expenditures SFY17 All Medicaid = $25.6 Billion LTC Expenditures FY17 LTC = $7.3 Billion FFS NF 20.9% 29% MyCare 32.9% FFS Aging Waiver 4.8% FFS ODM Waiver 1.7% FFS PDN/HH/DME 7.0% 71% DODD Services 32.8% Long Term Care Rest of Medicaid 42
MyCare Ohio is more than MLTSS Managed long-term services and supports (MLTSS) uses managed care plans (MCPs) to deliver a range of long-term services and supports usually encompassing institutional and home and community based care (HCBS) MyCare Ohio has a MLTSS component but also includes integration with Medicare, the health and acute care payment source for people dually eligible for Medicare and Medicaid
Key Provision of the Ohio Dual Demonstration: MyCare Ohio ICDS Regions NE United CareSource Buckeye Lake NEC United CareSource Lucas Fulton Ottawa NW Aetna Buckeye Geauga Managed Care Plans Cuyahoga Wood Trumbull Lorain Portage Medina Summit 7 total regions 2 Plans per region except 3 in Cleveland region Mahoning Wayne Stark Columbiana EC United CareSource Union Delaware WC Molina Buckeye Central Molina Aetna Franklin Clark Madison Montgomery Greene Pickaway Plans awarded include: Aetna Better Health CareSource Butler Warren Clinton SW Molina Aetna Hamilton Molina United Clermont Buckeye Health (Centene) ICDS Regions and Demo Counties NEC- Northeast Central NW - Northwest Central SW - Southwest EC - East Central WC - West Central NE - Northeast
MyCare Ohio Five year demonstration project that integrates Medicare and Medicaid into one program operated by a Medicare Medicaid Plan (MMP) Current enrollment is at its highest: Approximately 112,000 (70% opt-in with both Medicare & Medicaid) 3 year report on website http://medicaid.ohio.gov/Portals/0/Initiatives/M LTSS/MyCare_Ohio_Progress_Report_2017.pdf The future of My Care Ohio (expires 12/31/2019) move to MLTSS?
Key Provision of the MyCare Ohio Dual Demonstration Care delivery model Managed Care Plans coordinate Medicare & Medicaid services through a person-centered planning process Plans must contract with AAAs to provide waiver service coordination for enrollees over age 60 Some plans fully delegate care management of all waiver members Financing CMS capitated financial alignment model Benefits Nearly all Medicare and Medicaid services and plan flexibility to add benefits Targeted population Est. 114,00 beneficiaries Excludes those with developmental disabilities
Successes of MyCare 70% opt-in rate (highest in country) Since 2015, MCPs have been involved in the closure of 7 poor performing nursing facilities MCPs in MyCare reduced the number of NF resident days by 4% through 2015 HEDIS scores: MyCare MCPs outpaced national averages on care plan completion, documented care plan goals, and follow-up care visits
Lessons Learned *From advocate view Provider payment is key Appropriate penalties and alternative payment models Example: 99% payment in 30 days aggregate broken down revealed 30% HCBS payment in 30 days Provider education and training -- Clean claims Allow ample roll out and have vigorous readiness review Quality Measures: make sure they measure LTSS and not just health care (HEDIS, CAHPS) Robust appeals and grievance and ombudsman processes IT systems at MCPs and State should be up to the task of enrollment, risk stratification, payment, patient liability, etc.
Why Ohio might move to MLTSS only? Promote the health, safety, and well-being through care coordination. Expand community LTSS options, and streamline and standardize the way people access them. Create a system where health care providers are incentivized to keep individuals healthy and eliminate gaps in service delivery. Strengthen the focus on quality measurement, including both quality of life and quality of care, in order to achieve better outcomes. Ensure transparency, accountability, effectiveness, and efficiency of the program. Ensure long-term sustainability of the system as demand for LTSS grows by managing costs. (Ohio Medicaid LTSS expenditures are growing at a faster than the national average) Less cumbersome than CMS driven MyCare Medicare/Medicaid 49
State identified areas of challenge * The information provided in the following slides are initial ideas from Ohio Medicaid with intent to continue work with stakeholders to improve implementation of MLTSS. Member Transition System Integration Managed care plan readiness Comprehensive assessments Waiver services Provider reimbursement Patient liability Value-based contracting Network adequacy Provider and member education