Mechanism of Action of Antifolate Drugs in Bacterial Synthesis
Folate-derived cofactors are crucial for cell growth, with bacteria relying on de novo synthesis while humans need preformed folate. Antifolates like sulfonamides and trimethoprim disrupt folate synthesis in bacteria, inhibiting DNA synthesis. This article explores how these drugs target bacterial enzymes involved in folate production, contrasting with human folate metabolism.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Antifolate Antifolate Drugs Drugs Antifolate Antifolate Drugs Drugs
Folate-derived cofactors are essential for the synthesis of purines and other compounds necessary for cellular growth and replication. Therefore, in the absence of folate, cells cannot grow or divide. To synthesize the critical folate derivative, tetrahydrofolic acid, humans must first obtain preformed folate in the form of folic acid from the diet. In contrast, many bacteria are impermeable to folic acid and other folates and, therefore, must rely on their ability to synthesize folate de novo. The sulfonamides sulfonamides (sulfa drugs) are a family of antibiotics that inhibit de novo synthesis of folate. A second type of folate antagonist trimethoprim trimethoprim prevents microorganisms from converting dihydrofolic acid to tetrahydrofolic acid, with minimal effect on the ability of human cells to make this conversion. This second group includes also pyrimethamine pyrimethamine, which inhibits folate reduction in some protozoa and is primarily used to treat toxoplasmosis and malaria and methotrexate which inhibits folate reduction in mammalian cells and is used in the treatment of neoplastic and autoimmune diseases Thus, both sulfonamides and trimethoprim interfere with the ability of an infecting bacterium to perform DNA synthesis. Combining the sulfonamide sulfamethoxazole sulfamethoxazole with trimethoprim (the generic name for the combination is cotrimoxazole cotrimoxazole) provides a synergistic combination. methotrexate,
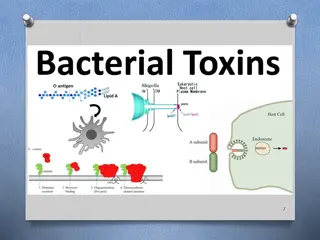
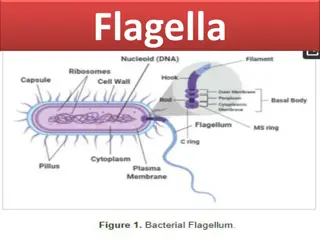
Mechanisms of Action Mechanisms of Action Bacterial synthesis of folate begins with the fusion of pteridine , glutamate and p-aminobenzoic acid (PABA) to form dihydrofolate. step involves the enzyme dihydropteroate synthase. dihydropteroate synthase. Dihydrofolate is then converted to tetrahydrofolate tetrahydrofolate by dihydrofolate reductase In bacteria, the sulfonamides and trimethoprim inhibit sequential steps in the synthesis of folate. The sulfonamides are structural analogues of PABA and competitively inhibit dihydropteroate synthase and the effect of the sulfonamide may be overcome by adding excess PABA. (This is why some local anaesthetics, which are PABA esters such as procaine antagonise the antibacterial effect of these agents). Trimethoprim inhibits bacterial dihydrofolate reductase. Mammals must obtain folic acid in their diet because they are unable to synthesize dihydrofolate. Once absorbed, dihydrofolate is converted to tetrahydrofolate and active folate derivatives (methyl, formyl, and methylene tetrahydrofolate) that donate single-carbon atoms during the synthesis of purine bases and other components of DNA. Although dihydrofolate reductase is found in both microbial and mammalian cells, the affinity of trimethoprim for the enzyme in bacteria is about 100,000 times greater than its affinity for the mammalian enzyme. dihydrofolate. This dihydrofolate reductase. procaine can
Sulfonamides Sulfonamides In the 1930s, sulfanilamide metabolite of Prontosil, a dye that had been developed in the search for bacterial stains with antimicrobial properties. This discovery led to the synthesis and development of a large number of sulfonamide compounds to treat bacterial infections. Only a few of these are still used today. sulfanilamide was found to be the active Spectrum, Indications, and Bacterial Resistance Spectrum, Indications, and Bacterial Resistance The sulfonamides were the first drugs used in the treatment of systemic bacterial infections. They were once active against a wide variety of organisms. Over the years, however, significant resistance resistance to sulfonamides has developed in many bacterial species and the antimicrobial spectrum of these drugs has been greatly reduced. The sulfa drugs are seldom prescribed alone except in developing countries, where they are still employed because of their low cost and efficacy. The sulfa drugs, including cotrimoxazole, are bacteriostatic.
Sulfonamides inhibit both gram-positive bacteria, such as Staphylococcus sp and gram-negative enteric bacteria such as Escherichia coli, Klebsiella pneumoniae, Salmonella, Shigella, and Enterobacter sp, as well as Nocardia sp, Chlamydia trachomatis, and some protozoa. They are active against select Enterobacteriaceae in the urinary tract and Nocardia infections. . Sulfamethoxazole Sulfamethoxazole is administered in combination with trimethoprim(see below). Sulfadiazine Sulfadiazine is available in the form of silver sulfadiazine sulfadiazine ointment to prevent or treat burn infections and other superficial skin infections. The silver ions in this preparation have antibacterial activity and contribute to its efficacy in this setting. In addition, sulfadiazine in combination with the dihydrofolate reductase inhibitor pyrimethamine is the preferred treatment for toxoplasmosis. Sulfadoxine pyrimethamine is used as an antimalarial drug. Sulfacetamide topically to treat blepharitis and conjunctivitis, ocular infections that are common throughout the world. It is also effective in treating trachoma highly contagious ocular infection that is caused Chlamydia trachomatis and is prevalent in Asia and the Middle East. silver Sulfadoxine in combination with Sulfacetamide is administered trachoma, a Bacteria that can obtain folate from their environment are naturally resistant to these drugs. Acquired bacterial resistance to the sulfa drugs can arise from plasmid transfers or random mutations. Resistance is generally irreversible and may be due to 1) an altered dihydropteroate synthetase, 2) decreased cellular permeability to sulfa drugs, or 3) enhanced production of the natural substrate, PABA.
Pharmacokinetics Pharmacokinetics The sulfonamides are benzene sulfonic acid amide derivatives. Most sulfonamides are adequately absorbed from the gut an exception is sulfasalazine sulfasalazine which is not absorbed when administered orally or as a suppository and, therefore, is reserved for treatment of chronic inflammatory bowel disease. The sulfonamides are bound to serum albumin in the circulation and are widely distributed to tissues and fluids throughout the body, including the cerebrospinal fluid. The half-lives of sulfonamides vary greatly, but the most widely used compounds for treating human infections, such as sulfacetamide sulfamethoxazole sulfamethoxazole, , have half-lives ranging from 6 to 10 hours. Sulfonamides are converted to inactive compounds by N- acetylation in the liver, and the parent drug and its metabolites are excreted in the urine. The acetylated metabolites are less soluble than the parent compound in urine, and they can precipitate in the renal tubules, causing crystalluria is important for patients who are being treated with a sulfonamide to consume adequate quantities of water. sulfacetamide and crystalluria. Therefore it
Adverse Effects Adverse Effects Historically, drugs containing a sulfonamide moiety, including antimicrobial sulfas, diuretics, diazoxide, and the sulfonylurea hypoglycemic agents, were considered to be cross-allergenic. However, more recent evidence suggests cross- reactivity is uncommon and many patients who are allergic to nonantibiotic sulfonamides tolerate sulfonamide antibiotics. In some patients, sulfonamides cause skin rashes, which are hypersensitivity reactions that can remain mild or progress to a serious or life-threatening form, such as erythema multiforme or Stevens Stevens Johnson syndrome. Other adverse effects of sulfonamides include crystalluria, gastrointestinal reactions, headaches, hepatitis, and hematopoietic toxicity. In persons with glucose glucose 6 6 phosphate dehydrogenase deficiency, phosphate dehydrogenase deficiency, sulfonamides can cause hemolytic anemia. hemolytic anemia. Kernicterus Kernicterus may occur in newborns, because sulfa drugs displace bilirubin from binding sites on serum albumin. The bilirubin is then free to pass into the CNS, because the blood brain barrier is not fully developed. Contraindications: Contraindications: Due to the danger of kernicterus, sulfa drugs should be avoided in newborns and infants less than 2 months of age, as well as in pregnant women at term. Sulfonamides should not be given to patients receiving methenamine, since they can crystallize in the presence of formaldehyde produced by this agent. Johnson syndrome.
Trimethoprim Trimethoprim Trimethoprim Trimethoprim is a synthetic amino-pyrimidine drug. It is a potent inhibitor of bacterial dihydrofolate reductase and exhibits an antibacterial spectrum similar to that of the sulfonamides. However, trimethoprim is 20- to 50-fold more potent than the sulfonamides. Trimethoprim is most often compounded with sulfamethoxazole, producing the combination called cotrimoxazole. Trimethoprim is active against many aerobic gram- negative bacilli and a few gram-positive organisms (It is active against most Staphylococcus aureus strains, both methicillin-susceptible and methicillin-resistant). It is usually administered in combination with sulfamethoxazole to prevent or treat urinary tract infections, but it is occasionally used alone for UTIs and treatment of bacterial prostatitis. Resistance Resistance in gram-negative bacteria is due to the presence of an altered dihydrofolate reductase that has a lower affinity for trimethoprim. Efflux pumps and decreased permeability to the drug may play a role.
Pharmacokinetics Pharmacokinetics: It is well absorbed from the gut and is widely distributed to tissues. After extensive hepatic metabolism, the remaining parent compound and metabolites are excreted in the urine. Trimethoprim is a weak base and is concentrated in acidic prostate tissues and vaginal fluids via ion trapping trapping. This makes trimethoprim useful in the treatment of bacterial prostatitis and vaginitis. The adverse effects The adverse effects of trimethoprim include nausea, vomiting, and epigastric distress; rashes and other hypersensitivity reactions; hepatitis; and effects of folic acid deficiency which include megaloblastic anemia, leukopenia, and granulocytopenia, especially in pregnant patients and those having very poor diets. These blood disorders may be reversed by the simultaneous administration of folinic acid, which does not enter bacteria. ion
Trimethoprim Trimethoprim- -Sulfamethoxazole Sulfamethoxazole Sulfamethoxazole and trimethoprim have synergistic activity against susceptible organisms and are available in fixed-dose combinations to treat bacterial infections. The synergistic antimicrobial activity of cotrimoxazole results from its inhibition of two sequential steps in the synthesis of tetrahydrofolic acid. Spectrum and Indications Spectrum and Indications Cotrimoxazole exhibits bactericidal activity against some organisms that are not susceptible to either drug given alone. Cotrimoxazole is active against members of the family Enterobacteriaceae Enterobacteriaceae, , including strains of Escherichia coli, Klebsiella pneumoniae, Proteus species, and Enterobacter species. Cotrimoxazole is often used to prevent or treat urinary tract prostate infections prostate infections caused by these organisms. Because of increased bacterial resistance to cotrimoxazole, it is not recommended for the empiric treatment of urinary tract infections in locations where greater than 30% of E. coli isolates are resistant to cotrimoxazole. In these locations, fosfomycin, nitrofurantoin, or a fluoroquinolone drug can be used to treat these infections. Cotrimoxazole is not active against Pseudomonas aeruginosa, a common cause of urinary tract infections in hospitalized patients. urinary tract and
Cotrimoxazole is also the drug of choice for treating pulmonary infections caused by Pneumocystis (carinii) (carinii) and Nocardia Nocardia asteroides asteroides, which most often occur in immunocompromised patients. It is active against some strains of Haemophilus influenzae and Moraxella catarrhalis. It is active against some strains of Salmonella and Shigella, but other strains are resistant. Currently a fluoroquinolone is usually preferred to treat most infections caused by these organisms. It also has activity against MRSA. Resistance to the trimethoprim sulfamethoxazole combination is less frequently encountered than resistance to either of the drugs alone, because it requires that the bacterium have simultaneous resistance to both drugs. Pneumocystis jiroveci jiroveci
Pharmacokinetics Pharmacokinetics Sulfamethoxazole has been combined with trimethoprim because it has a similar half-life (10 hours). In vitro tests show that maximal synergistic activity occurs when the concentration of sulfamethoxazole is 20 times greater than the concentration of trimethoprim. To obtain plasma drug concentrations in a ratio of 20 : 1, the drugs are administered in a ratio of five parts of sulfamethoxazole to one part of trimethoprim. The 5 : 1 dose ratio produces a 20 : 1 plasma concentration ratio because trimethoprim has a greater volume of distribution than does sulfamethoxazole.
Cotrimoxazole is generally administered orally, intravenous infusion is used for moderately severe to severe pneumocystis pneumonia. Both agents distribute throughout the body. Cotrimoxazole readily crosses the blood brain barrier. Both parent drugs and their metabolites are excreted in the urine. Adverse Effects Adverse Effects The adverse effects of cotrimoxazole are similar to those of the individual drugs. Reactions involving the skin are very common and may be severe in the elderly. Nausea and vomiting are the most common gastrointestinal adverse effects. Cotrimoxazole can cause megaloblastic megaloblastic anemia anemia in persons who have a low dietary intake of folic acid, but this adverse effect is uncommon.
Antimicrobial Agents Affecting Bacterial Antimicrobial Agents Affecting Bacterial Topoisomerases Topoisomerases Fluoroquinolones Fluoroquinolones Fluoroquinolones Fluoroquinolones have become increasingly important in the treatment of a wide range of infections because of their broad-spectrum bactericidal activity and attractive pharmacokinetic properties. Unfortunately, overuse resulted in rising rates of resistance in gram- negative and gram-positive organisms, increased frequency of Clostridium difficile infections, and identification of numerous untoward adverse effects. The original fluoroquinolones, such as ciprofloxacin primarily active against gram-negative bacteria. Newer agents, such as levofloxacin levofloxacin, have good activity against both gram-positive and gram-negative organisms. ciprofloxacin, are
Chemistry and Mechanism of Action Chemistry and Mechanism of Action The original quinolone, nalidixic acid, had limited antimicrobial activity. Successive modification of its structure by the addition of a fluorine atom and other moieties resulted in a group of fluoroquinolones with increased affinity for DNA gyrase and a broader spectrum of antimicrobial activity, and a better safety profile. In all organisms, DNA topology is regulated by a family of enzymes, the DNA DNA topoisomerases topoisomerases. . Every organism requires at least one type I and one type II topoisomerase enzyme to manage DNA supercoiling during DNA transcription and replication. Fluoroquinolones inhibit two types of bacterial type IIA topoisomerase, of which one is called DNA the other is designated type IV topoisomerase type IV topoisomerase. These topoisomerase enzymes are essential for maintaining DNA in a stable and biologically active form. bacterial type IIA DNA gyrase gyrase and
DNA gyrase introduces negative circular bacterial DNA. These negative supercoils eliminate the positive positive supercoils supercoils that occur ahead of the DNA replication fork during DNA replication. DNA replication cannot proceed without DNA gyrase activity, DNA gyrase produces supercoiling by breaking doubled-stranded DNA, moving a section of double- stranded DNA through the break, and resealing the broken strands of DNA. Type IV topoisomerase is responsible for separating the DNA of daughter chromosomes once DNA replication is completed. This process is called decatenation decatenation. . In general, DNA gyrase is the primary target of fluoroquinolones in gram-negative bacteria, whereas topoisomerase IV is the primary target in gram-positive organisms. negative supercoils supercoils into closed
Spectrum and Indications Spectrum and Indications Fluoroquinolones have bactericidal activity spectrum of gram-positive and gram-negative bacteria and acid-fast bacilli. Fluoroquinolones exhibit concentration dependent killing, dependent killing, and it appears that maximal bacterial killing occurs when the ratio of the peak serum drug level to the organism s minimal inhibitory concentration is at least 10. Most fluoroquinolones have a long postantibiotic effect, with some organisms failing to resume growth for 2 to 6 hours after drug levels are no longer detectable. Because of their favorable properties, fluoroquinolones can be given orally to treat some infections that formerly required parenteral therapy with other drugs. bactericidal activity against a broad concentration
Fluoroquinolones may be classified into generations based on their antimicrobial targets. The nonfluorinated quinolone nalidixic nalidixic acid acid is considered to be first generation, with a narrow spectrum of susceptible organisms. Ciprofloxacin Ciprofloxacin and norfloxacin generation because of their activity against aerobic gram- negative and atypical bacteria. In addition, these fluoroquinolones exhibit significant intracellular penetration, allowing therapy for infections in which a bacterium spends part or all of its life cycle inside a host cell (for example, chlamydia, mycoplasma, and mycobacteria). Levofloxacin Levofloxacin(is the L-isomer of ofloxacin and has largely replaced it clinically) is classified as third generation because of its increased activity against gram- positive bacteria. Lastly, the fourth generation includes moxifloxacin moxifloxacin, gemifloxacin gemifloxacin, and delafloxacin their activity against anaerobic and gram-positive organisms. generations norfloxacin are second ofloxacin delafloxacin because of
Ciprofloxacin Ciprofloxacin has excellent activity against gram-negative bacteria and is used to treat infections caused by enteric gram-negative bacilli, gonococci, chlamydia, and P . aeruginosa, including urinary tract infections, infections, prostatitis prostatitis, , and pelvic inflammatory disease. pelvic inflammatory disease. Ciprofloxacin is used to treat bacterial diarrhea bacterial diarrhea caused by Campylobacter, Salmonella(Salmonella typhi: Typhoid fever Typhoid fever), and Shigella species, as well as Yersinia enterocolitica, and they are effective in treating traveler traveler s diarrhea, s diarrhea, which is typically caused by enterotoxigenic strains of E. coli. Fluoroquinolones are used in combination with other drugs to treat intra-abdominal infections, bone and joint infections, skin infections, and febrile neutropenia. Ciprofloxacin is also indicated to treat anthrax anthrax and for postexposure prophylaxis of inhalational anthrax, such as might occur in a bioterrorism event. Ciprofloxacin is also used as a second-line agent in the treatment of tuberculosis. tuberculosis. It achieves high concentrations in neutrophils, and this contributes to their effectiveness in patients with mycobacterial infections. urinary tract bioterrorism event. Levofloxacin Levofloxacin maintain the bacterial spectrum of second generation agents, with improved activity against Streptococcus spp., including S. pneumoniae, methicillin susceptible Staphylococcus aureus, and Mycobacterium spp.
The advanced or respiratory fluoroquinolones (moxifloxacin, gemifloxacin gemifloxacin, , and delafloxacin delafloxacin ) have enhanced gram-positive activity, including Staphylococcus and Streptococcus spp.while retaining activity against gram-negative organisms. These drugs are used to treat respiratory tract infections, including sinusitis and bronchitis and pneumonia. Delafloxacin has activity against methicillin-resistant Staphylococcus aureus (MRSA) and Enterococcus faecalis. Further, delafloxacin and moxifloxacin have activity against Bacteroides fragilis, while maintaining activity against Enterobacteriaceae and Haemophilus influenzae. From this group, only delafloxacin has activity against Pseudomonas aeruginosa. Lastly, these agents maintain atypical coverage, with moxifloxacin and delafloxacin showing activity against Mycobacteria spp. Several fluoroquinolones (ciprofloxacin, levofloxacin, moxifloxacin) are available in formulations for topical ocular administration to treat bacterial conjunctivitis. conjunctivitis. These drugs are also the most commonly prescribed drugs for treating bacterial corneal ulcers. ulcers. moxifloxacin, corneal
Bacterial Resistance Bacterial Resistance Resistance to fluoroquinolone drugs has increased among both gram- positive and gram-negative pathogens. This resistance develops through two primary mechanisms: alterations in the target enzymes (topoisomerases) and alterations in drug access to the target enzymes. Alterations in bacterial DNA gyrase occur most commonly in gram- negative bacteria, whereas alterations in type IV topoisomerase are more prevalent in gram-positive organisms. Resistance by DNA gyrase mutations is usually caused by decreased affinity of DNA gyrase for the drugs. Topoisomerase IV mutations also lead to reduced fluoroquinolone binding affinity. Resistance to fluoroquinolones can also occur through expression of membrane transport proteins or efflux pumps efflux pumps that actively transport a number of antibacterial agents out of bacterial cells and thereby confer multidrug resistance. multidrug resistance. In addition, some gram-negative bacteria have decreased levels of porins porins in their outer membrane, resulting in decreased fluoroquinolone uptake by these bacteria.
Pharmacokinetics Pharmacokinetics Fluoroquinolones are usually given orally, and ciprofloxacin, levofloxacin, moxifloxacin and delafloxacin can also be administered intravenously. Ciprofloxacin has a half-life of 4 hours and is usually administered every 12 hours. Advanced fluoroquinolones have half-lives ranging from 7 to 12 hours and are given once every 24 hours to treat most infections. Fluoroquinolones are well absorbed from the gut, but can chelate divalent and trivalent cations, including calcium, iron, magnesium, and zinc. Therefore fluoroquinolones should be taken 2 hours before or 2 hours after ingesting foods and drugs containing these cations.
Fluoroquinolones are widely distributed to tissues, and their concentrations in the lungs, kidneys, liver, gallbladder, prostate, and female reproductive tissues are often two to five times greater than their plasma concentrations. Fluoroquinolones undergo varying degrees of hepatic biotransformation, and they are excreted unchanged in the urine, along with their metabolites. Moxifloxacin is excreted primarily by the liver, and no dose adjustment is required for renal impairment.
Adverse Effects and Interactions Adverse Effects and Interactions Fluoroquinolones are generally well tolerated. The most common adverse effects are nausea, vomiting, and diarrhea. Headache and dizziness may occur. However, they can cause serious adverse effects, These agents carry boxed warnings for tendinitis, tendon rupture tendinitis, tendon rupture, peripheral neuropathy, and CNS effects (hallucinations, anxiety, insomnia, confusion, and seizures. These drugs have a high affinity tendons, where they exert direct toxic effects on the tendon matrix and cause tendon cell death by activating apoptosis pathways (programmed cell death). The risk of tendonitis and tendon rupture is increased in persons over 60 years of age, patients with renal insufficiency and in those taking corticosteroids. Articular cartilage erosion (arthropathy arthropathy) has been observed in immature animals exposed to fluoroquinolones. Therefore, these agents should be avoided in pregnancy and lactation and in children and adolescents except for distinct clinical scenarios (for example, cystic fibrosis exacerbation). Patients taking fluoroquinolones are at risk for phototoxicity resulting in exaggerated sunburn reactions. Patients should use sunscreen and avoid excessive exposure to ultraviolet (UV) light. phototoxicity
Other adverse effects of fluoroquinolones include alterations in blood glucose alterations in blood glucose (hypoglycemia and hyperglycemia), hepatotoxicity, and prolongation of the QT interval prolongation of the QT interval of the electrocardiogram leading to ventricular tachycardia. These effects are more likely to occur in persons with other risk factors for these conditions, such as those with diabetes. Ciprofloxacin inhibits P450 1A2- and 3A4- mediated metabolism. Serum concentrations of medications such as theophylline, tizanidine, warfarin, ropinirole, duloxetine, caffeine, sildenafil, and zolpidem may be increased.
Urinary Tract Antiseptics Urinary Tract Antiseptics Nitrofurantoin Nitrofurantoin Nitrofurantoin Nitrofurantoin is a synthetic nitrofuran derivative. It inhibits various enzymes and damages bacterial DNA. It is administered orally and is rapidly excreted in the urine. Because of its low plasma concentrations, its antibacterial activity is limited to the urinary bladder. Ingesting nitrofurantoin with food enhances its absorption and reduces the risk of gastrointestinal irritation. Antibacterial spectrum: Antibacterial spectrum: Nitrofurantoin is bactericidal against gram- positive and gram-negative bacteria that commonly cause acute lower urinary tract infections, including E. coli, Enterococcus faecalis, K. pneumoniae, and Staphylococcus saprophyticus. Nitrofurantoin, however, is not active against Proteus species, Serratia species, or P . aeruginosa. Acquired microbial resistance to nitrofurantoin has generally not been a significant clinical problem. Adverse effects: Adverse effects: Nitrofurantoin is usually well tolerated, but it can cause gastrointestinal irritation, nausea, vomiting, and diarrhea. To avoid these adverse effects, a macrocrystalline macrocrystalline formulation formulation of the drug is usually employed. The large drug crystals in this formulation dissolve slowly in the gut, producing less gastrointestinal distress than do other formulations. Less common adverse effects of nitrofurantoin include pulmonary fibrosis, hepatitis, and hemolytic anemia in patients with G6PD deficiency.
Methenamine Methenamine Mechanism of action: Mechanism of action: Methenamine is a heterocyclic organic compound that decomposes at an acidic pH of 5.5 or less in the urine, thus producing formaldehyde, which acts locally and is toxic to most bacteria. Bacteria do not develop resistance to formaldehyde, which is an advantage of this drug. [Note: Methenamine is frequently formulated with a weak acid (for example, mandelic acid or hippuric acid) to keep the urine acidic. The urinary pH should be maintained below 6. Antacids, such as sodium bicarbonate, should be avoided.] Antibacterial spectrum: Antibacterial spectrum: Methenamine is primarily used for chronic suppressive therapy to reduce the frequency of UTIs. Routine use in patients with chronic urinary catheterization to reduce catheter- associated bacteriuria or catheter-associated UTI is not generally recommended. Methenamine should not be used to treat upper UTIs (for example, pyelonephritis).
Pharmacokinetics: Pharmacokinetics: Methenamine is administered orally. In addition to formaldehyde, ammonium ions are produced in the bladder. Because the liver rapidly metabolizes ammonia to form urea, methenamine is contraindicated in patients with hepatic insufficiency, as ammonia can accumulate. Methenamine is distributed throughout the body fluids, but no decomposition of the drug occurs at pH 7.4. Thus, systemic toxicity does not occur, and the drug is eliminated in the urine. Adverse effects: Adverse effects: The major side effect of methenamine is gastrointestinal distress, although at higher doses, albuminuria, hematuria, and rashes may develop. Methenamine mandelate is contraindicated in patients with renal insufficiency, because mandelic acid may precipitate. [Note: Sulfonamides, such as cotrimoxazole, react with formaldehyde and must not be used concomitantly with methenamine. The combination increases the risk of crystalluria and mutual antagonism.]
 undefined
undefined