Insights into Recent Quality Alerts for Bexley Patients
Review the quality alerts reported for Bexley patients, focusing on medicines-related issues and learnings from red and amber graded alerts. Cases cover medication errors, lack of follow-up, and adverse effects, highlighting the importance of review processes and specialist involvement in patient care.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
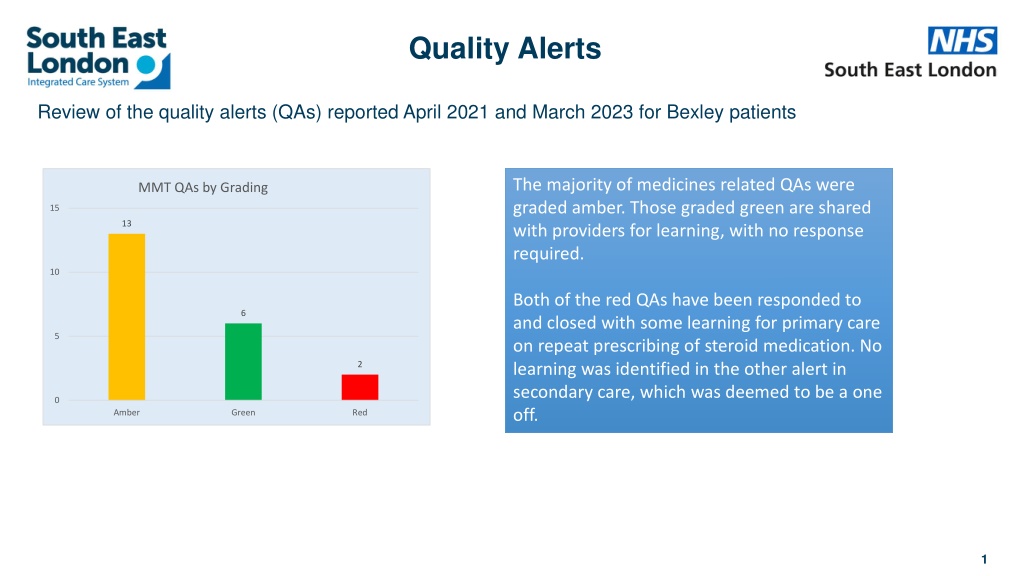
Quality Alerts Review of the quality alerts (QAs) reported April 2021 and March 2023 for Bexley patients The majority of medicines related QAs were graded amber. Those graded green are shared with providers for learning, with no response required. MMT QAs by Grading 15 13 10 Both of the red QAs have been responded to and closed with some learning for primary care on repeat prescribing of steroid medication. No learning was identified in the other alert in secondary care, which was deemed to be a one off. 6 5 2 0 Amber Green Red 1
Quality Alerts Learning from Red graded quality alerts Patient admitted with abdominal pain and on review of notes from previous admission in July 2020 it was found that patient was given a diagnosis of SLE. She was discharged on Hydroxychloroquine and Prednisolone 20mg daily with the discharge summary noting For outpatient follow up with rheumatology . There was no follow up appointment and the patient continued to be prescribed Prednisolone by her GP at the same dose for the next two years without review by any specialist team. There are 24 consecutive primary care prescription records between August 2020 and April 2022 which state Prednisolone 5mg tablets, take 4 tablets (20mg) once daily until Rheumatology review, 112 tablet . (ID 4181) Response / Learning from the GP practice It is noted on the discharge summary from Gastroenterology that Prednisolone is recorded as a new medication prescribed since admission. It is recorded in the Discharge Plan and Clinical Information/Summary that Outpatient follow-up would be arranged with Rheumatology. The medication was therefore entered in her records and first issued in August 2020. We note that the medication was entered on to her 'repeat medication' list as it had been assumed that Rheumatology follow-up would be arranged by the hospital and the medication potentially altered/tapered following this. However, as the follow-up did not take place the medication continued to be issued at the original dose. We have taken learning from this incident and have now put a system in place to ensure that steroid medication is reviewed on a regular basis and monitored, these measures will ensure that continual repeat prescribing does not happen in the future. 2
Quality Alerts Inpatient discharged from Cardiology with colchicine tablets as directed but he has developed increasing nausea and now has started with diarrhoea. He was advised to report this to the GP but as this use of colchicine is off license, the GP was unable to advise on this or offer an alternative. (ID 4281) Response The Cardiology Consultants that cared for the patient during their admission with pericarditis have advised that if the patient has side effects from the medication colchicine it should be stopped immediately, they would not prescribe an alternative medication. The Trust advised that if GPs need to contact the team to discuss issues such as this in the future, they recommend contacting the ward the patient was discharged from for advice (noted on the electronic discharge notification eDN) or the secretary of the named consultant for the patient. 3
Quality Alerts Learning from amber graded quality alerts An 84 yr. old discharged to Rehab following hip surgery after a fall at home. Medications on discharge were Ibuprofen 400 mg TDS, Enoxaparin 40mg and Alendronate. Proton pump inhibitors were prescribed and omeprazole 40 mg once a day. The patient was re admitted the following day with coffee ground vomit and a low haemoglobin and an AKI eGFR 18 with deranged LFTs. Endoscopy showed extensive gastric ulceration. The patient was transfused and medically managed but went on to develop a HAP and was treated with intravenous antibiotics. On 04/05/20 the patient was confirmed covid positive, in the coming days the patient became increasing unwell and a DNACPR was put in place. On 15/05/20,the patient sadly died. Response from the GP Practice In General Practice patients on Alendronic Acid are reviewed after 5 years as per guidance below: The need to continue bisphosphonate treatment for osteoporosis should be re-evaluated periodically based on an assessment of the benefits and risks of treatment for individual patients, particularly after 5 or more years of use. The medication was started in July 2018, patient would have had a review in July 2023.There is no other specific Monitoring undertaken in the GP Surgery. The Trust completed an RCA and identified learning around co prescribing of NSAID Enoxaparin 40mg and Alendronate and the report was shared with the widow who requested further review around the prescribing and monitoring of the Alendronate acid. To offer the widow closure the Trust are looking at this but are not clear where this was first prescribed and the detail of any GP monitoring that was in place. Learning from this case was discussed at the practice clinical meeting in July 2021. (ID 1023) 4
Quality Alerts Response from Cardiology The Clinical Lead for Cardiology confirmed that Dapaglifozin was started by the cardiology SpR when the patient was referred for a cardiac opinion by one of the medical wards. Unfortunately, the medical ward team were not aware that this medication was an Amber medication and apologise for the patient being discharged without the transfer of care document being completed. The clinical lead for Cardiology has raised your concern at the Cardiology governance meeting to ensure patients who are not on a speciality ward but are discharged on speciality treatment have the relevant transfer of care document completed where appropriate. It was also noted that the patient has since been seen by the community heart failure team. Response from the Pharmacy team If the patient is initiated on Dapagliflozin as an inpatient, the hospital will provide a month s supply on discharge. A discharge letter is sent to the GP with the initiation information and monitoring/follow up requirements. There is no specific transfer of care documentation, however the following should be included in the discharge letter: - Indication for therapy, including an updated HF management/medicines optimisation plan, and details of the shared decision-making process/counselling with the patient - Baseline renal function assessment and BP reading (include baseline HbA1c if checked) - Details of HF specialist and/or community HF team for follow up/support within the first month (if required). If initiated in hospital, patients will be reviewed by the initiating HF team or referred to the community HF team. When Dapagliflozin for HF is started as an inpatient, the clinician must ensure that the initiation checklist is completed. The ward pharmacist will clinically screen the prescription and as part of this process ensures that the initiation checklist has been completed. The ward pharmacist facilitates the discharge process and prompts the ward doctors to complete any transfer of care documentation. Ward teams have been reminded to check drug formulary status and of the importance of completing any additional documentation and information to support safe patient discharge. A Patient who was admitted following a fall then developed arrhythmia as an inpatient. This was investigated and significant medication changes made. They were discharged with plan for GP follow up and with a note that the hospital team would refer to community heart failure team for specialist follow up. An amber 1 drug (dapagliflozin) had been started while he was an inpatient, but no adequate plan for prescription, titration and monitoring under specialist supervision. The GP requested that heart failure team reviewed the patient as a matter of urgency and it transpired that they had not received a referral from the inpatient team. The GP continued the prescription despite Amber 1 status to maintain patient safety and made contact with the heart failure team to ensure timely follow up. The practice team arranged necessary medication monitoring tests as they were appropriately asked to do. (ID 2862) 5
Quality Alerts Learning from green graded quality alert Response from the Dialysis Team The concerns raised by the GP were discussed with the Clinic Manager for Sidcup Dialysis Unit. EMLA cream has always been prescribed by the patient s GP. The dialysis unit only provides a week s supply at the beginning so that the patient can have enough time to get the prescription. Some patients may have it on their repeat prescription, some may have to drop a note to the GP surgery requesting to add EMLA to their prescription when they are running low on supply Patient advised to contact GP practice for prescription of Emla cream for dialysis treatment. The patient is frail, needing to put a request in for medication and then wait 48 hours to get it from her pharmacy. The GP felt this was unnecessary work for both reception and clinical staff at the practice and said that given this is needed for her treatment why is it not provided by the dialysis unit? As the patient had a start at Borough dialysis unit, the unit would have provided that to her. Our Clinic Manager for Sidcup Dialysis Unit has checked with the patient regarding their EMLA cream and the patient has confirmed that she received two packs (10 tubes) of EMLA cream from our dialysis unit. She has also confirmed that the pharmacy is trying to resolve the prescription with the GP. This was shared with the MMT lead at Bexley to follow up with the practice. For information - due to the volume of green graded QAs raised there is no requirement for providers to give a response. 6
Medication related Serious Incidents Four serious incidents where medication errors was identified as the primary issue were reported for Bexley patients between Apr-21 and Mar-23 as detailed below. StEIS Number 2020/8079 Patient seen in to ED with severe vomiting and jaundice related to high alcohol intake. On arrival tests showed life threateningly low potassium which was rapidly corrected with IV sodium chloride and potassium. The blood gas test in ED indicated that her sodium level was critically low at 102 but this was not initially acknowledged in the ED notes. There was significant delay of 9 hours in the low sodium result being confirmed by the pathology lab and then a further 3-hour delay before the patient was referred to intensive care. During the 12 hours, she received 2.5L sodium chloride which contributed to over rapid correction of her sodium level, resulting in the osmotic demyelination syndrome. Had the low sodium result available from the VBG machine been acted on earlier and the patient monitored more closely, it is possible that the sodium level would have been restored more slowly and the osmotic demyelination syndrome avoided. Brief description of incident Learning It is vital to have a robust system to monitor abnormal sodium levels in a timely fashion. It needs to ensure that clinicians are confident in the accuracy of all aspects of point of care VBG results There is need to improve management of abnormal sodium levels by facilitating teaching across the Trust The Trust s Clinical Guideline for the Management of Hyponatraemia and Hypernatraemia in Adults need to be updated to reflect the need for regular, timely monitoring, including discussion with intensive care and or Critical Care Outreach Team where appropriate Communication between the medical and pathology teams needs to be improved to ensure timely constructive discussion about any potential abnormal results. 2020/23706 Patient unwell on admission, admitted to ICU for renal replacement. Working diagnosis- Biliary sepsis with multisystem failure. Angioedema secondary to drugs. NSTEMI on 03/09/20 - angio + PCI at GSST. Hypertrophic cardiomyopathy. Patient -plan for heparin. Patient had new bilateral rectus sheath haematomas and was on anti-platelets already. Heparin infusion commenced for six hours, then discontinued. Any patient bleeding who is on dual/triple antiplatelet agents post PCI and stenting requires urgent senior discussion with the cardiologists regarding the need to temporarily/permanently reduce or stop their antiplatelet treatment It is vital that senior staff implement proactive supervision of more junior / less experienced staff who are caring for those who are becoming critically unwell. 2021/1615 A 13 year old boy incorrectly prescribed anti-epileptic medication, Phenobarbitone. After 4 days of taking Phenobarbitone, the patient was taken to ED with symptoms of sleepiness and unsteadiness. At this point it was identified that the Phenobarbitone was in fact a different medication to the Phenibut and the symptoms related to over sedation from the Phenobarbitone. The Phenobarbitone was stopped and the patient made a full recovery. The incident took place over the period of the coronavirus pandemic which posed challenges with respect to accessing local services and arranging face to face consultations. Medications prescribed in other countries should either be physically checked or original prescription records reviewed. Professional curiosity should be exercised when doses or dosing regimens appear to be unusual and outside of standard practice. Independent interpreters should be used at all appointments when there may be communication difficulties due to language. Dispensing procedures for outpatient pharmacies should be followed particularly in the case of a controlled drug and where there are language difficulties 2021/14735 Patient self-presented to the ED via a GP referral due to increased confusion. Following assessment she was diagnosed as having a urinary tract infection and was given a stat dose of 2 tablets of Nitrofurantoin and discharged with a 3 day course. She was brought back by ambulance later the same day having collapsed in the street. On checking her summary care record by LAS and GP from 2019 LAS identified she was allergic to nitrofurantoin. Importance of checking all allergies at the point of triage Importance of checking all allergies during patients journey through the ED Importance of checking allergies at the point of prescribing, administration and dispensing Importance of complying with the Trusts Medicine s Policy
Quality Team Your Quality contacts for Bexley are: harpinder.priest@selondonics.nhs.uk sue.higgins@selondonics.nhs.uk Please share this link to raise a Quality Alert: DCIQ: NHS South East London ICS Quality Alerts reporting form (datixcloudiq.co.uk) Contact the team via email at qualityalerts@selondonics.nhs.uk For serious incident queries at qualityteam@selondonics.nhs.uk 8