Inflammation and Tissue Repair
Inflammation is a complex process involving cardinal signs like redness, swelling, heat, and pain. Factors such as immune responses and tissue repair play crucial roles. Causes of inflammation range from infections to trauma and surgery, while granulomatous inflammation is associated with foreign bodies and specific infections. Vascular changes and cellular stages in acute inflammation further highlight the body's response mechanisms.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
INFLAMMATION, TISSUE REPAIR, AND WOUND HEALING
CARDINAL SIGNS OF INFLAMMATION Rubor (redness) Tumor (swelling) Calor (heat) Dolor (pain) Functio laesa (loss of function)
FACTORS INVOLVED IN PROTECTIVE RESPONSES AND BODILY REPAIR Inflammatory reaction Immune response Tissue repair and wound healing
CAUSES OF INFLAMMATION Immune response to infectious microorganisms Trauma Surgery Caustic chemicals Extremes of heat and cold Ischemic damage to body tissues
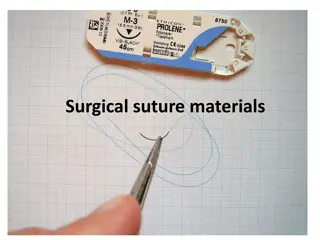
GRANULOMATOUS INFLAMMATION Associated with foreign bodies such as Splinters Sutures Silica, asbestos Associated with microorganisms that cause Tuberculosis Syphilis, sarcoidosis Deep fungal infections Brucellosis
VASCULAR CHANGES THAT MAY OCCUR WITH INFLAMMATION An immediate transient response Occurs with minor injury An immediate sustained response Occurs with more serious injury and continues for several days and damages the vessels in the area A delayed hemodynamic response Involves an increase in capillary permeability that occurs 4 to 24 hours after injury
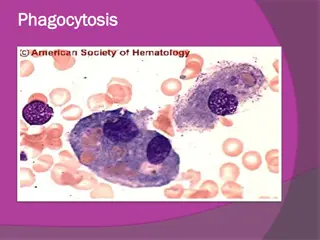
CELLULAR STAGE OF ACUTE INFLAMMATION Marked by movement of phagocytic white blood cells (leukocytes) into the area of injury Two types of leukocytes participate in the acute inflammatory response: Granulocytes (neutrophils, eosinophils, and basophils) Monocytes (the largest of the white blood cells)
DIRECTION OF CELLULAR RESPONSE Margination, adhesion, transmigration Cytokines Adhesion molecules Selectins, integrins, and immunoglobulin Initiation of adhesion Aggregation of inflammatory cells Movement into underlying tissue
INFLAMMATORY MEDIATORS Histamine Cytokines Arachidonic acid metabolites Eicosanoids Prostaglandins Leukotrienes Omega-3 polyunsaturated fatty acids Platelet-activating factor Plasma proteins
CLASSIFICATION OF INFLAMMATORY MEDIATORS BY FUNCTION Those with vasoactive and smooth muscle constricting properties Chemotactic factors such as complement fragments and cytokines Plasma proteases that can activate complement and components of the clotting system Reactive molecules and cytokines liberated from leukocytes, which when released into the extracellular environment can damage the surrounding tissue
TYPES OF INFLAMMATORY EXUDATES Serous Exudates Watery fluids low in protein content Result from plasma entering the inflammatory site Hemorrhagic Exudates Occur when there is severe tissue injury that causes damage to blood vessels or when there is significant leakage of red cells from the capillaries
TYPES OF INFLAMMATORY EXUDATES (CONTINUED) Membranous or Pseudomembranous Exudates Develop on mucous membrane surfaces Are composed of necrotic cells enmeshed in a fibropurulent exudate Purulent or Suppurative Exudates Contain pus; composed of degraded white blood cells, proteins, and tissue debris Fibrinous Exudates Contain large amounts of fibrinogen and form a thick and sticky meshwork
BASIC PATTERNS OF INFLAMMATION Acute inflammation Of relatively short duration; non-specific early response to injury Aimed primarily at removing the injurious agent and limiting tissue damage Chronic inflammation Longer duration lasting for days to years A recurrent or progressive acute inflammatory process or a low- grade smoldering response that fails to evoke an acute response
CHRONIC VERSUS ACUTE INFLAMMATION Acute inflammation self-limited and of short duration (recall that there are vascular and cellular stages) Infiltration of neutrophils Exudate Chronic inflammation self-perpetuating and may last for weeks, months, or even years Infiltration by mononuclear cells (macrophages) and lymphocytes Proliferation of fibroblasts-responsible for tissue building during wound repair
MOST PROMINENT SYSTEMIC MANIFESTATIONS OF INFLAMMATION Acute-phase response Alterations in white blood cell count (leukocytosis or leukopenia) Fever Sepsis and septic shock (severe)
TYPES OF STRUCTURES OF BODY ORGANS AND TISSUES Parenchymal Tissues contain the functioning cells of an organ or body part (e.g., hepatocytes, renal tubular cells) The Stromal Tissues Consist of the supporting connective tissues, blood vessels, extracellular matrix, and nerve fibers
TYPES OF BODY CELLS INVOLVED IN TISSUE REGENERATION Labile Continue to divide and replicate throughout life, replacing cells that are continually being destroyed Stable Normally stop dividing when growth ceases Permanent Cells Cannot undergo mitotic division
HEALING BY PRIMARY OR SECONDARY INTENTION The objective of the healing process is to fill the gap created by tissue destruction and to restore the structural continuity Primary healing small gap, no tissue loss, clean wound Secondary healing great loss of tissue with contamination
BASIC COMPONENTS OF THE EXTRACELLULAR MATRIX (ECM) Fibrous structural proteins Collagen and elastin fibers Water-hydrated gels that permit resilience and lubrication Proteoglycans and hyaluronic acid Adhesive glycoproteins that connect the matrix elements to each other and to cells Fibronectin and laminin
BASIC FORMS OF THE ECM Basement Membrane Surrounds epithelial, endothelial, and smooth muscle cells Interstitial Matrix Present in the spaces between cells the connective tissue and between the epithelium and supporting cells of blood vessels
STAGES OF WOUND HEALING Inflammatory phase Proliferative phase-key cell is the fibroblast Maturational or remodeling phase
STEPS IN DEVELOPMENT OF A NEW CAPILLARY VESSEL Proteolytic degradation of the parent vessel basement membrane, allowing for formation of a capillary sprout Migration of endothelial cells from the original capillary toward an angiogenic stimuli Proliferation of the endothelial cells behind the leading edge of the migrating cells Maturation of the endothelial cells and proliferation of pericytes (for capillaries) and smooth muscle cells (for larger vessels)
TISSUE REPAIR (OVERLAPS INFLAMMATORY PROCESS) Tissue Regeneration Replacement of injured tissue with same cell type Fibrous tissue repair Severe damage may not heal with regeneration alone. Repair may occur with replacement of tissue with connective tissue which generates granulation tissue (red, moist connective tissue that contains newly developed blood vessels)
FACTORS REGULATING THE HEALING PROCESS Action of chemical mediators and growth factors that mediate the healing process Interactions between the extracellular and cell matrix
TWO PHASES OF SCAR FORMATION Emigration and proliferation of fibroblasts into the site of injury Deposition of the ECM by these cells
CAUSES OF IMPAIRED WOUND HEALING Malnutrition Impaired blood flow and oxygen delivery Impaired inflammatory and immune responses Infection Wound separation Foreign bodies Age effects