Improving Access to Healthcare for Care Homes in East of England
The healthcare improvement plan developed by the Mid and South Essex Sustainability and Transformation Partnership aims to enhance healthcare services for care home residents in the region. By leveraging innovation and technology, the initiative includes a successful proxy ordering program in partnership with Firza Group. Manor Lodge Care Home served as the pilot for this program, streamlining prescriptions and medication management to enhance person-centred care delivery in a complex care setting.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
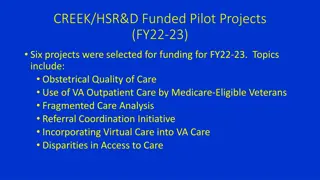
GP Proxy Access for Care homes Best Practice examples: All Regions Alison Taylor RN Digital Transformation Manager NHSX May 2021
GP Proxy Access for Care homes Best Practice examples: All Regions East of England Firza Group London North West London South West London Midlands Northamptonshire Coventry and Warwickshire North East Yorkshire & Humber NEY accelerator site Wakefield North West William Blake House Morecambe Bay Cheshire West Lancashire South East South East ICS South West NHS Bristol, North Somerset & South Gloucestershire CCG Devon CCG Sound PCN
East of England - Firza Group Background / Description of the part of the process the best practice covers. The Mid and South Essex Sustainability and Transformation Partnership (STP) have been developing a healthcare improvement plan to support the increasing number of people residing within their 5 CCGs (Basildon and Brentwood; Mid Essex; Southend-on-Sea; Castle Point and Rochford; and Thurrock) requiring healthcare support. It is widely recognised that their healthcare services needed to be streamlined to make them more efficient and effective for patients and care home residents and their families/carers. Providing a more joined-up approach to local healthcare services within Mid and South Essex STP would propel delivery of care to become a more person-centred solution. From the very start of the partnership with Firza, it was very clear that Mid and South Essex STP strongly believed in both innovation and technology to improve healthcare within the local community. Prior to the start of the proxy ordering programme, Firza had delivered what was deemed by Mid and South Essex STP to be a very successful MOCH service, which save the NHS 28K in a year for just 1 care home alone. It was down to this success and the close relationships Firza had already developed with a lot of local GP surgeries and care homes, that Firza was approached by Debalina Gupta (Mid and South Essex STP Primary Care Commissioning Manager) and Alison Taylor (Senior Programme Manager) to help with the roll out of proxy ordering. Initially, it was agreed to run a trial on the largest and most complex of care homes within Mid and South Essex STP, Manor Lodge (Chelmsford). It was decided that the funding obtained from NHS England would be utilised for this project. If successful, the trial would then be rolled out across further care homes in the region. Situation: (in other words what was the issue) With a total population of 1.2m, Mid and South Essex STP provides at total of 8000 care home beds within its 302 care homes. With only 179 GP practices supporting this infrastructure, the pressures on the healthcare system were immense. Manor Lodge Care Home is a very well-run care home which has received many accolades for both care of their residents and also their staff (Care Home Awards Finalist 2021; Dementia Hero Awards 2021; UK Employee Experience Awards 2021 and Residential Care Provider of the Year 2021). Manor Lodge stands as the largest (with 120 beds) and most complex care home within Mid and South Essex STP, which at the time was attached to 5 separate GP surgeries. The idea behind starting with Manor Lodge was, if proxy ordering can be successfully run on such a vast and complex care home, then adoption should be relatively simple for any other care home. Although, a well-run care home, the carers always seemed to be chasing their tales, spending a significant amount of time chasing prescriptions or missing medication. This impacted on the amount of time and individual care they could spend with each resident which meant person-centred care always seemed to take a back seat. This totally went against their ethos of how they thought a care home should be run. Reasons for the inefficiency and lengthy lead times was down to the complexity of handling physical paper requests. This led to long lead times, as quite often they were physically driven over by a courier or carer after finishing a work shift. This was not only slow, but also created room for error as there was room for human error and orders would sometimes go missing, not to mention the environmental impact of this too. Prior to proxy, once the medication order was submitted, there was no visibility in terms of the progress of the order.
East of England - Firza Group What change did they want to bring about? Primary care colleagues in Mid and South Essex STP recognised that their own GPs were tremendously under resourced, as they struggled to meet local demand and believed an overhaul was required to provide a more resilient and efficient service. Solution and impact / benefits: The solution was to transition from paper-based medication ordering to proxy ordering throughout Mid and South Essex STP. The aim was to bring medication ordering in to the 21stcentury by enabling care homes/GP surgeries and local pharmacies to be able to work in much more efficient and effective way with each other. Initially, Firza contacted each surgery to ascertain whether they wanted to make the move over to proxy ordering. When this was the case, it was Firza s responsibility to contact the relevant care homes to enrol them into the system and ensure they met all requirements (secure email system, relevant technology), provided relevant training, and helped propel forward the whole process from cradle to grave (including obtaining rights to set up proxy access). The trial project proved to be a great success and within a year, was rolled out further across 5 CCGs over 10 weeks. This was part of the national roll out of proxy ordering, where each CCG was given a target to reach 25% of care homes live. The target was to enrol 74 care homes within Mid and South Essex STP. This target was smashed as 108 care homes ended up being enrolled and continues to grow. Total No. of CH 25% Remaining CH to Reach Target -4 -2 -18 CH to Achieve Correct Surgery Access CH Contacted Forms Received Training Provided CCG Live % Live (Target 25%) The table shows the success of proxy ordering implementation within the 5 CCGS. 51 93 94 13 23 23 23 53 43 15 32 25 16 32 39 17 25 41 3 17 2 33.33% 27.17% 44.57% Basildon & Brentwood Mid Essex Southend- on-Sea Castle Point & Rochford Thurrock 32 8 18 12 9 14 2 -6 43.75% 32 7 15 11 6 11 0 -4 37.93%
East of England - Firza Group In order to ensure the project was a success, all of the following points were considered: Planning: Initially the target homes were identified using NHS England survey data and local intelligence. Each of the relevant people (care home staff) and tasks for proxy ordering for the care home residents were identified and implemented. Communication: Educating the relevant stakeholders as early as possible was essential to ensure adoption uptake was efficient and effective. It was important for the project to be successful, so staff buy-in during the initial stages needed to be established as quickly as possible. A productive training programme was designed and implemented for each of the care home users to meet this new process. Resources: Transitioning to a digital platform, meant that as part of the process, the relevant equipment was identified and made available (in a suitable location), accessible to the relevant individuals (generation of login details; technology such as a PC and Monitor/iPad and a stable internet connection; access rights granted by the relevant surgeries; creating a secure email account) Data Protection: The care home staff needed to sign data protection declarations each time new GP surgery access was obtained to ensure patient information was kept confidential. The benefits for the proxy ordering programme have been immense. The digitalisation of the medication ordering process for care homes has meant that the overall pathway has significantly reduced. This has resulted in the speeding up the whole ordering-to-delivery process and has also meant that there is less room for error, as the need for historic technology has become redundant through this process (e.g., faxing and/or delivery of prescription requests). Proxy ordering provides a much more resilient platform for users working at the care homes (nurses and carers) as it has forced care homes to install a bullet proof encrypted email system (in most cases this tended to be the setup of NHSmail). Adoption of NHSmail was in some cases lengthy due to previous rollouts of this platform not being properly utilised, which meant potential users were locked out. Medicine s waste has significantly reduced as the system only enables medication to be issued that has been specifically requested. There has been a noticeable reduction in errors and queries associated with ordering, issuing, collecting, and dispensing (e.g., missing items) since implementation. The team involved in the ordering process within the care homes and GP surgeries have visibility to a full audit trail so at any one time, they have the tools to check on the ordering status. Previously, a significant amount of time was taken to chase missing items. Now, there is little/no requirement for this action. The lead pharmacy technician at Firza, as a direct result from the success of this project, was invited to present to the East of England region which is where Cambridge and Peterborough CCG requested to rollout proxy ordering.
East of England - Firza Group Key learning points: It soon came to light that once a care home agreed to use proxy ordering, the GP surgeries, although they bought in to the service, had no time to set up proxy for the care home. The CCG then decided that Firza would handle the service end-to-end. The support needed is in setting up the patients in the clinical systems to allow access. It is a time-consuming process which needs dedicated time and currently due to COVID we don t have that in the surgery and the same is probable at the nursing homes. Last time Alison came into the surgery and did this for us while supporting the nursing home staff at their end. If we could do the same we would proceed immediately. Practice Manager, Mid and South Essex GP Surgery The Firza team involved soon came to realise that if the GP surgery did not keep on top of medication reviews, then this would cause further issues and prevent any medications being ordered. If a patient is overdue a review/out of sync, the proxy platform will not let the user place an order for that medication. Some medicines are still manually inputted (e.g., for acute medicines). When this is the case, an audit trail will not be available but in the case of Manor Lodge, they will email the surgery with the request. GP surgeries are still able to order items on an ad hoc basis when required through adding irregularly issued template to the item. It is important that the proxy service is set up for every new care home resident as part of the care home registration process. However, findings were, that when left to the GP surgery, many of the residents were not set up. Firza was previously dealing with ad hoc requests to train admin staff at surgeries as it was not embedded into the process. Some surgeries set it up incorrectly when left to set proxy up themselves. (e.g., for each patient they would have to log in and log out which does not make sense)
East of England - Firza Group Key contact: add a named contact, ideally both from the NHS organisation and the supplier who can be contacted for more information (can also add generic emails if no known contact) Vikki Hartland, Medicines Management Technician, vikki.hartland@nhs.net, 07825 005 659 Irfan Mirza, Head of Integrated Care, Irfan.mirza@firza.health, 0203 488 1595 Confirm internal approval from the organisations referred to in the case study: Yes
London Region North West London North West London CCG Medicines Management Team Background / Description of the part of the process the best practice covers. Engagement from GP Practice, Community Pharmacy, PCN Pharmacist. Training on the repeat ordering process as a collaborative. This helped with identifying medicine champions for each organisation, agreed process for communication, requests for acute prescriptions, interim prescriptions and newly discharged patients and ordering cut off times. Times and days of ward rounds with a structured approach. CCG pharmacist provided support to the PCN pharmacists on setting the proxy accounts up for the residents on the GP system, liaising with the care home on collecting consent forms. Training was provided to the care home. Situation: (in other words what was the issue) As part of the PCN DES a new GP had taken over looking after the care home. The practice was not familiar with care home processes which resulted in miscommunication including frequent telephone calls to chase up outstanding prescription and paper requests for new cycle medication which were going missing. What change did they want to bring about? Reduce telephone call, requests on paper for repeat, interim and acute medicines
London Region North West London North West London CCG Medicines Management Team Solution and impact / benefits: Cycle Planner shared with details of community pharmacy cut off times for ordering, Single point of contact created for all organisations, Contact details shared Regular three way meetings set up PCN pharmacist responsible for proxy ordering set up Key learning points: Collaborative training improves communication processes. Key contact: add a named contact, ideally both from the NHS organisation and the supplier who can be contacted for more information (can also add generic emails if no known contact) Communication via Shamim Jivraj (s.jivraj@nhs.net), NWL CCG Lead Pharmacist for Adult Health Confirm internal approval from the organisations referred to in the case study: No need to discuss with organisations
London Region South West London South West London CCG Medicines Management Team Background / Description of the part of the process the best practice covers. In the Merton Borough, South West London CCG, the care homes pharmacy team covers 39 care homes, with a range of nursing, residential and learning disabilities homes. We identified Eltandia Hall Care Home as one of our priority care homes for implementing proxy access, who were keen to progress with this process. It is one of our large care homes with 83 beds, specialising in the provision of residential care, nursing care and young person s care. There are four units, split over two floors each with their own carers/nurses. The medical services are provided by two separate GP practices. Description of the best practice process: We are at the early stages of implementation of proxy access for Eltandia Hall Care Home; this report pertains to the initial engagement meetings, the completion and transfer of documentation from the care home to the GP practice. Situation: (in other words what was the issue) Ordering repeat medications from two different GP practices using the conventional paper-based system has always been a challenge and a time-consuming activity for both the care home and the two GP practices. Often both the care home and GP practice staff are having to spend a lot of time chasing or querying the prescription requests when items are missing off prescriptions or when there is confusion with the supplying pharmacy about what had been ordered/collected, which is compounded as there are two GP practices involved.
London Region South West London South West London CCG Medicines Management Team What change did they want to bring about? Eltandia Hall Care Home want to order their regular repeat medicines via proxy access for their residents, wishing to work closely with both practices to make this change. The issues with using a paper-based system, is that it is a time-consuming process. The GP practices would get requests from the care home in various formats, such as paper MAR charts, emails, or faxes and often at irregular times. Both the care and GP practices involved would like to streamline the ordering / request process for repeat medications using an online system. Solution and impact / benefits: Solution The solution to ordering repeat medications involved the initiation of the proxy ordering process. Engaged with Wideway Surgery, Tamworth Medical Centre and Eltandia Hall Care Hall; booked in virtual MS meetings for each GP practice and the care home, relevant staff attended. A follow-up email was sent providing next steps to be undertaken by both the GP practice and the care home together with the relevant documentation. Screening medications (not a medication review) was an additional step to screen medication prescribed for each resident prior to moving over to proxy access. This step was seen as an opportunity to ensure only appropriate repeat medication would be visible and available to order by care home staff to reduce the risk of medication errors and medicines waste.
London Region South West London South West London CCG Medicines Management Team Solution and impact / benefits: Impact/benefits The impact has been for the care home to prioritise obtaining consent and allowing protected time for the care home staff to undertake this activity. The care home manager prioritised those residents with capacity and those without capacity and then processed the consent forms. The care home undertook the consenting process as a focussed piece of work, and it took them approximately 2 weeks to complete all the consent forms for their 79 residents. Consent for those lacking capacity was undertaken in the same way as for the COVID 19 vaccinations. In general, the impact for the care home and the GP practice participating in this project was to find the time to attend (virtual) meetings and complete the necessary documentation (DSA and DPIA), however both feel that this is time well spent as it will help with the ordering of repeat medications in the long run. The benefits will not be realised until the first repeat medication cycle has been processed. Key learning points: Merton Borough Care Homes Pharmacy Team: Prior knowledge of all the relevant proxy access processes and being aware of the NHS E documentation. When organising the engagement meetings, we learnt that it is important to invite the key decision-makers, e.g., for the GP meetings, the key person with responsibility for deciding the level of data sharing from the medical record and for the care home meetings, the care home manager. Post meetings, it was important to send an email detailing the next steps that should be taken to the GP practice and care home, reinforcing the actions / documentation to be completed. Regular contact with the GP practice and care home is important to keep track of progress. Clarification of roles for the pharmacy team and the project officer to avoid duplication of effort by agreeing what each party will do.
London Region South West London South West London CCG Medicines Management Team Key learning points: Care Home: Get organised and decide which residents can provide consent themselves and those that cannot (i.e., lack capacity), therefore will need to contact NOK / LPA etc. Focus on obtaining consent for proxy access and try not to get distracted. Getting the care home staff on board is key, as they will be supporting this process. Be mindful that Mental Health Assessments will need to be undertaken and a best Interests meeting for those residents lacking capacity, so allow time for this part of the process, as it may take a bit longer. Communicating the proxy access process to the NOK / LPA was easier over the phone, rather than sending a letter. The care home recorded the date and time of the meetings with the NOK / LPA. GP Practices: Ensure that the Data Sharing Agreement and the DPIA are sent over to care home at the same time and followed-up when they have been signed by the care home. Obtain the staff authorisation and consent forms at the same time so that the process of assigning the proxy with resident can be initiated. Confirm internal approval from the organisations referred to in the case study: Yes, verbal approval from manager at Eltandia Hall Care Home.
North East Yorkshire & Humber Accelerator site North East Yorkshire & Humber - Example during outbreak/lockdown 1 of COVID-19 The North East and Yorkshire (NEY) region accelerated the roll out as a care home embargoed by a community pharmacy struggled to order routine medicines. From implementing proxy medication ordering online the impact for the 111/999 calls and A & E admissions shows a decline of 24% which is statistically significant. If this were scaled up to include all care homes nationally it would equate to an approximate reduction of 400 admissions per annum. With an average admission costing 2273 this equates to a saving of approximately 909,000 (including 111 call, A & E attendance, and admission costs). Even if we took a more conservative saving of 15% it would still equate to a saving in the region of 568,000. Although some hospital admissions are unavoidable, there are some circumstances where early recognition and intervention of deteriorating clinical symptoms could have meant people were managed in their usual place of residence and avoided an admission to hospital, particularly so of urinary tract infections (UTIs) if the correct medication information is available at the right time to the right healthcare professionals in that resident s care.
NEY - Wakefield Background / Description of the part of the process the best practice covers. Using multiple communication channels to increase awareness and engagement for both care homes and GP practices including PCN and practice pharmacy professionals. Situation: (in other words what was the issue) We found that many care homes and GP practices are not aware of proxy/online ordering for care homes. Both parties are often unaware of the system that can be used, the benefits for all parties, including safety, time saving, reduced queries. Also, to avoid the use of the term proxy ordering as this is often misunderstood, use the phrase online ordering of medicines or similar. What change did they want to bring about? To raise awareness of proxy/online ordering and increase engagement from both care homes and GP practices, also including other stakeholders. Solution and impact: Raising awareness and increasing the profile of proxy/online ordering will increase engagement and uptake, therefore improving procedures and clinical safety for both care home and GP practice. GP practices working together within their PCNs and sharing good practice and implementation strategies will help to build resilience, which in turn will help to facilitate the ongoing ownership and maintenance of the system.
NEY - Wakefield Key learning points: Utilise all communication channels available in the locality. Several of our local areas have a weekly meeting for all care home managers which can be attended to raise the profile of proxy/online ordering directly with target audience. Liaise with your local authority as provider of care homes to allow contact with all care home managers. If you have a Communications Team within your organisation you may wish to engage with them to send very short surveys to all care home managers to establish their current process for ordering medicines and gauge their interest in proxy/online ordering. This enables the care homes who have registered an interest to be set up first! Attend practice meetings/target events/prescribing events to showcase the benefits of proxy/online ordering to GP practices. Many GP practices believe this to be complex and labour intensive and are unaware of the clinical and safety benefits. You may also wish to send short surveys to GP Practice Managers to gauge their current stance and allow prioritisation. Include information on proxy/online ordering in any bulletins or updates sent to general practices from your organisation, including contact details of key stakeholders. Utilise contact with PCN pharmacy colleagues to share knowledge of proxy/online ordering with their practices and encourage engagement. Encourage the development of a two-way correspondent relationship between care homes and GP practices, named individuals who can take ownership and lead on system maintenance, cascade training and troubleshooting to help facilitate a more safe and effective medicines management process with regards to ordering. Empower GP practices and care homes with the necessary information to facilitate proxy/online ordering. Avoid the use of the term proxy ordering as this is often misunderstood, use the phrase online ordering of medicines or similar, to ensure your audience fully understand the process you are referring to. If you have a Quality Team within your organisation they can also support with discussions on proxy/online ordering during their contact with care homes. If there is an opportunity anywhere at any time to mention proxy/online ordering - shout about it! Key contact: Lizzie Atkinson, Medicines Optimisation Technician, Wakefield CCG. elizabeth.atkinson8@nhs.net Confirm internal approval from the organisations referred to in the case study: Yes
North West - William Blake House Registered Manager William Blake House: I have used the system today and all went well! What a huge time and resource saver this is going to be I love it! Thank you so much for helping us get to this point. Senior Care Leader St Peters Care Home: The last 2 month there has been no waste, all medication was carried forward Working well so far Some issues with staff accounts being locked, easily rectified by the practice after a conversation! Care Manager Howden Care Home: Going really well Issues being resolving quickly with the practice we have seen a reduction in overstock and waste
North West - Morecambe Bay CCG Background / Description of the part of the process the best practice covers. Medicines reconciliation between what was ordered previously via MAR charts with the community pharmacy driving the ordering process and what can be ordered now via proxy access with the surgery driving the process. Situation: (in other words what was the issue) Before setting up ordering via proxy access, ordering patient s medication was done using MAR charts that had been populated by items by the pharmacy. When this changed to ordering via proxy access and the items on the system being populated by the surgery, there seemed to be some discrepancies between what the care home thought the patient was meant to be taking and what the surgery had listed. What change did they want to bring about? The care home wanted the proxy access ordering information to match what they thought the patient was meant to be taking.
North West - Morecambe Bay CCG Solution and impact / benefits: When this first became apparent as an issue, the CSU liaised with the surgery and the care home to perform a medicines reconciliation on every patient. Where there were differences this was highlighted to the surgery. In some case it was simply moving regular medications from being acute to repeat on EMIS to allow then to be seen via proxy access ordering. Similarly making sure items which were used infrequently, didn t accidently more into past medications prematurely. Key learning points: To ensure successful implementation of ordering via proxy access, the correct medications must be able to be ordered to keep it as efficient a system as possible for the care home to want to continue to use it. Doing a medicines reconciliation throughout the care home before going live with proxy access ordering should remove issues of not being able to order all of a patient s medications. This can be done by the PCN pharmacy team if SMR s are done in the care homes in advance of the proxy access ordering going live. Key contact: Karen Wilson, NECS. Lead pharmacy technician on project in Morecambe Bay CCG. Email k.wilson14@nhs.net
North West - Cheshire Background / Description of the part of the process the best practice covers. The process of ordering medicines for care home residents can be an inefficient and long drawn out process. It usually begins three weeks before the medicines are required leading to medicines waste, and wasted time for all concerned during the month. It also adds to the carbon footprint if the care home or pharmacy have to drop off repeat slips at the GP practice. Situation: (in other words what was the issue) One particular care home hand wrote all the items they required each month onto a piece of A4. This was then dropped off at the practice and was processed and sent through to the dispensing pharmacy via EPS. Quite often items were ordered that weren t always required as it was quicker for the home to write all items required rather than list every item individually. What change did they want to bring about? Setting up the home with proxy ordering had a massive impact on the home. They were able to log into patient access and see the list of repeat medicines and just tick the items required. They reported the time spent on the monthly medicines order was reduced from one and a half days to four hours. Also, on average the amount of queries back to the practice and pharmacy were reduced from twenty to five per month. Solution and impact / benefits: Benefits have included a more streamlined process for the care homes, GP practices and pharmacy. It enables care home staff to spend more time with the residents rather than on the ordering process and chasing missing items, fewer phone calls to the practice and pharmacy. Care home residents now receive their medication in a timely manner. There is reduced footfall into the homes and GP Practice as everything is processed online, apart from when the pharmacy delivers the medicines. This has been particularly important during C19. The ultimate aim is to reduce the ordering time from 3 weeks to 2 weeks, leading to a further reduction in waste.
North West - Cheshire Feedback from care homes: Order what you need when you need it It sace Reallyorganised Key learning points: The care homes need extra support to set up the process, but once this is completed they see how easy it is to use the system and the benefits for everyone involved in the ordering process. Be aware there may be some housekeeping for the practice as the care home only see the list of repeat medicines. If some items are used regularly, it may be worth the practice adding these to variable repeat in the clinical system. Key contact: CCG MOCH Technician - Diane Sandbach diane.sandbach@nhs.net Station House Care Home - Amanda Hearn Amanda.Hearn@careuk.com Confirm internal approval from the organisations referred to in the case study: Yes
North West - West Lancaster Background / Description of the part of the process the best practice covers. Implementation in a care home Situation: (in other words what was the issue) The care home had not yet implemented proxy ordering What change did they want to bring about? To implement proxy ordering Solution and impact / benefits: The care home already had access to NHSmail and was aligned to a single GP, so we worked with the practice to successfully implement proxy ordering. The practice have also enabled proxy access to consultations for one member of care home staff, so she can view relevant information that they would have otherwise telephoned the surgery for. Key learning points: Alignment of a care home to a single GP practice has enabled the implementation of proxy ordering successfully and quickly. Key contact: Sam Russell s.russell9@nhs.net Confirm internal approval from the organisations referred to in the case study: Yes
South West - NHS Bristol, North Somerset & South Gloucestershire CCG Background / Description of the part of the process the best practice covers. Ordering medication with a reliable audit trail is really important for residents care home staff, this allows an effective and successful ordering procedure. Most care home in the area has different ways of recording interim and miscellaneous prescriptions, primarily on paper MAR charts. The success of this practice relies on each member of staff having to annotate on paper MAR charts. Situation: Audit trail for interim and miscellaneous prescription is very time consuming for care homes. Previously, care home staff will have to rely on what was recorded on the MAR charts, and if this task was not completed, care home staff was required to ring both the surgery and the community pharmacy to locate prescriptions. This was an inefficient use of time for the care home, the GP surgery and the resident. Consequently, it resulted in delaying the supply of medications and comprising resident s safety. What change did they want to bring about? We wanted to replace this way of working with proxy ordering to ensure that an efficient audit trail was in place. Hence, reduce the need to call both surgery and community pharmacies and ensure medication are supplied in a timely manner.
South West - NHS Bristol, North Somerset & South Gloucestershire CCG Solution and impact / benefits: As this was a widespread issue in our area, we suggested setting up proxy ordering in any quality or strategic meetings we had with care homes managers where similar issues have been raised. In addition, we recommended that the care homes should incorporate this new way of ordering to their standards operating procedures for ordering and medicines policy. Consequently, this had a major impact on resident s safety by receiving medication in time and using the care home staff time to optimise resident s care. Key learning points: Audit trail of medication is fundamental for resident s safety; proxy ordering provides an opportunity to address any issues that might result in delaying medication supply. Furthermore, the system provides an improved and easy to access audit trail, which saves time for care home staff to optimise residents care. Key contact: Gloucestershire CCG, Kassin.Yakhlef@nhs.net Kassin Yakhlef, Medicine Optimisation Pharmacy Technician, NHS Bristol, North Somerset and South Confirm internal approval from the organisations referred to in the case study: Yes
South West Devon CCG We are still early on in the process but are happy to share the process we have implemented so far: 1. In Devon CCG we chose to email all the GP Practices with the attached email to establish current use of proxy access or interest in proceeding. 2. Responses received were collated into a spreadsheet 3. Care homes using proxy access were contacted to confirm use and ask for feedback / share learning 4. Interested GP Practices were contacted and offered an individual Teams meeting to discuss NHS England website and resources provided 5. After Teams meeting a next steps email was sent to the GP Practice to encourage contacting the care homes and starting the process 6. GP Practices have been implementing proxy with minimal CCG support only contacting us when issues arise or advice required 7. Regular contact with GP Practices is made via email to ensure project on track and progress is being made Learning points Use resources available on the NHS England proxy access website next steps, FAQs and downloadable resources in particular Proxy access role out easier where there is an embedded Technician or Pharmacist / Administrator at the GP Practice who takes on the responsibility of the project Local issue occurred with whether a DPIA was required as well as an DSA still causing a delay in role out Key contact: Karen Northcottkarennorthcott@nhs.net and Carys Shepley carysshepley@nhs.net
South West Sound PCN Background / Description of the part of the process the best practice covers. The ordering process of medicines was already an inefficient process, but with the removal of the fax machine there were additional inefficiencies and medicine waste from Care homes. Having a background in pharmacy, I was driven to support the management of care home residents medicines more effectively to benefit both the system and the staff in the home. Situation: Having multiple conversations with the homes and managing complaints around missing items, new medicines and multiple orders, we went through the process of aligning the medications and supporting the nursing staff access to order via proxy on behalf of the patients. Solution and impact / benefits: Visibility of what has been requested and where it is in the process Reduction in emails and calls from the care home to the surgery for routine medications Audit trail for altered and ceased medication Reduces Admin workload in the practice and care home A simple process with no additional technical requirements on care homes, GP practice and community pharmacies Key Learning points It was very easy for the care home to revert to a paper process when they struggled with logins so make sure you support them for a few months until the process is embedded. Key contact: Sarah Giles, Elm Surgery s.giles2@nhs.net