Hypersensitivity Reactions and Classification
Hypersensitivity reactions occur in sensitized hosts following contact with specific antigens, leading to injurious consequences. The Gell and Coombs Classification categorizes reactions into Type I, II, III, and IV based on immune response and duration. Type I reactions are immediate and humoral, while Type IV reactions are delayed and cell-mediated. Different manifestations and examples illustrate the impact of hypersensitivity reactions on various bodily systems.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Definition Definition Injurious consequences in the sensitised host, following subsequent contact with specific antigens.
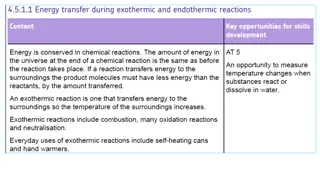
Gell Gell and Coombs Classification and Coombs Classification Type- I Type- II Type- III Type- IV Immune response altered Humoral Humoral Humoral Cell mediated Immediate or delayed Immediate Immediate Immediate Delayed Duration between appearance of symptoms & antigen contact 2min to 30 min 5-8 hrs 2-8 hrs 24 to 72 hrs
Gell Gell and Coombs Classification and Coombs Classification Type- I Type- II Type- III Type- IV Antigen Soluble Cell surface bound Soluble Soluble or bound Mediator IgE IgG Ag-Ab complex TDTH cell Effector mechanism Mast cell degranulation 1. ADCC 2. Complement mediated cytolysis Complement activation and inflammatory response Macrophage activation leads to phagocytosis or cell cytotoxicity Desensitization to the allergen Easy, but short lasting Easy, but short lasting Easy, but short lasting Difficult but sustained
Gell Gell and Coombs Classification and Coombs Classification Type- I Type- II Type- III Type- IV Typical manifestations 1.Anaphylaxis 2.Asthma 3.Atopic dermatitis 1.Transfusion reactions 2.Rh incompatibility 3.Hemolytic anemia 1.Arthus reaction 2.Serum sickness 3.Glomerulonephtiriti s 4.Rheumatoid arthritis 1.Tuberculin test 2.Granuloma formation in tuberculosis, leprosy, etc 3.Contact dermatitis
Immediate hypersensitivity reactions Immediate hypersensitivity reactions Occur immediately, within few minutes to few hours of antigen contact, as a result of abnormal exaggerated humoral response (antibody mediated). Further classified into three types: oType- I hypersensitivity reaction oType- II hypersensitivity reaction oType- III hypersensitivity reaction
Delayed hypersensitivity reaction Delayed hypersensitivity reaction Occurs after few days of antigen contact, as a result of abnormal cell mediated immune response. Also called as type- IV hypersensitivity reaction.
TYPE TYPE- - I HYPERSENSITIVITY REACTION I HYPERSENSITIVITY REACTION Hallmark - Production of IgE by sensitized B cells following a contact with an allergen which inturn induces mast cell degranulation. These changes ultimately lead to: oLocalized response (called atopy) oSystemic response (called anaphylaxis).
Allergens that induce type Allergens that induce type- -I hypersensitivity reaction I hypersensitivity reaction Food Nuts, egg, peas, sea food, beans, milk Plants & pollens Rye grass, rag weed, timothy grass Proteins Foreign serum Vaccines Drugs Penicillin, sulphonamides, local anesthetics and salicylates Insect bite products Venom of Bee, Wasp, Ant,Cockroach calyx and Dust mites Others Mold spores, animal hair and dander
Experiments to demonstrate Experiments to demonstrate type I hypersensitivity reaction type I hypersensitivity reaction P-K reaction Schultz Dale phenomenon Theobald smith phenomenon
P P- -K reaction K reaction- - K.Prausnitz and H.Kustner (1921). Injected serum from an allergic person into a nonallergic individual intradermally. when the appropriate antigen was injected at the same site, a wheal and flare reaction (analogous to hives) developed at the site first to demonstrate - antibodies in the serum are responsible for the allergy and it is transferable from one person to another.
P P- -K reaction K reaction- - Wheal and flare response occurs in three stages: oAppearance of an erythematous area at the site of injury. oDevelopment of a flare (erythema) surrounding the site. oWheal (swelling & congestion) forms at the site as fluid leaks under the skin from the surrounding capillaries.
Schultz Dale phenomenon Schultz Dale phenomenon Demonstrate anaphylaxis in vitro. By exposing isolated tissues such as intestine or muscle segments of sensitized guinea pigs to the allergens.
Mechanism of type I hypersensitivity Mechanism of type I hypersensitivity Sensitization phase Effector phase oBoth occurring with an interval of 2-3 weeks.
Sensitisation phase Sensitisation phase- Sensitisation is most effective - allergen is introduced parenterally but may occur by any route, including ingestion or inhalation. In susceptible individuals, very minute doses can be sufficient to sensitise the host. Allergen is processed by the antigen presenting cells and the antigenic peptides are presented to the CD4 helper T cells.
Sensitisation phase Sensitisation phase- Activated THcells are differentiated into TH2 cells which in turn secrete interleukin 4 induces the B cells to differentiate into IgE producing plasma cells and memory cells. Secreted IgE migrate to the target sites, and coat on the surface of mast cells and basophils. Fc region (the CH3 and CH4 domains) of IgE binds to high affinity Fcreceptors (e.g. Fc R1) present on mast cell surface. Such sensitized mast cells (coated with IgE) will be waiting for interaction with the subsequent antigenic challenge.
Effector phase Effector phase When the same allergen is introduced subsequently (shocking dose), it directly encounters with the Fab region of IgE coated on mast cells. IgE Cross linkage initiates degranulation-Allergen bound to IgE triggers the mast cells (and basophils) activation and degranulation. Granules in turn release a number of pharmacologically active chemical mediators that lead to the various manifestations of type-1 reaction. The memory B cells further differentiate into plasma cells that supply the IgE.
Effector phase Effector phase Degranulation in two phases: oPrimary mediators- The preformed chemical mediators which are already synthesized by mast cells, are immediately released. Primary Mediators Histamine, Heparin and Serotonin Eosinophil chemotactic factor (ECF-A) Neutrophil chemotactic factor (NCF-A) Proteases Action Vascular permeability Smooth-muscle contraction Eosinophil chemotaxis Neutrophil chemotaxis Bronchial mucus secretion; Degradation of blood-vessel basement membrane
Effector phase Effector phase oSecondary mediators are those which the mast cells synthesize and release Secondary Mediators Platelet-activating factor Action Platelet aggregation and degranulation; Contraction of pulmonary smooth muscles Vascular permeability; Contraction of pulmonary smooth muscles Leukotrienes (slow reactive substance of anaphylaxis, SRS-A) Prostaglandins Vasodilation; Contraction of pulmonary smooth muscles; Platelet aggregation Bradykinin Cytokines (IL-1 and TNF- ) Vascular permeability; Smooth-muscle contraction Systemic anaphylaxis; Expression of cell adhesion molecules (CAMs) on venular endothelial cells
Effector phase Effector phase Pharmacological actions: oChemical mediators - bronchial and other smooth muscle contraction, increased vascular permeability and vasodilation. Symptoms: Breathlessness, hypotension and shock leading to death at times.
Manifestations of Type Manifestations of Type- -I Reaction Immediate Manifestations Immediate Manifestations I Reaction- - Systemic anaphylaxis: oAcute medical emergency condition, characterized by severe dyspnoea, hypotension, and vascular collapse leading to death. oOccurs within minutes of exposure to allergen and unless treated promptly, may lead to fatality. oEpinephrine (adrenalin) is the drug of choice for systemic anaphylactic reactions.
Localized anaphylaxis (atopy) Localized anaphylaxis (atopy) Reaction is limited to a specific target tissue or organ, mostly the epithelial surfaces at the entry sites of allergen. These allergies afflict more than 20% of people. Almost always run in families (i.e. inherited) Examples include: oAllergic rhinitis (or hay fever): Most common atopic disorder. Affects 10% of the population. Results from exposure to airborne allergens with the conjunctiva and nasal mucosa leading to appearance of various symptoms such as watery secretions of the conjunctiva, nasal mucosa, and upper respiratory tract, as well as sneezing and coughing.
Localized anaphylaxis (atopy) Localized anaphylaxis (atopy) oAsthma: Second most common atopic manifestation. Differs from hay fever in involvement of lower respiratory mucosa, resulting in contraction of the bronchial smooth muscles and airway edema, mucus secretion; all together leading to bronchoconstriction and dyspnoea. The stimulus may or may not be an allergen. Accordingly asthma can be classified as- Allergic asthma- Induced by airborne or blood-borne allergens, such as pollens, dust, fumes, insect products, or viral antigens. Intrinsic asthma- It is independent of allergen stimulation; induced by exercise or cold.
Localized anaphylaxis (atopy) Localized anaphylaxis (atopy) oFood allergy oAtopic dermatitis (allergic eczema) oDrug allergy- Various drugs (such as penicillin, sulphonamides, etc.) may produce type-I hypersensitivity responses which may be either local reactions or even sometimes produce systemic anaphylaxis.
Manifestations of Type Manifestations of Type- -I Reaction Late Late Manifestations Manifestations I Reaction- - Mediators: oReleased in acute induce recruitment of various inflammatory cells such as neutrophils, eosinophils, macrophages, and lymphocytes etc. oAmong the infiltrates, eosinophils and neutrophils predominate; each accounting for 30% of the total inflammatory cells influx.
Manifestations of Type Manifestations of Type- -I Reaction Late Late Manifestations Manifestations I Reaction- - Eosinophil influx: oFavoured by ECF (eosinophil chemotactic factor), IL-5 and GM- CSF. oEosinophils express Fcreceptors for IgG & IgE and thus bind directly to antibody-coated allergens. oCauses release of toxic granules from eosinophils which contribute to the chronic inflammation of the bronchial mucosa that characterizes persistent asthma.
Manifestations of Type Manifestations of Type- -I Reaction Late Late Manifestations Manifestations I Reaction- - Neutrophil infiltration: oInduced by NCF (neutrophil chemotactic factor), and other cytokines such as IL-8. oActivated neutrophils release various mediators which further potentiates inflammatory tissue damage and thickening of basement membrane.
Factors influencing type I hypersensitivity Factors influencing type I hypersensitivity Genetic makeup Allergen dose: oDose of the allergen has a definite impact on the type of immune response produced. TH1 vs TH2 response
Detection of type I hypersensitivity Detection of type I hypersensitivity Skin prick test: oAdvantage- Skin test is relatively inexpensive and allows screening of a large number of allergens at one go. oDisadvantage- It may occasionally sensitize the individual to new allergens and in some rare cases may induce late-phase reaction or even systemic anaphylactic shock.
References Textbook of Medical Microbiology by Ananthnarayan, Paniker Textbook of Medical Microbiology by Satish Gupte Textbook of Medical Microbiology by S. Bhat, A.S.Sastry Textbook of Medical Microbiology by D.R.Arora, Brij bala Arora
 undefined
undefined