Functions of the Placenta in Pregnancy
The placenta plays crucial roles in pregnancy, facilitating gas exchange, nutrient transfer, hormone production, and immune protection for the fetus. It also mediates Rh isoimmunization, a condition potentially affecting the fetus due to Rh incompatibility.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
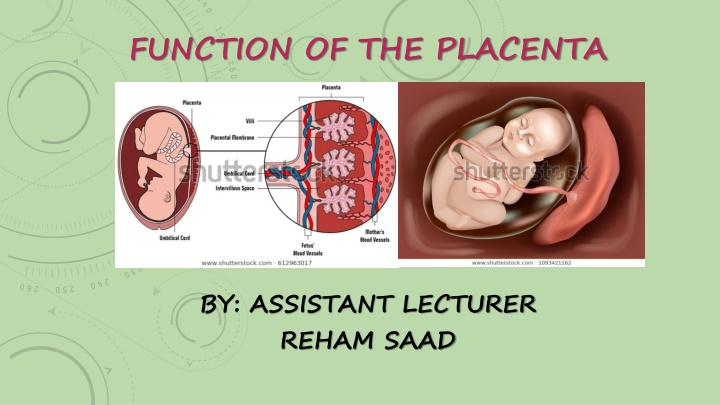
FUNCTION OF THE PLACENTA BY: ASSISTANT LECTURER REHAM SAAD
FUNCTION OF THE PLACENTA 1. Exchange of gases, Such as oxygen , carbon dioxide, carbon monoxide, is accomplished by simple diffusion. 2. Exchange of nutrients and electrolytes, such as amino acids, free fatty acids, carbohydrates, and vitamins, is rapid and increase as pregnancy advance. 3. Transmission of maternal IgG 7S antibodies to the fetus; and thus providing passive immunity for the fetus to some infectious diseases except chickenpox and whooping cough. This passive immunity supports the newborn for a short time after birth.
FUNCTION OF THE PLACENTA 4. Hormone production; the syncytial trophoblast synthesized the following: The placenta produces an increasing amount of estrogen until labor, this estrogen stimulates the growth of the uterus and the breast. The placental lactogenic (somatomammotropin), this hormone makes the mother diabetogenic and gives the fetus priority to maternal blood sugar. Also, this hormone promotes the development of the breast.
FUNCTION OF THE PLACENTA During the 1st and 2nd months of pregnancy, the placenta secrets the human chorionic gonadotropin (hCG) that maintain the corpus luteum secreting progesterone and estrogen until the 4th month. Detection of this hormone exerted in the urine of the mother is used to diagnose early pregnancy. At the end of the 4th month; the placenta produces progesterone to maintain the implantation in the endometrial mucosa. Before this, the progesterone is secreted by the corps luteum that generate after the 4th month.
Rh isoimmunization (Rh incompatibility) 1. If the father blood is Rh+ve, 2. and the mother is Rh-ve, 3. the fetus blood may be Rh+ve. Fetal blood invade the maternal circulation during pregnancy and at labor via the placenta and thus creating an immune response in the mother resulting in the formation of maternal antibodies to Rh+ve RBC. These antibodies may be transmitted to the fetus across the placenta in the same pregnancy or in the subsequent pregnancy and causing hemolysis of the Rh+ve fetal RBC.
Rh isoimmunization (Rh incompatibility) This is a fatal condition called erythroblastosis fetalis, it could be diagnosed by spectrophotometric examination of the aspirated amniotic fluid to detect the level of antiRh+ ve antibodies. The treatment is either by: a. intra-peritoneal blood transfusion to the fetus inside the uterus b. or by exchange transfusion after birth.
Rh isoimmunization (Rh incompatibility) To prevent this disease: The mother should receive an intramuscular injection of anti Rh+ve antibody called anti-D injection 3 days after birth. The injected antibodies hemolysis the Rh+ve fetal blood entering the maternal circulation massively at birth and thus preventing the sensitization of the maternal immunity by the Rh+ve fetal blood and so causes no antibodies production.
The umbilical cord and amnion The cephalocaudal and lateral folding of the embryonic disk during the 2nd month of development lead to the formation of a ring at the junction of the amnion and the ectoderm. This ring is called the primitive umbilical ring that contains the following:
The umbilical cord and amnion 1. The connecting stalk containing the allantois and two umbilical arteries and one umbilical vein. 2. The vitelline duct of the yolk sac or called the yolk sac stalk containing the vitelline vessels. 3. A canal connecting the intra-embryonic cavity with the extra-embryonic cavity.
The umbilical cord and amnion The amniotic cavity is enlarged to fill the extra-embryonic chorionic cavity at the end of the 3rd month of pregnancy. This will lead to obliteration of the yolk sac in the chorionic cavity; also the enlarged amnion compresses the contents of the primitive umbilical ring and enclosing them to form the primitive umbilical cord which contains: A. Distally; the vitelline duct and umbilical vessels. B. Proximally; the allantois and a loop of the intestine that herniated in the umbilical cord because of the small abdominal cavity. This hernia is called the physiological umbilical hernia that withdrawn into the abdomen at the end of the third moth.
The umbilical cord and amnion The allantois and the vitelline duct and vessels obliterate in the full term umbilical cord, therefore; the mature cord contains only the umbilical vessels surrounded by the proteoglycan material called Wharton jelly that protect the vessels. The walls of the umbilical arteries are rich with muscular and elastic tissue to be contractible after birth.
Features of the normal full term umbilical cord 1. 2cm in diameter. 50cm in length. Longer cord may encircle the fetal neck, and shorter cord pulls the placenta during delivery. 2. Tortuous causing false knots. 3. Contains two arteries and one vein. Vascular abnormality of the cord may be associated with cardiovascular anomalies.
Features of the normal amniotic fluid: This fluid produced by the amniotic cells but is derived from the maternal blood. 1.clear and watery. 2.about 30ml at 10 weeks, 350 at 20 weeks, 800-1000ml at birth. The fetus swallow about half of the fluid in each day, also the fetus urinate water in the amniotic fluid since the 5th month, the fluid is replaced every 3hours.
Features of the normal amniotic fluid: The amniotic fluid 1. Protects the suspended fetus. 2. Absorb jolts. 3. Allow fetal movement by preventing adhesion of the fetus with the amnion. 4. During birth the amniotic configuration act as a hydrostatic wedge to dilate the birth canal.
The Twins Twins are of two types: A. Dizygotic twins (fraternal): they fertilization having the following criteria: 1.They differ in genes and so are dissimilar to each other in shape and may be in sex. result from two the ova, of
The Twins 2. Each has its own implanted site and its own placenta, amnion, and chorion. 3. Sometimes the two placenta or the chorionic sac may be near together and fused, fusion of the placental may cause exchange of the blood groups of the fetus and is called erythrocyte mosaicism.
The Twins B.Monozygotic twins (identical): they result from splitting of the fertilized ova or zygote development. The splitting occurs: at any stage during the 1. At two cells stage; resulting in two separate separately, each has its own placenta, amnion and chorion. Both embryos develop the same blood group, finger print, sex, and external appearance. embryos that implanted
The Twins 2. At inner cell mass of the blastocyst stage; both embryos have the same placenta and chorion, but each of them has its own amnion. 3. At the bilaminar germ disc; both embryos have the same placenta, amnion, and chorion.