Antepartum Haemorrhage and Placenta Praevia
Antepartum haemorrhage, especially in cases of placenta praevia, can present challenges in pregnancy. This condition, where the placenta covers or is near the cervix, requires careful monitoring and may necessitate interventions like ultrasound scans and potential hospital admissions. Risk factors for placenta praevia include scarred uterus, advanced maternal age, and previous instances of the condition. Management strategies should be tailored to each patient's situation, considering factors like proximity to the hospital and maternal well-being.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Clinical Scenario 40 y/o Para 2 presents at 27 weeks with painless bleeding. Told at anomaly scan had a low lying placenta What more would you like to know from the history? What further examinations or Investigations should she have at this point?
Bleeding settled by time arrives. Small amount of fresh red blood. Patient stable. Hb 119 Rhesus positive. CTG normal. No signs of labour. Differential diagnoses?
Ultrasound Ultrasound shows posterior placenta overlying cervical os Otherwise normal Diagnosis: PLACENTA PRAEVIA
Placenta Praevia Definition: Placenta completely covers the cervical os and is in front of the presenting part of the fetus Low-lying placenta if the placental edge is <2 cm from the cervical os Occurs in 0.3% to 0.5% of pregnancies worldwide >50% of women with PP will present with bleeding in 2nd half of pregnancy
Placenta Praevia Many low-lying placentas migrate during pregnancy and resolve spontaneously. If detected at the routine anatomical scan and no significant bleeding, repeat ultrasound at 32 weeks. If the placenta is now in normal position, no further investigations needed. If a low-lying/ PP is detected, it is very unlikely to resolve spontaneously Arrange further ultrasound for 36 weeks to aid delivery planning.
Risk factors for Placenta Praevia True/False Scarred uterus Advanced maternal age Smoking Illicit drug use Short inter-pregnancy intervals Prior PP Infertility treatment First pregnancy
Management How should this patient be managed? Should this patient be admitted? Patient says she cannot stay as has 2 other children to look after. She only stays 2 miles from the hospital. What advice should be given? Does this patient require Anti-D?
Second Presentation Patient presents again at 36+1 with painless heavy fresh red PV loss Due for elective C/S next week How should this patient be managed now?
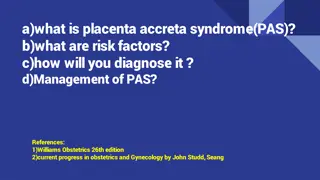
Placenta Praevia: Associated Conditions chorionic villi invade into the myometrium Placenta Accreta chorionic villi invade through the myometrium and sometimes into adjoining tissue Placenta Increta chorionic villi attach to the myometrium, rather than being restricted within the decidua basalis Placenta Percreta
Vasa Previa Occurs when fetal vessels run through the free placental membranes, unprotected by placental tissue or Wharton s jelly of the umbilical cord. Likely to rupture in active labour Especially when located near/ over the cervix, under the fetal presenting part.
Vasa Praevia diagnosis May be diagnosed during early labour by VE - detecting pulsatile fetal vessels inside the internal os Or by dark-red vaginal bleeding and acute fetal compromise after spontaneous or artificial rupture of membranes. Antenatally bu U/S
Management Vasa Previa Because of the speed at which fetal exsanguination can occur delivery should not be delayed while trying to confirm the diagnosis Especially if of fetal compromise on CTG The ultimate management goal of confirmed vasa praevia should be to deliver before rupture of membranes while minimising the impact of iatrogenic prematurity. planned caesarean delivery at 34 36 weeks of gestation is reasonable in asymptomatic women. Administration of corticosteroids for fetal lung maturity recommended from 32 weeks of gestation due to increased risk of preterm delivery.
Summary Placenta Praevia Low lying placenta covering/partially covering cervical os Risk factors- advanced age, smoking, uterine surgery,IVF Usually presents with painless fresh bleeding. Mx- USS monitoring and Elective LUSC. Other causes APH Abnormal Placentation (accreta, increta, percreta) Vasa praevia