Managing Chronic Kidney Disease in Pregnancy: A Case Study
This case study discusses the management of Chronic Kidney Disease in pregnancy, focusing on a patient with severe anemia and the need for medical termination of pregnancy. The patient underwent blood transfusion and medical termination, followed by post-evacuation monitoring and counseling on sterilization and follow-up care. Key points highlight the importance of a multidisciplinary approach and the impact of pre-pregnancy renal function on outcomes. Learning objectives include pre-conception, antenatal, and postnatal care in women with CKD. The definition of CKD is also provided.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
CKD in Pregnancy Dr. Shaista Mehmood PGR Gynae Unit-1
Management We received call from Female Medical Unit for this patient with plan of Medical Termination of Pregnancy (As advised by Nephrologist) Patient was shifted to Labour Room with the diagnosis of Chronic Kidney Disease with Severe Anemia (Hb-6) & fetus of Gestational Age of 19 weeks on USG. Our plan was to first optimize Hemoglobin levels of patient and then plan TOP We transfused 3 units of blood and then medical termination was started with Tab. Misoprostol and after 2nd dose of Misoprostol, patient went into labour and delivered FSB fetus followed by ERPC
Her post evacuation scan was done which showed no retained products of conception Patient was kept under observation to monitor for PV bleeding Patient was counselled regarding need for sterilization in the form of BTL and need of follow up from Nephrologist for her CKD management Patient was shifted back to FMU-1 for further management We further followed the patient in Medical Unit-1 for postnatal monitoring but on the next day of TOP, patient Left Against Medical Advice from Medical Unit-1
Chronic Kidney Disease in Pregnancy
Learning Objectives To understand the basic principles in pre- conception care, Antenatal care and postnatal care of women with CKD To be aware of risks to pregnancy as well as long term renal function
Key Points A multidisciplinary team should manage pregnancy in women with CKD The outcome is dependent upon pre-pregnancy renal function and the presence of hypertension and proteinuria Women on dialysis and renal transplant recipients form a special group that needs expert care during pregnancy
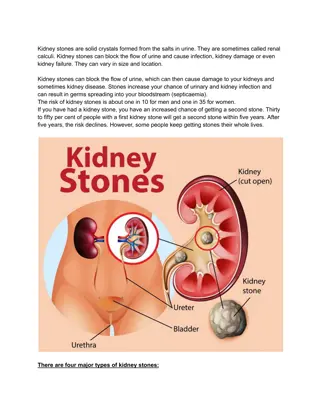
Definition CKD is defined as either kidney damage or Glomerular Filtration Rate (GFR) < 60ml/min/1.73m(2) for 3 months or more, irrespective of cause. Kidney damage is defined as pathologic abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies.
Physiological changes to kidneys during healthy pregnancy
I have kidney disease. Can I become pregnant??
Mild renal impairment Stage 1 & 2 Serum creatinine <1.4mg/dl Tolerate pregnancy well Moderate renal impairment Stage 3 Serum creatinine 1.4-2.8mg/dl Increased risk of permanent loss of function during and after pregnancy 50% will have permanent decline in function 35% will have ESRD Pregnancy is not advised & should not be continued Severe renal impairment Stage 4 & 5 Serum creatinine >2.8mg/dl *Source: Dewhurst s
Four factors determine outcome in CKD. 1. Type of CKD 2. Associated hypertension 3. Baseline serum creatinine levels 4. Degree of proteinuria
Pregnancy is possible in all phases of chronic kidney disease (CKD), but its management may be difficult and the outcomes are not the same as in overall population. Normal or mild renal impairment with persistent protein in urine affects up to 3%of women of child bearing age (20-39 years). Stage 3-5 (GFR <60ml/min or creatinine levels >1.5mg/dl) affect around 1 in 150 women of child bearing age but because of reduced fertility and an increased rate of early miscarriage, pregnancy in these women is less common.
I am Pregnant and I have CKD Can pregnancy affect my kidneys??
Adverse kidney outcomes in pregnancy Worsening of kidney functions - Stage 1 7.6% - Stage 4,5 >50% Worsening proteinuria Uncontrolled Blood pressure High chances of pre-eclampsia. If pre-eclampsia develops, maternal renal function deteriorates further
Adverse Pregnancy outcomes To the Baby To the Mother Spontaneous Miscarriages Urinary Tract Infections IUGR Pre-Eclampsia Low birth weight Preterm Delivery Stillbirths Caesarean delivery Neonatal Unit Admission Neonatal Mortality
Management of patient with CKD in pregnancy
Before Pregnancy Awareness regarding the long term risks to the renal function and to the fetus before they conceive Women with CKD have amenorrhea but may still occasionally ovulate and thus conceive Should conceive after consultation with Nephrologist & Obstetrician Folic Acid 400 micrograms should be given before conception until 12 weeks gestation Feto toxic drugs such as ACE inhibitors and Angiotensin-2 receptor blockers should be stopped before pregnancy
Obstetric Management Follow up with nephrologist, obstetrician and fetal medicine expert. Folic acid supplementation Early Dating scan to estimate gestational age accurately Anomaly scan detailed scan of urinary tract to look for evidence of inherited conditions such as obstructive uropathy Regular scan every 4 weeks from 28 weeks check growth and liquor volume Prophylactic low dose Aspirin for prevention of Pre-Eclampsia Blood pressure monitoring and control - Not higher than 140/90mmHg -Methyldopa, calcium channel blockers, hydralazine and labetalol safe
Early detection of Anemia & correction Preterm Labour is common. Prompt treatment of bacterial vaginosis and UTI including asymptomatic bacteriuria can be helpful in prevention of preterm labour Women with nephrotic syndrome should receive prophylactic heparin in pregnancy and 6 weeks postpartum Delivery should be planned at term or near term Early delivery for obstetric indications like pre-eclampsia and IUGR or rapidly deteriorating renal function. Caesarean section is only recommended for obstetric indications
Postpartum Breast feeding Contraception counselling - Progesterone only methods highly effective and safe alternatives (mini pills, implant, mirena) - IUCD ( no more increased risk of pelvic inflammatory disease) -Combined Oral Contraceptives can cause hypertension and thromboembolism. Follow up with Nephrologist
Indications of Acute Dialysis during pregnancy Severe refractory metabolic acidosis Electrolyte imbalance, especially severe refractory hyperkalemia Volume overload leading to congestive heart failure Pulmonary edema that is unresponsive to diuretics Dialysis may be initiated earlier in pregnancy if there is an acute deterioration in renal function because of increased risk of fetal demise
Pregnancy in women on Chronic Dialysis Frequency of pregnancy on chronic dialysis increasing, 1-7% Conception likely with residual renal function and those beginning dialysis Incidence of pregnancy is lower on peritoneal dialysis than on hemodialysis Spontaneous miscarriage is common, 21% reaching the second trimester Preterm delivery is common Mean gestational age of delivery is 32 weeks contributing to low infant survival rate Perinatal outcome is better in those who conceive prior to starting dialysis than those who conceive after dialysis
Protein intake increased to 1.5g/kg/day on hemodialysis and 1.8g/kg/day on peritoneal dialysis Weight gain 0.5kg/week Calcium replacement 1.5g/day achieved by high calcium dialysate. Measurement of 25-hydroxy vitamin D levels each trimester and supplementation if low Dialysis-high phosphate levels but if low oral phosphate supplements Folate dose of 5mg/day Vitamin C, thiamine, niacin and vitamin B6 supplementation
Management of Hemodialysis Frequency of dialysis increased to at least 20 hours per week Aim to maintain predialysis urea levels of 15-20 mmol/L. Maternal volume depletion and hypotension avoided and biocompatible, smaller surface area dialyzer to reduce ultrafiltration rate per treatment. Maternal Diastolic blood pressure 80-90 mmHg Bicarbonate and Potassium in dialysate adjusted based on serum chemistries to avoid electrolyte imbalance that can result of more frequent dialysis.
Management of Peritoneal Dialysis Continued safely during pregnancy Increased number of exchanges during pregnancy and fill volumes of peritoneal dialysis fluid that may need to be reduced to 1-1.5L. Its is more practical to do this by switching to automated peritoneal dialysis As pregnancy progresses, size of enlarging uterus it may become impossible to continue with peritoneal dialysis and there should be a switch to hemodialysis Possibility of peritonitis exists
Pregnancy in Renal Transplant Recipients 12% of transplanted women of childbearing age and number of kidney transplant recipients who conceive seems to be increasing Miscarriage rate, congenital anomalies similar to general population 95% of gestations end successfully Ectopic pregnancy higher related to adhesions from previous surgery and peritoneal dialysis Hypertension 70% of the transplant recipients Superimposed pre-eclampsia and UTI 40% Acute bacterial pyelonephritis and gestational diabetes risk Incidence of preterm delivery, Preterm premature rupture of membranes is high 60%