Diagnostic Investigation for Respiratory TB in a Young Adult
Mrs. Peacock, a non-smoking 30-year-old woman with chronic cough, malaise, fever, and weight loss, presents with an enlarged neck lymph node. Following NICE guidelines, the next diagnostic steps involve chest x-ray, sputum samples for microscopy and culture, and possible bronchoscopy before starting treatment for suspected TB. Primary TB commonly presents with mediastinal or hilar enlargement, reflecting a common radiological manifestation. Consolidation, lymphadenopathy, pleural effusion, and caseating granuloma are key features of primary TB diagnosis.
Uploaded on Oct 02, 2024 | 1 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
SCE Questions Ruth Sobala ST4 24/06/20
Mrs Peacock is a 30 year old lady who presents to clinic with a chronic productive cough, general malaise, fever, and weight loss. On examination she had an enlarged neck lymph node. She has never smoked but recently returned from a three month trip visiting volunteering in a local school in India. What is the next diagnostic investigation in accordance with NICE Guidelines? a) Chest x-ray b) Sputum Samples c) Bronchoscopy d) Pleural Biopsy
Mrs Peacock is a 30 year old lady who presents to clinic with symptoms of a chronic productive cough, general malaise, fever, and weight loss. On examination she had an enlarged neck lymph node. She has never smoked but recently returned from a three month trip visiting volunteering in a local school in India. What is the next diagnostic investigation In accordance with NICE Guidelines? a) Chest x-ray b) Sputum Samples (3 x deep cough samples) c) Bronchoscopy d) Pleural Biopsy
NICE guidance recommends that to diagnose active respiratory TB you should: Arrange for the patient to have a posterior-anterior chest x ray. If the appearance of the chest x ray is suggestive of TB the patient should have further tests, eg microscopy and culture of sputum. Send multiple samples of sputum microscopy (three deep cough samples, preferably with one early morning sample), and culture for suspected respiratory TB. If possible, clinicians should send samples before starting treatment, or failing that, within seven days of starting treatment in patients with life threatening disease. Obtain sputum samples that have been spontaneously produced by deep cough if possible, otherwise clinicians should use induction of sputum or bronchoscopy in adult patients. Start treatment without waiting for culture results if there are clinical signs and symptoms consistent with a diagnosis of TB.
Which features is most commonly seen in primary TB: a) Consolidation b) Lymphadenopathy c) Pleural Effusion d) Caseating granuloma
Which features is most commonly seen in primary TB: a) Consolidation b) Lymphadenopathy c) Pleural Effusion d) Caseating granuloma
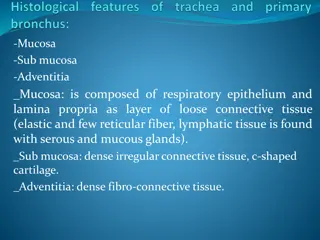
Mediastinal and/or hilar enlargement occurs in 10-43% of adults and is the most common radiological manifestation of primary TB. Most commonly effected areas are the right paratracheal and hilar lymph nodes. Lymphadenopathy typically demonstrates a low-attenuation center with peripheral rim enhancement on CT due to central caseous necrosis with peripheral granulomatous inflammatory tissue. Consolidation occurs in segmental or lobar distribution and can take up to 2 years to show resolution, or have residual opacities. Pleural effusion seen in approx 25% of cases are are usually unilateral. Airway disease such as bronchial stenosis occurs between 10-40%
Mrs Peacocks chest x ray is suggestive of TB and she has a positive sputum smear. She is diagnosed with tuberculosis. What treatment regimen should she be commenced on? a) Isoniazid (with pyridoxine), rifampicin, pyrazinamide and ethambutol for 2 months then isoniazid (with pyridoxine) and rifampicin for a further 10 months. b) Rifampicin, isoniazid (with pyridoxine) and pyrazinamide for 2 months then Rifampicin and isoniazid (with pyridoxine) for 4 months c) Isoniazid (with pyridoxine), rifampicin, pyrazinamide and ethambutol for 2 months then isoniazid (with pyridoxine) and rifampicin for a further 4 months. d) Isoniazid (with pyridoxine), rifampicin, pyrazinamide and ethambutol for 4 months then ethambutol and rifampicin for a further 2 months.
Mrs Peacocks chest x ray is suggestive of TB and she has a positive sputum smear. She is diagnosed with tuberculosis. What treatment regimen should she be commenced on? a) Isoniazid (with pyridoxine), rifampicin, pyrazinamide and ethambutol for 2 months then isoniazid (with pyridoxine) and rifampicin for a further 10 months. b) Rifampicin, isoniazid (with pyridoxine) and pyrazinamide for 2 months then Rifampicin and isoniazid (with pyridoxine) for 4 months c) Isoniazid (with pyridoxine), rifampicin, pyrazinamide and ethambutol for 2 months then isoniazid (with pyridoxine) and rifampicin for a further 4 months. d) Isoniazid (with pyridoxine), rifampicin, pyrazinamide and ethambutol for 3 months then ethambutol and rifampicin for a further 4 months.
For people with active TB without central nervous system involvement, offer: Isoniazid (with pyridoxine), rifampicin, pyrazinamide, and ethambutol for two months, followed by isoniazid (with pyridoxine) and rifampicin for a further four months. Isoniazid can cause peripheral neuropathy and is given with vitamin B6 (pyridoxine) to reduce the risk. Clinicians should offer fixed dose combination tablets as part of any TB treatment regimen, with a daily dosing schedule.
For people with active TB of the central nervous system, offer: isoniazid (with pyridoxine), rifampicin, pyrazinamide and ethambutol for 2 months then isoniazid (with pyridoxine) and rifampicin for a further 10 months. Dexamethasone (reducible course over 4-8 weeks).
Mrs Peacock lives alone and works as a baker. She took a flight to return home from India 2 weeks ago. You contact the relevant bodies so that contact tracing can occur. Which of the following would require inform and advice information to be sent out to the airline passengers? a) Less than 4 months have elapsed since the flight and the index case was smear-positive for multi drug-resistant TB. b) Contact tracing only needs to take place if the index case is an aircraft crew member. c) Less than 3 months has elapsed since the flight and the flight was longer than 8 hours and the index case is smear-positive and the index case coughed frequently during the flight. d) Contact tracing never needs to be carried out on fellow airline passengers.
Mrs Peacock lives alone and works as a baker. She took a flight to return home from India 2 weeks ago. You contact the relevant bodies so that contact tracing can occur. Which of the following would require the airline to provide inform and advice information to be sent out to its passengers. a) Less than 4 months have elapsed since the flight and the index case was smear-positive for multi drug-resistant TB. b) Contact tracing only needs to take place if the index case is an aircraft crew member. c) Less than 3 months has elapsed since the flight and the flight was longer than 8 hours and the index case is smear-positive and the index case coughed frequently during the flight. d) Routinely contact tracing does not need to be carried out on fellow passengers.
Following a diagnosis of tuberculosis in an aircraft traveller, healthcare professionals should not routinely perform contact tracing of fellow passengers. However, the notifying clinician should inform the relevant professional in health protection if: Less than three months has elapsed since the flight, and the flight was longer than eight hours, and The index case is sputum smear positive, and either The index case has multi-drug resistant (MDR) TB, or The index case coughed frequently during the flight. The professional in health protection should provide the airline with inform and advise information, to send to passengers seated in the same part of the aircraft as the index case.
You review Mrs Peacock once she has completed the 6 months of treatment for TB. On examination you notice the neck lymph node, though smaller is still present. What is your next course of action? a) Discharge her from clinic b) Continue Isoniazid and Rifampicin for a further 2 months c) Suspect MDR TB and switch to Rifampicin, pyrazinamide and ethambutol for 2 months then Rifampicin and ethambutol for 10 months. d) Arrange for a lymph node biopsy
You review Mrs Peacock once she has completed the 6 months of treatment for TB. On examination you notice the neck lymph node, though smaller is still present. What is your next course of action? a) Discharge her from clinic b) Continue Isoniazid and Rifampicin for a further 2 months c) Suspect MDR TB and switch to Rifampicin, pyrazinamide and ethambutol for 2 months then Rifampicin and ethambutol for 10 months. d) Arrange for a lymph node biopsy
For people with active TB of the lymph nodes, do not routinely extend treatment beyond 6 months for newly enlarged lymph nodes or sinus formation, or for residual enlargement of the lymph nodes or sinuses.
Mr Johns is a 42 year old man who has emigrated to the UK from Indonesia to work as a nurse in the NHS. As part of his screening he undergoes a Mantoux test. He has had a previous BCG vaccination. The Mantoux test is 16 mm. He has no symptoms of a cough, fever or weight loss. This is his chest X-ray. What would you offer him next?
Mr Johns is a 42 year old man who has emigrated to the UK from Indonesia to work as a nurse in the NHS. As part of his screening he undergoes a Mantoux test. He has had a previous BCG vaccination. The Mantoux test is 16 mm. He has no symptoms of a cough, fever or weight loss. This is his chest X-ray. What would you offer him next? a) An interferon-gamma release assay b) Six months of isoniazid with pyridoxine c) Discharge him from clinic d) Isoniazid (with pyridoxine), rifampicin, pyrazinamide and ethambutol for 2 months then isoniazid (with pyridoxine) and rifampicin for a further 4 months
Mr Johns is a 42 year old man who has emigrated to the UK from Indonesia to work as a nurse in the NHS. As part of his screening he undergoes a Mantoux test. He has had a previous BCG vaccination. The Mantoux test is 16 mm. He has no symptoms of a cough, fever or weight loss. This is his chest X-ray. What would you offer him next? a) An interferon-gamma release assay b) Six months of isoniazid with pyridoxine c) Discharge him from clinic d) Isoniazid (with pyridoxine), rifampicin, pyrazinamide and ethambutol for 2 months then isoniazid (with pyridoxine) and rifampicin for a further 4 months
Offer a Mantoux test to new NHS employees who are from a high-incidence country. WHO states countries with more than 40 cases per 100 000 population per year of TB are considered high risk. Indonesia has a prevalence of 316 cases per 100 000 in 2018. If the Mantoux test is positive (5 mm or larger, regardless of BCG history), assess for active TB; if this assessment is negative, offer them treatment for latent TB infection. If Mantoux testing is unavailable, offer an interferon-gamma release assay.
Patients who are <65 years and agree to have treatment for latent TB infection should start on either one of the following regimens: a) Three months of rifampicin and isoniazid (with pyridoxine) b) Six months of isoniazid (with pyridoxine) Before starting treatment offer patients testing for HIV and hepatitis B and C.
Offer a Mantoux test to new NHS employees who will be in contact with patients or clinical materials, if the employees: are not new entrants from high-incidence countries and have not had BCG vaccination (for example, they are without a BCG scar, other documentation or a reliable history). If the Mantoux test is positive, offer an interferon-gamma release assay. If this is positive, assess for active TB; if this assessment is negative, offer them treatment for latent TB infection.
Mr Johns is unsure if he wishes to proceed with latent TB treatment. Which of the following is NOT a risk factor for going on to develop active TB: a) younger than 5 years b) jejunoileal bypass c) diabetes d) gastrectomy e) silicosis f) hepatitis C
Mr Johns is unsure if he wishes to proceed with latent TB treatment. Which of the following is NOT a risk factor for going on to develop active TB: a) younger than 5 years b) jejunoileal bypass c) diabetes d) gastrectomy e) silicosis f) hepatitis C
Be aware that certain groups of people with latent TB are at increased risk of going on to develop active TB, including people who: are HIV-positive are younger than 5 years have excessive alcohol intake are injecting drug users have had solid organ transplantation have a haematological malignancy are having chemotherapy have had a jejunoileal bypass have diabetes have chronic kidney disease or receive haemodialysis have had a gastrectomy are having treatment with anti-tumour necrosis factor-alpha or other biologic agents have silicosis.
People in the groups listed who do not have treatment for latent TB, should be advised of the risks and symptoms of TB (on the basis of an individual risk assessment), usually in a standard letter of the type referred to as 'Inform and advise' information.
References https://radiopaedia.org/cases/normal-chest-x-ray https://www.nice.org.uk/guidance/ng33/chapter/recommendations# latent-tb https://worldhealthorg.shinyapps.io/tb_profiles/?_inputs_&lan=%22 EN%22&iso2=%22ID%22&main_tabs=%22est_tab%22 https://radiopaedia.org/articles/tuberculosis-pulmonary- manifestations-1?lan https://www.radiologymasterclass.co.uk/gallery/chest/pulmonary- disease/tuberculosis_tb#top_1st_img https://pubs.rsna.org/doi/full/10.1148/rg.2017160032