DERMATOLOGY AND RHEUMATOLOGY
Staphylococcal Scalded Skin Syndrome (SSSS) is a serious condition characterized by red blistering skin resembling burns. It is caused by toxins from Staphylococcus aureus, leading to exfoliation of the skin. Common in infants, the elderly, and immunocompromised individuals, SSSS requires prompt diagnosis through history, examination, and investigations like skin biopsies. Treatment involves a supportive approach and antibiotics, while complications can include severe dehydration, pneumonia, sepsis, and shock.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
DERMATOLOGY AND RHEUMATOLOGY BY DR OLALEKAN ADISA
DERMATOLOGY AND RHEUMATOLOGY STAPHYLOCOCCAL SCALDED SKIN SYNDROME ERYTHEMA MULTIFORME STEVEN JOHNSON SYNDROME TOXIC EPIDERMAL NECROLYSIS SYSTEMIC LUPUS ERYTHEMATOSUS
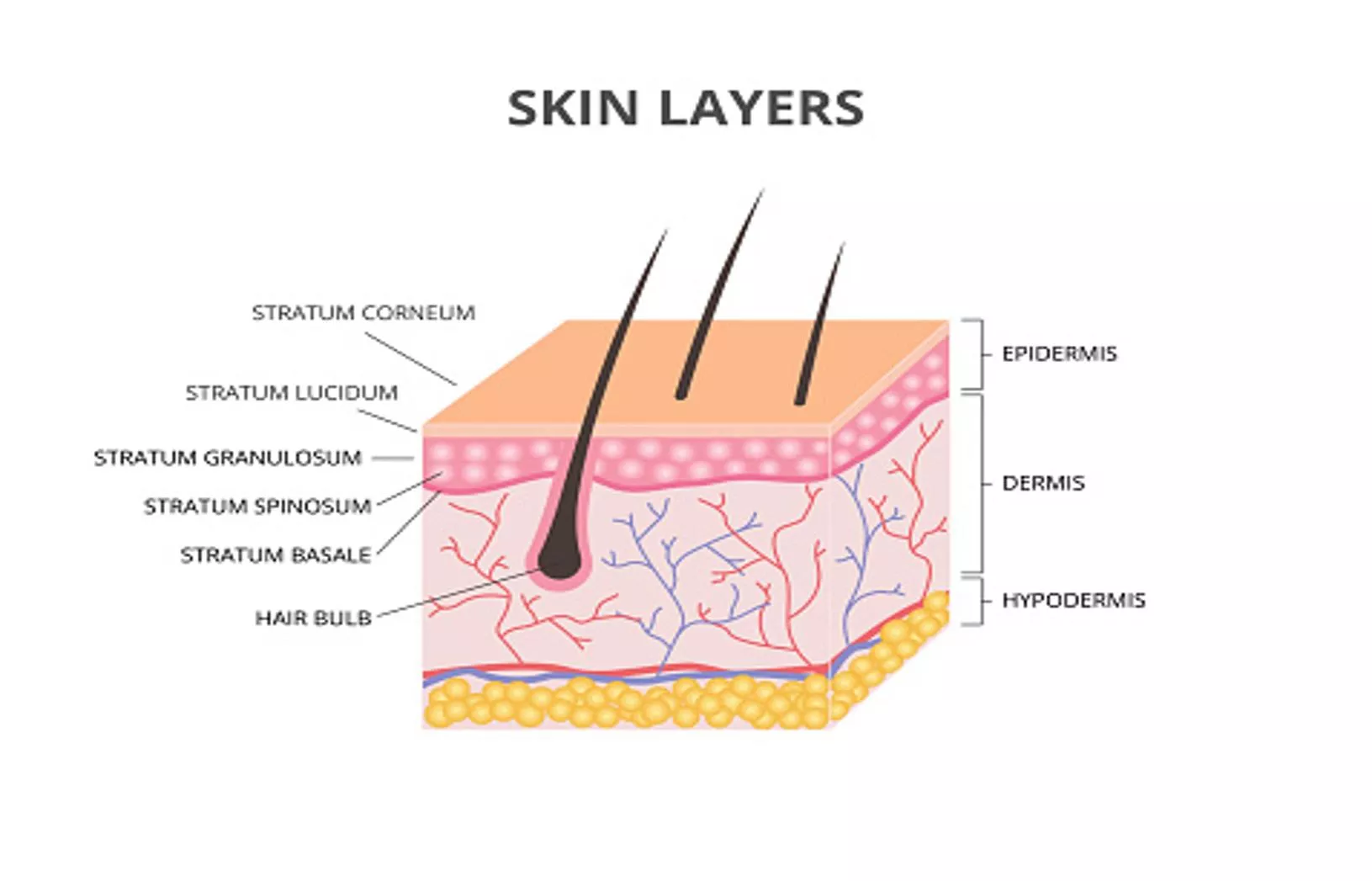
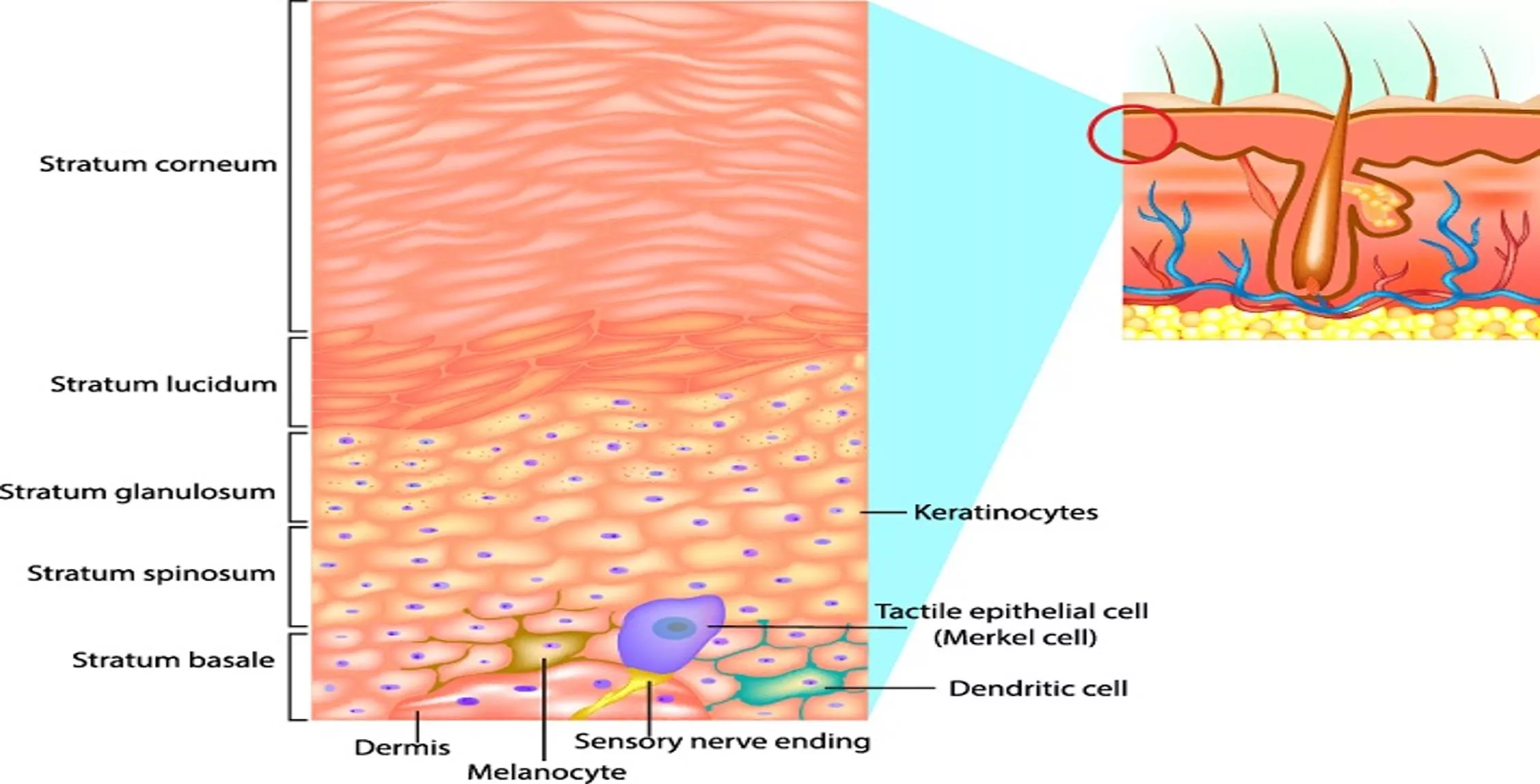
STAPHYLOCCOCAL SCALDED SKIN SYNDROME Staphylococcal scalded skin syndrome(SSSS): is an illness characterised by red blistering skin that looks like burns or scald. SSSS is caused by exfoliative epidermolysis exotoxin of Staphyloccus aureus. Desmosomes are attacked and destroyed by toxins Blister formation and rupture in24-48hours
STAPHYLOCCOCAL SCALDED SKIN SYNDROME Formation of burn-like skin area Start around the flexure area of the body Common in infant and <5years Neonates, Immunocompromised individuals, individual with renal failure and Elderly are at risk
RISK FACTORS 1) Low immunity Infants Elderly Immunocompromised individuals 2) Individual with renal failure
DIAGNOSIS HISTORY: Rash, irritable,fever etc EXAMINATION: Peeling skin, Nicolsky sign +ve INVESTIGATIONS: FBC, Serum chemistry, skin,urine & blood culture, skin biopsy
TREATMENT ABC APPROACH SUPPORTIVE ANTIBIOTICS
COMPLICATIONS SEVERE DEHYDRATION PNEUMONIA SEPSIS SEVERE INFECTION: SHOCK
ERYTHEMA MULTIFORME DIFINITION TYPES EPIDEMIOLOGY CAUSES CLINICAL FEATURES TREATMENTS COMPLICATIONS
ERYTHEMA MULTIFORME Erythema multiforme is an immune-mediated mucocutaneous condition characterised by target lesions. It is a skin reaction that can be triggered by an infection or some medicines.
TYPES 2 Types: Minor and Major Minor: It's usually mild and goes away in a few weeks. Major: a rare, severe form that can affect the mouth, genitals and eyes and can be life- threatening.
EPIDERMIOLOGY Erythema multiforme mainly affects children and young adults(adults under 40) Although it can happen at any age. Slightly affects more males than females In UK: Incidence is unknown, but account for 1% of clinician visit of dermatological problems Globally: 1.2-6 cases per million individuals per year
CAUSES Idiopathic Infections Drugs
CAUSES Some medicines can occasionally cause the more severe form of erythema multiforme. Possible medicine triggers include: Antibiotics such as sulfonamides, tetracyclines, amoxicillin and ampicillin NSAIDs such as Ibuprofen Anticonvulsants such as phenytoin and barbiturates
CAUSES Infections: Viral, bacterial Most cases are caused by a viral infection often the herpes simplex (cold sore) virus. This virus usually lies inactive in the body, but it can become reactivated from time to time. Some people will get a cold sore a few days before the rash starts. Erythema multiforme can also be triggered by mycoplasma bacteria, a type of bacteria that sometimes cause chest infections.
CLINICAL FEATURES The rash starts suddenly and develops over a few days. It tends to start on the hands or feet Later spreading to the limbs, upper body and face. It is usually self limiting and resolves within 2-4weeks in most cases.
CLINICAL FEATURES The rash: Starts as small red spots, which may become raised patches a few centimetres in size Often has patches that look like a target or "bulls-eye", with a dark red centre that may have a blister or crust, surrounded by a pale pink ring and a darker outermost ring May be slightly itchy or uncomfortable Usually fades over 2 to 4 weeks In more severe cases, the patches may join together to form large, red areas that may be raw and painful.
CLINICAL FEATURES Additional symptoms of erythema multiforme can include: A high temperature A headache Feeling generally unwell Raw sores inside your mouth, making it hard to eat and drink
OTHER CLINICAL FAETURES Swollen lips covered in crusts Sores on the genitals, making it painful to pee Sore, red eyes Sensitivity to light and blurred vision Aching joints
DIAGNOSIS HISTORY EXAMINATION INVESTIGATION
TREATMENTS Treatment aims: To tackle the underlying cause of the condition Relieve your symptoms And stop your skin becoming infected.
TREATMENTS Stopping any medicine that may be triggering your symptoms Antihistamine and moisturising cream, emollients, to reduce itching Steriod cream to reduce redness and swelling (inflammation) Painkillers for any pain Antiviral tablets, if the cause is a viral infection Anaesthetic mouthwash to ease the discomfort of any mouth sores
TREATMENTS Severe cases: Stronger painkillers Wound dressings to stop the sores becoming infected A softened or liquid diet if mouth is badly affected some people may need fluids given through a drip into a vein Steriod tablets to control the inflammation Antibiotics if there is a bacterial infection Eye drops or ointment if eyes are affected
COMPLICATIONS Most people with erythema multiforme make a full recovery within a few weeks. There are usually no further problem and the skin heals without scarring. There is a risk the condition could come back at some point, especially if it was caused by the herpes simplex virus. You may be given antiviral medicine to prevent attacks if you experience them frequently.
COMPLICATIONS In severe cases, possible complications can include: A skin infection (cellulitis) Sepsis Permanent skin damage and scarring Permanent eye damage Inflammation of internal organs, such as the lungs
STEVENS-JOHNSON SYNDROME DEFINITION TYPES/VARIANTS EPIDEMIOLOGY CLINICAL FEATURES CAUSES TREATMENT COMPLICATIONS
STEVENS-JOHNSON SYNDROME Stevens-johnson syndrome (SJS) is a serious disorder of the skin and mucous membrane. It is usually a reaction to medication. It starts with aflu-like symtoms And followed by a painful rash Rash spreads and blisters Then the top layer of the affected skin dies, sheds and begins to heal after several days.
STEVENS JOHNSON SYNDROME (SJS) TOXIC EPIDERMAL NECROLYSIS(TEN) SJS/TEN OVERLAP
EPIDERMIOLOGY SJS/TEN: Rare 0.4-1.3 per million individual Female >Male Children and young adults/older adults
CAUSES SJS is a rare and unpreditable illness and cause may or may not be be identified. Medication(up to 2 weeks) Infection Both
CAUSES Medications: Allopurinol(especially >100mg/day) Anticonvulsants & antipsychotics Antibacterial/sulfonamides Nevirapine(viramune, viramune XR) Pain relievers(acetamenophen, NSAIDS)
CAUSES Medications: Anticonvulsants: Lamotrgine, carbamazipine, phenytoin, phenobarbitone Sulfonamides: cotrimoxazole, sulfasalazine
CAUSES INFECTIONS: BACTERIAL INFECTION: Pneumonia caused by mycoplasma pneumoniae VIRAL INFECTION: Herpes simplex
RISK FACTORS HIV infection: 100 times >general population A weakned immune system: organ transplant, HIV/AIDS & autoimmune diseases Cancer: particularly blood cancer are at increased risk of SJS Past hx of SJS A family Hx of SJS in immediate blood relative Genetic factors: certain genetic variation called HLA-B*1502 in Asian & south Asian ancestry, especially if also taking drugs for seizure, gout or mental illness.
CLINICAL FEATURES Early(1-3 days): Fever A sore mouth and throat Fatigue Burning eyes
CLINICAL FAETURES Later(as the condition develops): Unexplained widespread skin pain A red or purple rash that spreads Blisters on the skin and mucous membranes of the mouth, nose, eyes and genitals Shedding of the skin withins days after blisters form
DIAGNOSIS History Physical examination Investigations: to confirm and or rule out other causes(Blood tests, imaging-CXR-pneumonia, culture- to rule infection, and skin biopsy-to confirm and rule out other possible causes
TREATMENT SJS is an emergency and might requires ICU/burn unit. Stop all medications especially the non essential drugs Supportive care(ABC)
TREATMENT Supportive care: Fluid replacement and nutrition(NG tube feeding) Wound care: cool, wet compression, blister/dead tissue removal, petrolleum jelly, and wound dresssing MDT- urologist(stricture) Eye care: may need ophthalmologist