COVID-19 Vaccination Programme for Childbearing Women - Educational Slides and Key Messages
This presentation focuses on the COVID-19 vaccination programme for childbearing women, providing information on learning objectives, key messages, and current vaccination programmes for pregnant and breastfeeding women. It discusses the understanding of COVID-19 symptoms, the importance of vaccination during pregnancy and breastfeeding, and guidelines for women planning pregnancy. Key messages emphasize the safety and benefits of vaccination, highlighting recommendations from the Joint Committee on Vaccination and Immunisation. The content aims to educate healthcare professionals and support informed decision-making for women in various stages of pregnancy and motherhood.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
COVID-19 Vaccination programme for childbearing women Acknowledgments to PHW and PHE for use of their training slides These slide are provisional Subject to revision Provisional Subject to revision Use latest version link: x
Content 1. Learning objectives, key messages and introduction 2. COVID-19 symptoms and complications 3. COVID-19 in pregnant women and neonates 4. COVID-19 vaccination programme for pregnant women, breastfeeding women and women planning a pregnancy 5. Additional information and resources
Learning objectives By the end of this session, you should be able to: explain what COVID-19 is and be aware of common symptoms / symptom progression identify pregnant women who are at high risk of COVID-19 infection understand the COVID-19 vaccination programme for pregnant women, breastfeeding women and women planning a pregnancy
Key messages There is no known risk associated with giving inactivated, recombinant viral or bacterial vaccines or toxoids during pregnancy or whilst breastfeeding The Joint Committee on Vaccination and Immunisation (JCVI) have advised that women who are pregnant should be offered vaccination at the same time as non-pregnant women, based on their age and clinical risk group Women who are planning pregnancy or are in the immediate postpartum period can be vaccinated with a suitable COVID-19 vaccine for their age and clinical risk group
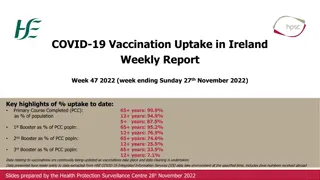
Current vaccination programmes for pregnant women Pregnant women and women who are breastfeeding are already routinely and safely offered vaccines. These vaccines, like the COVID-19 vaccines, are non- live vaccines: influenza vaccine recommended for all pregnant women at any gestation (during flu season) pertussis (whooping cough) vaccination for pregnant women in each pregnancy from 16 weeks gestation
COVID-19 - SARS-CoV-2 The disease COVID-19 is the disease that is caused by infection with the SARS-CoV-2 virus which belongs to the Coronavirus family - SARS-CoV-2 stands for Severe Acute Respiratory Syndrome (SARS) and CoV for coronavirus - COVID-19 stands for Coronavirus Disease and 19 is from the year 2019 when it was first seen SARS-CoV-2 virus is the most recently discovered coronavirus and has now affected many countries globally because of the global spread and the substantial number of people affected, the World Health Organisation (WHO) declared COVID-19 as a pandemic on 11/03/2020 (Pan (all) demos (people))
COVID-19 Symptoms The estimated incubation period is 3 to 6 days but can vary between 1 and 11 days. Symptoms may vary by age but the main symptoms of coronavirus are: a new, continuous cough coughing for more than an hour, or 3 or more coughing episodes in 24 hours a high temperature a loss or change to sense of smell or taste Other symptoms reported include: fatigue and lethargy shortness of breath headache sore throat aching muscles diarrhoea and vomiting rhinorrhea (runny nose) myalgia (aching muscles)
COVID-19 symptom progression Symptoms may begin gradually and are usually mild. the majority of people (around 80%) have asymptomatic to moderate disease and recover without needing hospital treatment around 15% may get severe disease including pneumonia older people and those with underlying medical problems such as high blood pressure, heart and lung problems, diabetes, or cancer are more likely to develop serious illness around 5% become critically unwell. This may include septic shock and/or multi- organ and respiratory failure
Complications of COVID-19 disease Complications from COVID-19 can be severe and fatal. The risk of developing complications increases with age and is greater in those with underlying health conditions. Complications that can develop include: venous thromboembolism heart, liver and kidney problems neurological problems coagulation (blood clotting) failure respiratory failure multiple organ failure septic shock
COVID-19 in pregnant women The risk to pregnant women and neonates following COVID-19 infection is generally low, with more than half of pregnant women who test positive for SARS-CoV-2 being asymptomatic A small proportion of pregnant women can have severe or fatal COVID-19 Risks are higher > 28 weeks gestation Studies in the UK have revealed women with COVID-19 during pregnancy were > 50% more likely to experience pregnancy complications (including premature birth, pre-eclampsia, admission to intensive care and death) compared to pregnant women unaffected by COVID-19 (www.ox.ac.uk/news/2021-04-23-research- uncovers-high-risk-pregnant-women-covid-19) The largest global systematic review indicates that pregnant women are more likely to be admitted to the intensive care unit (ICU) with COVID-19 than age matched non-pregnant women (https://doi.org/10.1101/2021.01.06.21249325)
Risk of severe COVID-19 in pregnant women Pregnant women are more likely to have severe COVID-19 infection if they: are overweight or obese are of black and Asian minority ethnic background have co-morbidities such as diabetes (including gestational), hypertension and asthma are 35 years old or older
COVID-19 in neonates It is still unclear whether SARS-CoV-2 can be transmitted vertically, and only about 2% of neonates born to COVID-19 positive mothers in the UK have tested positive for SARS-CoV-2 in the first 12 hours of life However, the risk of preterm birth is increased two to threefold for women with symptomatic COVID-19, and neonates born to mothers with COVID-19 have an increased risk of admission to a neonatal unit Although stillbirths have been reported, perinatal deaths are rare and occurs in < 1% of neonates Studies are now suggesting the development of passive immunity in the neonate following maternal COVID-19 infection, with documentation of the presence of SARS-CoV-2 antibodies in cord blood and breast milk (https://pubmed.ncbi.nlm.nih.gov/33512440)
COVID-19 Vaccination in Pregnancy There is no known risk associated with giving inactivated, recombinant viral or bacterial vaccines or toxoids during pregnancy or whilst breastfeeding Since inactivated vaccines cannot replicate, they cannot cause infection in either the mother or the fetus Although clinical trials on the use of COVID-19 vaccines during pregnancy are not advanced, there is emerging data on the safety of COVID-19 vaccines in pregnancy and the available data do not indicate any harm to pregnancy JCVI has therefore advised that women who are pregnant should be offered vaccination at the same time as non-pregnant women, based on their age and clinical risk group Clinicians should discuss the risks and benefits of vaccination with the woman, who should be told about the limited evidence of safety data for the vaccine in pregnancy
COVID-19 Vaccination in Pregnancy (2) There is now extensive post-marketing experience of the use of the Pfizer BioNTech and Moderna vaccines in the USA, with > 120,000 doses of these vaccines given to pregnant women with no safety signals to date (https://www.cdc.gov/coronavirus/2019- ncov/vaccines/safety/vsafepregnancyregistry.html) There is a limited experience with the use of COVID-19 Vaccine AstraZeneca in pregnant women, and as with most pharmaceutical products, large clinical trials of COVID-19 vaccine in pregnancy have not been carried out Although AstraZeneca COVID-19 vaccine contains a live adenovirus vector, this virus is non replicating so will not cause infection in the mother or the fetus. Adenovirus vectors, similar to those used in the AstraZeneca COVID-19 vaccine, have been widely used to vaccinate women against Ebola without raising any concern Pfizer and Moderna vaccines are the preferred vaccines for pregnant women of any age, because of more extensive experience of their use in pregnancy Pregnant women who commenced vaccination with AstraZeneca, however, are advised to complete with the same vaccine
Pregnant women should be encouraged to read the Royal College of Obstetricians and Gynaecologists (RCOG) information decision aid tool at www.rcog.org.uk/covid-vaccine prior to discussing the risks and benefits of COVID-19 vaccination with their clinician, including the latest evidence on safety
Interval between COVID-19 vaccines and other vaccines given in pregnancy Although no data for co-administration of COVID-19 vaccine with other vaccines exists, in the absence of such data first principles would suggest that interference between inactivated vaccines with different antigenic content is likely to be limited There is no evidence of any safety concerns, although it may make the attribution of any adverse events more difficult Because of the absence of data on co-administration with COVID-19 vaccines, the current advice is COVID-19 vaccine should not be routinely offered at the same time as other vaccines Studies are ongoing to support co-administration of COVID-19 vaccines with influenza during the 2021 / 22 season. Where co-administration does occur, individuals should be informed about the likely timing of potential adverse events relating to each vaccine
Breastfeeding and COVID-19 vaccination There is no known risk associated with giving non-live vaccines whilst breastfeeding JCVI advises that breastfeeding women may be offered vaccination with any of the COVID-19 vaccines The developmental and health benefits of breastfeeding should be considered along with the woman s clinical need for immunisation against COVID-19 The woman should be informed about the absence of safety data for the vaccine in breastfeeding women
COVID-19 vaccination in women who are planning pregnancy JCVI advise that women who are trying to become pregnant do not need to avoid pregnancy after vaccination Women who are planning pregnancy or in the immediate postpartum period can be vaccinated with a suitable product for their age and clinical risk group If a woman finds out she is pregnant after she has started a course of vaccine, she may complete vaccination during pregnancy using the same vaccine product (unless contraindicated). Alternatively, vaccination should be offered as soon as possible after pregnancy Termination of pregnancy following inadvertent immunisation when a woman did not know she was pregnant should not be recommended Surveillance of the inadvertent administration of COVID-19 vaccines in early pregnancy is being conducted by PHE, report at www.gov.uk/guidance/vaccination-in-pregnancy-vip
Additional information and resources
COVID-19 vaccines and fertility There is no evidence to suggest that COVID-19 vaccines will affect fertility or fertility treatment The RCOG advise there is no plausible mechanism by which current vaccines could cause any impact on women s fertility
Menstrual disorders and unexpected vaginal bleeding The MHRA is closely monitoring reports of menstrual disorders and unexpected vaginal bleeding following vaccination against COVID-19 in the UK These reports have also been reviewed by the independent experts of the Commission on Human Medicines COVID-19 Vaccines Benefit Risk Expert Working Group and members of the Medicines for Women s Health Expert Advisory Group The current evidence does not suggest an increased risk of either menstrual disorders or unexpected vaginal bleeding following the vaccines The number of reports of menstrual disorders and vaginal bleeding is low in relation to both the number of females who have received COVID-19 vaccines to date and how common menstrual disorders are generally Although the MHRA will continue to closely monitor reports of menstrual disorders and vaginal bleeding with COVID-19 vaccines, they advise that women with concerns about menstrual bleeding or irregularities should seek the advice of a healthcare professional
Adverse reactions following vaccination Vaccines can cause side effects. This is because vaccines work by triggering an immune system response. Most side effects are mild and only last a few days Very common side effects include: having a painful, heavy feeling and tenderness in the arm where you had the injection; feeling tired; a headache; general aches, chills, or flu like symptoms Mild fever can last for two to three days after the vaccination but a high temperature is unusual An uncommon side effect is swollen glands in the armpit or neck on the same side as the arm where you had the vaccine. This can last for around 10 days, but if it lasts longer seek medical advice
Contraindications and precautions There are very few individuals who cannot receive the Pfizer BioNTech, Moderna or AstraZeneca COVID-19 vaccines. Where there is doubt, rather than withholding vaccination, appropriate advice should be sought from the relevant specialist, or from the local immunisation or health protection team (Duty Room 0300 555 0119) The vaccine should not be given to those who have had a previous systemic allergic reaction (including immediate-onset anaphylaxis) to: A previous dose of the same COVID-19 vaccine Any component (excipient) of the COVID-19 vaccine e.g. polyethylene glycol (PEG) Minor illnesses without fever or systemic upset are not valid reasons to postpone immunisation If an individual is acutely unwell, immunisation may be postponed until they have fully recovered. This is to avoid confusing the differential diagnosis of any acute illness (including COVID-19) by wrongly attributing any signs or symptoms to the adverse effects of the vaccine Although pregnancy increases the risk of clotting conditions, there is no evidence that pregnant women, those in the postpartum or women on the contraceptive pill are at higher risk of the specific condition of thrombosis in combination with thrombocytopaenia after the AstraZeneca vaccine. There have been no confirmed cases reported in pregnant women to date Individuals who have received the first dose of AstraZeneca vaccine without developing this rare condition are advised to receive the second dose of the same vaccine at the currently recommended interval
Useful resources Green Book COVID-19 chapter 14a https://www.gov.uk/government/publications/covid-19-the- green-book-chapter-14a RCOG COVID-19 information for pregnancy and women s health https://www.rcog.org.uk/en/guidelines-research-services/coronavirus-covid-19-pregnancy-and- womens-health/ PHA COVID-19 Vaccination training resources https://www.publichealth.hscni.net/covid-19- coronavirus/northern-ireland-covid-19-vaccination-programme https://www.gov.uk/guidance/vaccination-in-pregnancy-vip PHE tracks women who have been immunised with COVID -19 vaccine who did not know they were pregnant at the time of vaccination. Please complete the notification and reporting form for all cases Coronavirus Yellow Card reporting scheme coronavirusyellowcard.mhra.gov.uk/ or call 0800 731 6789 https://www.gov.uk/government/news/jcvi-issues-new-advice-on-covid-19-vaccination-for-pregnant- women