Comprehensive Overview of HIV Testing Services for Health Professionals
This session covers essential topics on HIV Testing Services (HTS) for health professionals, including the definition of HTS, guiding principles, service delivery platforms, testing process, test results, equipment required, linkage to care, and more. Participants will gain insight into the benefits of knowing one's HIV status, a rights-based approach to HTS, and the foundation of effective HTS known as the 5 Cs: Consent, Counselling, Confidentiality, Correct Connection, and Continuity of Care.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Basic HIV Course for Health Professionals Session 3a: HIV Testing Services (HTS)
Learning Objectives By the end of this session participants should be able to: Explain what HIV testing services (HTS) are Define the different modalities under HTS Describe the guiding principles of HTS Describe the different HTS service delivery platforms Describe the HIV testing process Outline different HIV tests results Describe equipment required to conduct an HIV rapid test Explain importance of linkage to care following a HIV positive diagnosis and the services that patients should expect to receive
Group Discussion What are the benefits of knowing one s HIV- status?
Definition: HIV Testing Services (HTS) HIV testing services (HTS) embrace full range of services provided with HIV testing: Counselling (pre test information, post-test counselling) Linkage to HIV prevention, treatment and care services and other clinical and support services Coordination with lab services to support quality assurance and the delivery of correct results
A Rights-Based Approach Human rights-based approach that prioritises: universal health coverage gender equality and health-related rights such as accessibility availability acceptability and quality of services essential for success of HTS programme This Photo by Unknown Author is licensed under CC BY-SA
The 5 Cs: The Foundation of Effective HTS Consent People who receive testing must: Counselled and consent to be tested be informed of HTS process and of right to decline testing Discussions between HTS provider and client should not be disclosed to anyone without consent of person being tested Encourage shared confidentiality with partner or family members Pre-test information can be done in group setting, but provide individuals with a private setting for individuals with questions they do not wish to share with others Follow HIV testing with high-quality post-test counselling Quality assurance (QA) mechanisms are essential to ensure people receive a correct diagnosis Linkage to prevention, treatment and care services and effective and appropriate follow-up should be provided Confidentiality Counselling Correct Connection
CICT - Client Initiated Counselling and Testing For client-initiated counselling and testing, (CICT), individual voluntary requests (previously VCT)an HIV test and counselling at health facility and other areas where HTS services are offered. Those receiving CICT provide signed consent, which should always be documented by provider in patient s file
PICT - Provider Initiated Counselling and Testing Also known as Routine offer of Voluntary Counselling and testing In this model, provision of HIV counselling and testing is offered and recommended by health care providers to all patients attending health facilities - standard component of medical care All patients that receive PICT should provide, at a minimum, written consent for HIV testing
HIVSS- Self-Screening Person voluntarily collects own specimen and performs an HIV screening and interprets the result Not recommended for users with known HIV status who are taking ARV drugs - may lead to an incorrect self-test result (false non-reactive)
Index testing Index testing: voluntary process where counsellors and/or health care workers ask index clients to list all of their: (1) sexual or injecting drug partners within the past year, and (2) biologic children. Index client: an individual newly diagnosed as HIV-positive and/or an HIV-positive individual who is enrolled in HIV treatment services
Index testing process If the index client agrees, each listed partner and child is: (1) contacted, (2) informed that they need an HIV test, and (3) offered voluntary HIV testing services (HTS). Goal of index testing is to break the chain of HIV transmission by offering HTS to persons who have been exposed to HIV and linking them to: HIV treatment, if positive, or Prevention services (e.g. VMMC, PrEP, condoms), if negative.
HIV Testing Algorithm HTS using rapid antibody test (adolescents/adults including pregnant/ breastfeeding women)
HIV Testing Algorithm HTS using rapid antibody test: adolescents/adults Group information to all clients Individual sessions offer to Agree to test (person signs the consent form Refuse HIV reactive Confirm by 2nd rapid test Post-refusal Counselling HIV non-reactive 2nd test reactive Continuous offer PITC with each visit 2nd test non-reactive -Post test counselling -Re-test after 6 weeks, 4 weeks with 4th generation antibody/antigen test - Repeat test in pregnant woman after 3 months Post test counselling Same day: -TB screening -Clinical staging -Baseline bloods -Initiate ART when if the patient is ready Repeat the testing algorithm If still indeterminate, do HIV Elisa
Rapid Testing: Principles of Testing Process must be: Completely voluntary; Conducted with informed consent Confidential Protective of person who tested All forms of HTS should be voluntary, adhere to five Cs Children may self-consent to HIV testing if 12 years of age and above, and child is of sufficient maturity to understand benefits, risks, and implications of HIV test
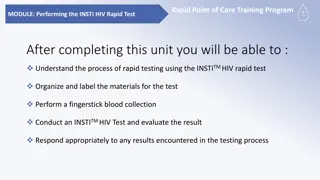
Components of Testing 1. Informed consent 2. Consent formed signed 3. Collecting the necessary equipment 4. Performing the test 5. Interpreting and providing the result This Photo by Unknown Author is licensed under CC BY-NC-SA
Consent No person may undergo testing without full information of what test is about It is vitally important prior to testing that patient has signed for informed consent Consent may either be written or verbal
Pre-test Information Must be age-appropriate through either individual or group information session Followed by individual one-on-one session to assess whether information communicated in group session has been understood and remaining questions answered, with aim to clarify misunderstandings, address concerns
Collecting the Necessary Equipment Checklist of Supplies and Materials Hand washing soap Paper towels Surgical Gloves Alcohol swabs Sterile Lancets Cotton gauze / wool Transfer pipettes HIV Rapid Test Kit(s) Diluent Timer, clock, or watch Sharps container Red bag for soiled materials Clear plastic bag for unsoiled materials Band-Aids or plasters Spray/Wash bottle Pens for labelling Disinfectant Log book or register Standard Operating Procedures Positive and Negative Controls
Steps Involved in Performing the HIV Test (1) Introduction Introduce yourself, explain your role, HTS process Discuss confidentiality Contracting
Steps Involved in Performing the HIV Test (2) Motivation for testing and risk reduction Explore reasons for testing, knowledge of HIV/AIDS and client history Discuss client s sexual risk behaviour and risk reduction options Discuss advantages and disadvantages of testing Explain window period and seroconversion and their impact on results Check client s understanding of the above and invite questions
Steps Involved in Performing the HIV Test (3) Basic HIV/AIDS education Explain and discuss: what HIV and AIDS are, HIV transmission, prevention measures (condom use, PrEP etc.), HIV symptoms and myths
Steps Involved in Performing the HIV Test (4) Anticipation of the reaction to HIV test results Discuss feelings about possible results Discuss imagined consequences of a positive and negative result Discuss and identify possible supportive people Discuss disclosure Provide referral, wellness and support options
Steps Involved in Performing the HIV Test (5) Testing procedure and readiness to test Discuss type of test, what it measures, accuracy, confirmatory tests and how results are given Discuss readiness to test Explain procedure to client Get consent; signed consent is adequate Open test kit in front of client Label test kit using client registration number or name Position hand palm-side up Choose whichever finger is least calloused
Performing the Rapid Test: Testing Procedure Summary Wash hands, put on gloves Position hand palm-side up, assess fingers, choose least calloused Apply intermittent pressure to finger to help blood flow Clean fingertip using alcohol swab, allow area to dry for 30 seconds Hold finger firmly and firmly press lancet to puncture fingertip Wipe away first drop of blood Collect blood using pipette Lower finger to below elbow to encourage blood flow Apply pressure to puncture site using cotton wool to stop bleeding Dispose of needle in sharps container
Clients who Test HIV-Negative Post-test counselling session should focus on: keeping individual negative and active linkage to appropriate prevention services Educate person on window period Educate about PrEP Educate about VMMC is male patient Provide person with condoms and lubricants
Post-Test Services All clients, regardless of the outcome of the HIV test, should be offered and should receive post-test counselling based on their test result All results must be communicated clearly
Post-test Services for People Testing HIV-Negative Those testing HIV-negative should receive health information about test result including: risk reduction counselling recommendations on uptake of preventive behaviours including consistent condom use Post-test counselling session should focus on keeping individual negative Provide active linkage to appropriate services
Services for People with Discrepant Test Results An HIV-inconclusive/indeterminate result means: first reactive test results were not confirmed by subsequent testing using an HIV rapid test Clients with an HIV-inconclusive status should be told a definitive diagnosis cannot be provided that day and Whole blood should be drawn and sent to lab for ELISA testing as a tie breaker; give clients a clear plan for follow-up testing Encourage them to return within seven days for ELISA results to confirm diagnosis
Managing Discrepant HIV Rapid Testing ELISA/EC HIV screening Test HIV NON-REACTIVE HIV REACTIVE ELISA HIV confirmation Test REACTIV E NON- REACTIVE Report as HIV NEGATIVE Report as HIV DISCREPANT and request client to return to facility after six weeks for rapid testing Report as HIV POSITIVE
When to repeat the HIV test WHO WHEN Every full BANC visit Postnatal health care encounter throughout breastfeeding (monthly testing recommended aligned to EPI expanded programme of immunisation) Routinely at labour/delivery At 6-week mother/child visit Couple counselling and testing recommended At Birth Around10 weeks (and 18 weeks for those on 12 week AZT & NVP) At 18 months 6 weeks after complete cessation of breastfeeding Anytime if child has symptoms suggestive of HIV 6 12-monthly depending on risk 6 12-monthly if sexually active or more frequently if they have new sexual partner/s or if having unprotected intercourse After 6 12 weeks for window period Every 3 12 months Pregnant/breastfeedi ng women (to detect HIV sero- conversion) HIV-exposed babies (do not repeat test if infant confirmed to be HIV-infected) All children General population Adolescents If exposed to HIV Key populations (MSM and sex workers)
Recommended Testing Intervals for Infants and Children HIV PCR Test AT BIRTH ALL HIV-exposed neonates These infants can be regarded as high-risk cases that need an urgent diagnosis so should receive HIV PCR as soon as possible after birth Repeat HIV PCR testing at 10 weeks or 18 weeks should be done on all HIV-exposed infants without confirmed HIV infection, regardless of earlier testing Any infant with a positive birth PCR should be urgently referred/ discussed telephonically for ART initiation by a paediatric HIV expert At 10 weeks: All HIV-exposed infants At 18 weeks: All infants who received 12 weeks of NVP prophylaxis
Recommended Testing Intervals for Infants and Children Rapid HIV Antibody (1) AT 18 MONTHS All HIV exposed infants Breastfed infants: (6 weeks post cessation of breastfeeding) All HIV exposed infants- age appropriate: if <18 months old- do HIV PCR >18 months old do rapid HIV Antibody test Family and social history (at all times) Parental request to test the child Father or sibling with HIV infection Death of mother, father or sibling When mother s HIV status is unknown, her whereabouts are unknown, or she is unavailable to be tested
Testing Intervals At 18 weeks if infant received 12 weeks NVP Prophylaxi s At any age if sympto matic or mother test HIV positive 6 weeks post cessation of breastfeeding At 10 weeks At 18 months At birth
Recommended Testing Intervals for Infants and Children Rapid HIV Antibody (2) All children (at all times) with: Clinical features suggestive of HIV infection Acute, severe illness IMCI classification of Suspected symptomatic HIV infection IMCI classification of Possible HIV infection TB diagnosis or history of TB treatment Risk of sexual assault Wet-nursed or breastfed by a woman with unknown or HIV-positive status Children considered for fostering
Linkage to Care (1) Activities that support people testing for HIV and people diagnosed with HIV to engage with prevention, treatment and care services For people with HIV, period begins with HIV diagnosis and ends with enrolment in care or treatment Responsibility of all HTS providers to ensure that clients are connected to appropriate care HIV testing alone is of limited value unless linked with other services
Linkage to Care (2) Services include: Treatment, care, support, disease management Sexual and reproductive health Testing for partners and families includes partner notification and index case testing HIV prevention, including education on condom use and lubricants, and voluntary medical male circumcision (VMMC) other clinical and supportive services
Any Questions? Thank you!