Comparing Bleeding and Mortality Risks of Dabigatran vs. Rivaroxaban in Elderly Medicare Beneficiaries
A study by DJ Graham et al. compared the risks of stroke, bleeding, and mortality in elderly Medicare beneficiaries with nonvalvular atrial fibrillation treated with dabigatran or rivaroxaban. The study included over 118,000 patients and found that dabigatran was associated with a lower risk of major extracranial bleeding, major GI bleeding, and intracranial hemorrhage compared to rivaroxaban. Patients initiating treatment with dabigatran also had a lower risk of major GI bleeding. The study utilized Cox regression and propensity score weighting techniques. The average follow-up duration was less than 4 months.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
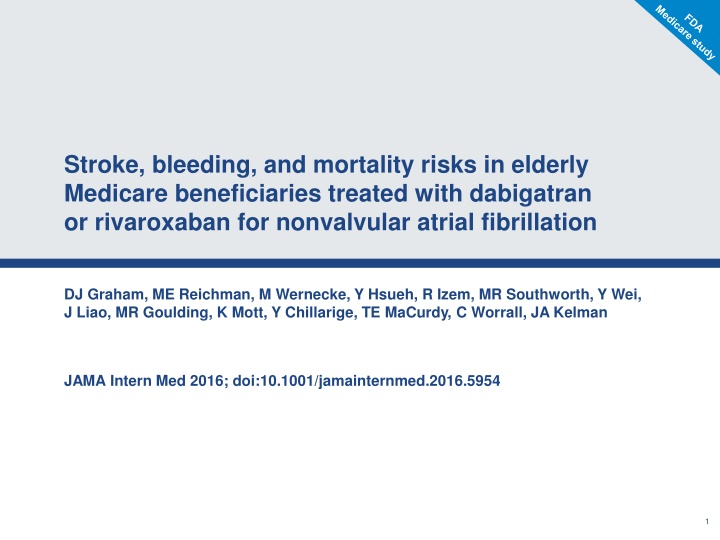
Stroke, bleeding, and mortality risks in elderly Medicare beneficiaries treated with dabigatran or rivaroxaban for nonvalvular atrial fibrillation DJ Graham, ME Reichman, M Wernecke, Y Hsueh, R Izem, MR Southworth, Y Wei, J Liao, MR Goulding, K Mott, Y Chillarige, TE MaCurdy, C Worrall, JA Kelman JAMA Intern Med 2016; doi:10.1001/jamainternmed.2016.5954 1
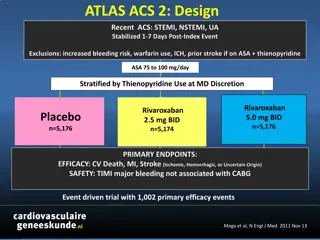
An independent FDA study of >118 000 Medicare patients compared dabigatran 150 mg BID with rivaroxaban 20 mg OD Outcomes Thromboembolic stroke, ICH, major extracranial bleeding events including major GI bleeding, and mortality Methods Retrospective analysis of Medicare database (Nov 2011 Jun 2014) Follow up until outcome of interest, death, end of study, treatment discontinuation (>3 day gap in anticoagulant supply), switching to different OAC Cox regression and inverse probability of treatment weighting based on propensity score Patients New users of dabigatran 150 mg BID, or rivaroxaban 20 mg OD with NVAF, aged 65 years, average follow-up duration <4 months N=118 891 (52 240 dabigatran, 66 651 rivaroxaban) Limitations No major limitations identified ! Funding Interagency agreement between the CMS and FDA CMS, Centers for Medicare and Medicaid Services; ICH, intracranial haemorrhage; Graham et al. JAMA Intern Med 2016 2
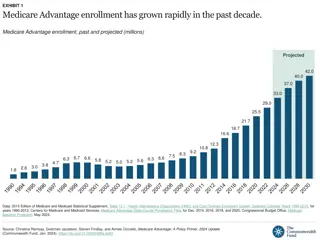
An independent FDA study of >118 000 Medicare patients compared dabigatran 150 mg BID with rivaroxaban 20 mg OD 5 Dabigatran Rivaroxaban HR 1.48 (1.32 1.67) 4 per 100 person-years* HR 1.40 (1.23 1.59) Incidence rate 3 HR 1.15 (1.00 1.32) 2 HR 0.81 (0.65 1.01) 1 HR 1.65 (1.20 2.26) 0 Major extracranial bleeding Major GI bleeding ICH Thromboembolic stroke Death Dabigatran was associated with a statistically significantly lower risk of major extracranial bleeding, major GI bleeding and ICH compared with rivaroxaban *Incidence rates are unadjusted; hazard ratios (HR) are adjusted HR (95% CI) comparing inverse probability of treatment- weighted new-user cohorts; bold values indicate statistical significance; average follow-up duration <4 months; ICH, intracranial haemorrhage; GI, gastrointestinal; Graham et al. JAMA Intern Med 2016 3 3
An independent FDA study of >118 000 Medicare patients compared dabigatran 150 mg BID with rivaroxaban 20 mg OD Kaplan Meier analysis Weighted failure curves 2.0 Death 2.5 Major GI bleeding Rivaroxaban Dabigatran Rivaroxaban Dabigatran 2.0 Cumulative adjusted 1.5 incidence rate, % 1.5 1.0 1.0 0.5 0.5 0 0 0 60 120 180 240 300 0 60 120 180 240 300 Follow-up time, days Follow-up time, days Patients initiating treatment with dabigatran experienced a statistically significantly lower risk of major GI bleeding than those initiating treatment with rivaroxaban Average follow-up duration <4 months; Graham et al. JAMA Intern Med 2016 4
An independent FDA study of >118 000 Medicare patients compared dabigatran 150 mg BID with rivaroxaban 20 mg OD Kaplan Meier analysis Weighted failure curves ICH Thromboembolic stroke 0.6 0.6 Rivaroxaban Dabigatran Rivaroxaban Dabigatran Cumulative adjusted incidence rate, % 0.4 0.4 0.2 0.2 0 0 0 60 120 180 240 300 0 60 120 180 240 300 Follow-up time, days Follow-up time, days The increased rate of ICH with rivaroxaban exceeded its (nonsignficantly) decreased rate of thromboembolic stroke Average follow-up duration <4 months; ICH, intracranial haemorrhage Graham et al. JAMA Intern Med 2016 5
Graham et al. JAMA Intern Med 2016: summary 1 This large, independent FDA analysis of Medicare data reinforces the favourable safety profile of dabigatran compared with rivaroxaban 2 Dabigatran is associated with significant reductions in ICH and major extracranial (including GI) bleeding, compared with rivaroxaban 3 This analysis adds to a growing body of real-world evidence from a range of sources that support the favourable safety profile of dabigatran ICH, intracranial haemorrhage 6
Appendix Baseline patient characteristics 7
Baseline patient characteristics: Graham et al. JAMA Intern Med 2016 Unweighted cohorts Weighted cohorts Characteristic Dabigatran Rivaroxaban Dabigatran Rivaroxaban Age, yrs 65 74, % 50 51 50 50 75 84, % 40 40 40 40 10 9 9 9 85, % Women, % 47 47 47 47 Diabetes, % 34 32 33 33 Heart failure*, % 16 14 15 15 Hypertension, % 86 86 86 86 CHADS2 score 0 1, % 33 34 34 34 2, % 40 40 40 40 3, % 19 18 19 19 4, % 8 8 8 8 HAS-BLED score 1, % 10 10 10 10 2, % 54 54 54 54 3, % 29 29 29 29 4, % 7 7 7 7 Prior hospitalized bleeding event <1 <1 <1 <1 *Hospitalized and outpatient data combined 8
Mortality by age, chronic kidney disease, and CHADS2 Number of events (100 person-years) Dabigatran Rivaroxaban Age, yrs 65 74 145 (0.78) 180 (1.05) 74 84 145 (0.64) 232 (0.81) 55 (0.14) 88 (0.17) 85 Chronic kidney disease Yes 55 (0.13) 77 (0.14) No 291 (1.42) 423 (1.89) CHADS2 score 2 219 (1.15) 276 (1.52) >2 127 (0.41) 224 (0.51) Favours rivaroxaban Favours dabigatran 0.5 1 1.5 2.0 HR Mortality was significantly increased with rivaroxaban compared with dabigatran treatment in patients aged 75 years or with a CHADS2 score >2 Graham et al. JAMA Intern Med 2016 9