Cognitive Behavioral Therapy for Psychosis: Concepts and Applications
Explore the foundational principles of Cognitive Behavioral Therapy (CBT) for psychosis, emphasizing how thoughts influence feelings and behaviors. Gain insights into the cognitive-behavioral model of paranoia and learn about the main tenets of CBTp. Discover how CBTp can effectively address psychotic symptoms by targeting cognitive distortions and maladaptive behaviors, tying symptom reduction to personal goals.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Cognitive Behavioral Therapy for Psychosis: A Workshop for Clinicians Kim T. Mueser Center for Psychiatric Rehabilitation Boston University (With contributions by Cori Cather, Jen Gottlieb, Eric Granholm, and Kate Hardy)
REVIEW: PRIMARY ASSUMPTIONS UNDERLYING CBT What you think in a situation influences how you feel in that situation How you feel influences your behavior, or how you act in that situation or related situations in the future Sometimes how you feel in a situation influences what you think about it Learning how to evaluate and correct inaccurate thoughts/beliefs related to negative feelings can reduce those feelings and lead to more effective behavior
EXAMPLE You are sleeping in your ground floor apartment and you hear scratching on the window. You think someone might be trying to break into your apartment. How would you feel in this situation? What might you do? What if you remembered that you let your cat out before you went to bed, and she didn t come back in, so you think maybe it s your cat at the window? How would you feel? What might you do?
THE COGNITIVE-BEHAVIORAL MODEL Nobody likes me I am a failure Thoughts People want to hurt me Mood Behavior Isolation Depression Avoidance Anxiety Procrastination Fear
CBTp PHILOSOPHY Not so different from CBT for depression and anxiety, really Human experience and behavior exists on a continuum Psychotic symptoms (and other schizophrenia symptoms) are amenable to cognitive and behavioral interventions Reduction of symptoms/distress tied directly to personal goals
THE COGNITIVE-BEHAVIORAL MODEL OF PARANOIA I m in danger People cannot be trusted I m an outsider Social Isolation Avoidance Hypervigilence Safety Behaviors People want to hurt me Thoughts Paranoia Emotions Behavior
MAIN TENETS OF CBTp Symptoms are maintained by appraisal and behavior Distortions are amenable to cognitive and behavioral approaches Psychotic symptoms (e.g., delusions) represent an attempt to make sense of negative affect
WHICH ACT CLIENTS ARE MOST LIKELY TO BENEFIT FROM CBTp? Persons with persistent psychotic symptoms High levels of distress related to symptoms Preferable if person has some degree of doubt or is able to consider alternative explanations, but not absolutely required Can be engaged in talk for 30+ min. Good working relationship with ACT team member(s)
OVERARCHING GOALS OF CBTp Foster a curious attitude about symptoms Decrease distress about symptoms (but not necessarily frequency or intensity of symptoms themselves!) Adopt a living with illness strategy Improve sense of personal control Enhance healthy, effective coping with symptoms Improve day-to-day functioning Prevent severe relapse
STRUCTURE OF CBTp SESSIONS Collaborative agenda setting Review of previous session Review of homework Practice new skill in session Assign homework related to new skill area Session review and feedback
SELECTIVE CBTp SKILLS Engagement and befriending Goal setting Normalization Coping strategy enhancement Cognitive restructuring Cognitive distortions Socratic questioning Behavioral experiments
ENGAGEMENT AND BEFRIENDING Essential to developing therapeutic relationship Ongoing process throughout therapy May require increased amounts of befriending depending on symptoms Paranoia Hallucinations Severe negative symptoms
BEFRIENDING (Contd) Befriending -Focus on neutral non threatening topics -No active formulation or treatment -Non-confrontational -Empathic -Supportive -Accepting -Non-colluding Assertive engagement
COMMON ENGAGEMENT DIFFICULTIES IN CBTp Poor session attendance Lack of enthusiasm for treatment Paranoia or low disclosure at outset Difficulty formulating problems or goals
SOLUTIONS: ASSESS UNDERLYING CAUSES Organizational difficulties: problem-solve solutions Are you working on what is important to the client??? Is low enthusiasm simply negative symptoms? Take it slow, build trust, get to know the person, seek to align with their goals or interests
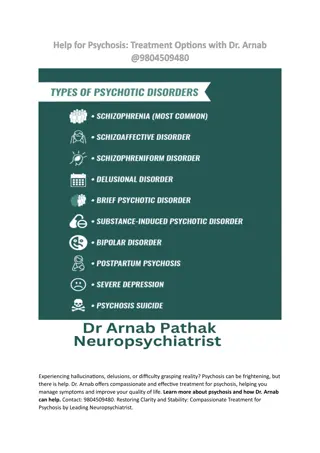
ASSESSMENT DOMAINS Positive Symptoms Delusions Hallucinations Disorganized thoughts Negative Symptoms Reduced emotional expressiveness Poverty of speech Loss of motivation Decreased activity Social withdrawal Quality of Life Work/School/Recreation Interpersonal relationships Physical health/self-care Cognitive Deficits Attention Memory Executive functions Insight Comorbid Conditions Mood Substance abuse Anxiety Medical Illness
AND Suicidality/homicidality Short and longer term life goals Values Understanding of psychosis and associated symptoms Medication adherence
DEVELOPING A PROBLEM/GOAL LIST Collaboration is key Elicit problem areas by discussing what is distressing to the person and what interferes with the goals or desires Assess what is most important to guide goal development Shows the client you are listening and creates a sense that difficulties are contained rather than infinite
DEVELOP A PROBLEM/GOAL LIST (Cont d) Brainstorm and be broad initially, then focus and become more specific Prioritize and maintain a focus throughout work with person Include at least one goal related to a psychotic symptom Other goals may be functional goals related to interference from psychosis or simply life goals
Bryant SAMPLE PROBLEM LIST 1. Neighbors are using wireless technology against me. 2. The voices keep me from getting a job. 3. I don t have anything to do all day. 4. I used to drive and now am worried about doing anything other than walking around the block with my mom. 5. I m confused about these experiences.
Charlotte SAMPLE PROBLEM LIST 1. Neighbors are watching me and informing the police about me. 2. I am being controlled by their instructions. 3. I feel like my family does not care about me. 4. I need to lose weight.
NORMALIZATION CBT is inherently normalizing We all experience negative thoughts We all engage in unhelpful thinking We all use coping strategies that aren t always the most healthy choices Allows for normalizing of psychotic symptoms as well
PSYCHOSIS EXISTS ON A CONTINUUM Stress Drugs Trauma Life experiences Sleep deprivation Psychosis No psychosis
NORMALIZATION OF PSYCHOTIC SYMPTOMS Normalization is the antidote to stigma Avoid catastrophizing Mental Illness is a common experience (1 in 4 people) Psychosis can affect anyone regardless of age, ethnicity, gender, SES Large number of people can overcome symptoms Symptoms may be viewed positively in different cultures Normalizing experiences not dismissing them Check in how the information is received (invalidating?)
NORMALIZING: HOW Encourage people to research and read personal recovery stories Elyn Saks John Nash Eleanor Longden Rufus May Develop library of recovery stories
NORMALIZING: HOW Research prevalence of symptoms (depression, hearing voices, paranoia etc.) 15-20% population experience frequent paranoid thoughts without significant distress 3-5% population have more severe paranoia (Freeman, 2006) 5% of population hear voices (Tien 1991) People hear voices without seeking mental health services (Romme & Escher 1989) 9% people hold delusional beliefs (van Os, 2000) Common to see or hear loved one following bereavement (Grimby 1993) Connect with other people experiencing psychosis Intervoice Psycope.co.uk Paranoia.com
VIDEO DEMONSTRATION OF NORMALIZATION
RATIONALE FOR COPING STRATEGY ENHANCEMENT Focus on distressing symptoms Does not require insight into hallucinations or delusions Use analogies to other distressing experiences (e.g., migraine headaches, bullying) Express empathy that this has been difficult and client has done best he/she can Express optimism that together you can improve coping
ASSESS CURRENT AND PAST COPING RESPONSES Evaluate behavioral, cognitive, affective strategies person has used in the past Categorize as helpful unhelpful and unknown Aggressive engagement and extreme avoidance are usually unhelpful strategies Assign a coping monitoring log Example (next page) of helpful and not helpful coping strategies for hallucinations
Bryant HELPFUL Studying for my exam Watching movies Telling myself that I can handle this Going for a walk with mom Making a list of my good qualities I am a good employee and will be an asset to any organization of which I am a part NOT HELPFUL Yelling back to voices Calling the police Researching wireless technology Trying to convince my dad to believe me Believing what they say Losing hope about my future
Charlotte VOICES: COPING LOG Situation What did How did you respond? Went to bed at 4pm How effective? you hear? Home thinking about watching TV Not at all A little Some A lot She is home.
BEHAVIORAL COPING STRATEGIES Listen to music or other things Change your location Talk with someone, such as trusted other, friend, etc. Listen to a relaxation tape or do a relaxation exercise Take a shower Exercise or go for a walk Do a hobby or other activity
COGNITIVE COPING STRATEGIES Keep a diary to identify triggers, content of the hallucination and associated thoughts Focus in on the experience and use distress tolerance skills Use positive self-talk or prayer Conduct a pro/con analysis (Pay-off Matrix) with command hallucinations and make your own decision about what to do Use acceptance-based strategies that don t actively attempt to suppress hallucinations
ACCEPTANCE AND COMMITMENT THERAPY: THE OTHER ACT Developed by Stephen Hayes, related to CBTp, but not the same Agrees with CBT that thoughts are the cause of much misery, but disagrees that solution is to modify the thoughts Acceptance = understanding of the essential uncontrollability of thoughts Commitment = commitment to one s values and goals, and behavior aligned towards them Suppression of thoughts ineffective Alternative: just notice thoughts, and get on with one s life Example: Thanking one s brain for the hallucination
COGNITIVE COPING STRATEGIES (Cont d) Hallucination scheduling (permit for period of time during day like worry scheduling) Review reattribution ideas that have been helpful
VIDEO DEMONSTRATION OF UNDERSTANDING VOICES
COGNITIVE RESTRUCTURING Teach clients the connection between thoughts and feelings Explain that the thoughts people have are often automatic and are often related to past experiences (e.g., traumatic) and self-perceptions Facilitate the examination of evidence supporting thoughts and beliefs underlying strong negative feelings
COGNITIVE RESTRUCTURING (Contd) Help clients challenge and modify upsetting thoughts and beliefs that are not supported by evidence by: Socratic questioning Exploring alternative beliefs Behavioral experiments Teaching how to recognize distorted thinking styles
CR TARGETS IN CBTp Accuracy of distressing belief Utility of holding onto belief Beliefs about the power and controllability of voices/persecutors Negative core beliefs about self, other s perceptions of self, future Self-stigmatized beliefs related to illness Beliefs about medications and treatment
SOCRATIC QUESTIONING OVERVIEW -Build rapport, engagement -Can be an MI technique -Explore how person understand an event, voice, thought, etc. -Explore possible consequences of staying with particular maladaptive thoughts or behaviors -Help clients to question own inaccurate or distressing assumptions, beliefs and behaviors -Help clients arrive at a new view of the situation that is more in line with evidence
SOCRATIC QUESTIONING STYLE Colombo-like style: freely admit confusion when trying to understand something, ask for client s help in resolving confusion Ask, don t tell Probe questions Gentle, non-judgmental curious style don t interrogate! Foster client s curiosity too
HOW TO: SOCRATIC QUESTIONING Explore meaning client attaches to a specific event, voice, thought What does it say about you that you are being watched by the government? If this were not the case, what would that say about you as a person? Explore possible consequences of staying with particular maladaptive thoughts or behaviors So, what happens if you continue to yell at your voices in public? You spend a lot of time thinking about the idea that you need to develop superpowers to read others minds in order to be happy. I wonder if that gets in the way of you pursuing other meaningful things in life?
HOW TO: SOCRATIC QUESTIONING (Cont d) What do you make of the fact that your brother says he can t hear what you hear? I wonder if it might be important for us to talk more about your belief that you are adopted, since it is causing so much distress? I m curious: what sorts of things got you thinking that your co-workers were poisoning your lunch? You ve mentioned that you are being terrorized by people on the street. What s your sense of why that might be? Help me understand a bit more about how that brain implant device works.
EXPLORING DYSFUNCTIONAL BELIEFS ABOUT VOICES Common Belief Omnipotence Examples My voice is all powerful My voice is in charge of everything I do My voice is all-knowing Whatever they say must be true The voices want to harm me, punish me, or kill me If I don t listen to the voices, they will punish me I cannot ignore my voices Omniscience Malevolence Controllability
EXPLORING BELIEFS ABOUT VOICES: HELPFUL PROBE QUESTIONS Control How much control do you have over the voices? Are there some things the voices told you to do where you drew the line and refused? Power Who is more powerful, you or the voices? Do the voices make empty threats?
EXPLORING BELIEFS ABOUT VOICES: HELPFUL PROBE QUESTIONS (Cont d) Trustworthiness Do the voices ever provide contradictory information? Have they ever lied? Can they always be trusted? Usefulness of Listening/Complying What important information has the voices given you over the years? Do the voices ever give you misinformation or lead you on a wild-goose chase?
EXPLORING BELIEFS ABOUT VOICES: HELPFUL PROBE QUESTIONS (Cont d) Malevolence Have the voices ever been helpful or kind? Is there anything you might miss about the voices if they were gone?
OVERVIEW: EXPLORING ALTERNATIVE BELIEFS Teach cognitive flexibility as a skill Pre-cursor to CR Begin with coaching around generating alternative beliefs for everyday scenarios Then progress to scenarios that are tailored to the individual s delusional or paranoid beliefs
EXPLORING ALTERNATIVE BELIEFS (Contd) Behavioral scaffolding Start with identified alternative responses to situation, move toward coaching of additional responses, then to independence with the exercise items Helpful probe questions: What s another possible explanation for why this may have happened? What factors related to____(the situation/the way the world works/the person involved in the scenario/you) may have caused or contributed to this happening?
BASED ON THE COGNITIVE MODEL Someone calls you on the phone and doesn t leave a message It s the mafia Anxious, scared It was a wrong number Calm It was a telemarketer Slightly Annoyed