Cerebral Edema: Causes, Treatments, and Pathophysiology
Cerebral edema is a life-threatening condition that can result from various factors such as trauma, infarction, hemorrhages, or tumors. This condition can lead to increased morbidity and mortality due to hemorrhage or herniation. New advances in understanding the pathophysiology of cerebral edema have led to clinical trials for more targeted treatments. The Monro-Kellie hypothesis explains the dynamics of intracranial pressure. Cellular changes and the inflammatory cascade contribute to the development of cerebral edema, with distinct stages characterized by morphological and molecular changes.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
WHAT IS CEREBRAL EDEMA? Cerebral edema is a life-threatening condition that develops as a result of an inflammatory cascade. Most frequently, this is the consequence of cerebral trauma, massive cerebral infarction, hemorrhages, abscess, tumor, allergy, sepsis, hypoxia, and other toxic or metabolic factors. Can lead to increased morbidity and mortality via hemorrhage and/or herniation.
CEREBRAL EDEMA OLD MEETS NEW Currently approved treatments for cerebral edema decompressive craniectomy and osmotherapy were developed prior to any knowledge of modern cerebral edema pathophysiology. These therapies attempt to manage downstream end-stage events without directly attenuating the underlying molecular mechanisms of cerebral edema. New advances have shed light on heretofore poorly understood cellular and molecular pathophysiology of cerebral edema, and have led to clinical trials of antagonists of key molecular events in cerebral edema formation. It is now understood that cerebral edema evolves in stages, where each stage is characterized by distinct morphological and molecular changes. Cytotoxic edema, or cellular swelling, manifests minutes after acute central nervous system (CNS) injuries. Ionic edema, an extracellular edema that occurs in the presence of an intact blood brain barrier (BBB), forms immediately following cytotoxic edema. Vasogenic edema, an extracellular edema that includes extravasation of plasma proteins, manifests hours after the initial insult.
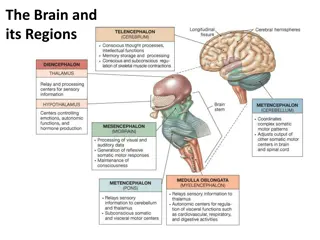
MONRO-KELLIE HYPOTHESIS Alexander Alexander Monro 1844) led to the formation and rise in popularity of the 1844) led to the formation and rise in popularity of the Monro states that during health, the volume occupied by the contents of the cranium must states that during health, the volume occupied by the contents of the cranium must remain in dynamic equilibrium, the implication being that the fluid influx rate must remain in dynamic equilibrium, the implication being that the fluid influx rate must equal the efflux rate. equal the efflux rate. Monro (1733 (1733 1817), George Kellie (1720 1817), George Kellie (1720 1779), and John Abercrombie (1780 1779), and John Abercrombie (1780 Monro- -Kellie axiom, which Kellie axiom, which 80% Brain 80% Brain 1400ml on average 10% CSF 10% CSF 150ml on average 10% Blood 10% Blood 150ml on average As the brain, blood or CSF volumes continue to increase, the accommodative mechanisms fail and intracranial pressure (ICP) then rises exponentially.
PATHOPHYSIOLOGY Cellular level = Complex Cellular level = Complex Damaged cells swell, blood vessels leak, blocked absorption pathways Injury cascade Glutamate release -> Sodium buildup in the cell, creating an osmotic gradient and thus expanding the cell by water volume. Increase in water causes dysfunction but not irreversible damage
PATHOPHYSIOLOGY Cellular level (continued) Cellular level (continued) Sodium pump is non-functioning which also increase the volume of calcium in the cell. This triggers an inflammatory response, releasing cytokines. Microglial cells are activated -> free radical release and proteases that attack cell membrane and capillaries. Once the membranes are damaged, the cell is irreparably damaged.
CEREBRAL EDEMA CLASSIFICATION Cytotoxic Edema: Cytotoxic Edema: Cellular (cytotoxic) cerebral edema refers to cellular swelling. - seen in conditions like head injury and hypoxia. - results from the swelling of brain cells, most likely due to the release of toxic factors from neutrophils and bacteria. - Cytotoxic edema is caused by swelling of glia, neurons, endothelial cells. - BBB remains intact BBB remains intact
CEREBRAL EDEMA CLASSIFICATION Vasogenic Vasogenic Edema: an incompetent blood brain-barrier (BBB). - the most common type of brain edema - results from increased permeability of the capillary endothelial cells. - breakdown in the blood-brain barrier allows movement of proteins from the intravascular space through the capillary wall into the extracellular space. Edema: the influx of fluid and solutes into the brain through VEGF (Vascular Endothelial Growth Factor ) VEGF (Vascular Endothelial Growth Factor ) - most brain tumors oversecrete VEGF, which leads to an abnormally permeable tumor vasculature. This hyperpermeability allows fluid to leak from the intravascular space into the brain parenchyma, which causes vasogenic cerebral edema and increased interstitial fluid pressure.
TREATMENT Vasogenic Vasogenic Edema Edema Oncology Setting Oncology Setting In high-grade gliomas and brain metastases, the BBB is typically disrupted, allowing passage of fluid into the extracellular space. Increased permeability of the BBB is primarily owing to opening of the interendothelial tight junctions, but also due to increased endothelial pinocytosis and endothelial fenestrations and relative destruction of the astrocytes. Dexamethasone - It has been suggested that corticosteroids produce their anti- edema effect by reducing the permeability of tumor capillaries. Dosing: 10MG BOLUS dosing; 4mg Q6 hours -> wean
WHAT COMES FIRST? - It is important to remember that the classifications of cerebral edema are not necessarily mutually exclusive. - Cytotoxic Edema -> Ionic Edema -> Vasogenic Edema -> Hemorrhagic conversion
THEN WHAT? Brain edema leads to worsening of ischemia, and often to herniation and death. Despite large-scale multinational interest in neuroprotection, hyperosmolar agents and supportive surgical procedures such as cerebrospinal fluid diversion and surgical decompression remain the only current treatments for brain swelling Advances in translational research now clearly identify cytotoxic edema as the initial, and most important, reversible first step in the sequence that leads to ionic edema, vasogenic edema, and complete hemorrhagic conversion.
TREATMENT Osmotherapy: most rapid and effective means of decreasing tissue water and brain bulk is osmotherapy Osmotic therapy is intended to draw water out of the brain by an osmotic gradient and to decrease blood viscosity. These changes would decrease ICP and increase cerebral blood flow (CBF). The treatment goal for cerebral edema is to maintain ICP below 20-22 mm Hg while maintaining a cerebral perfusion pressure (CPP) between 60 and 70 mm Hg
MANNITOL Mannitol is a sugar alcohol (C6H14O6) that decreases water and sodium reabsorption in the renal tubule and has been used for the reduction of ICP or cerebral edema since the 1960s. Mannitol lowers ICP through two distinct effects in the brain The first, The Rheological effect, reduces blood viscosity, and promotes plasma expansion and cerebral oxygen delivery. In response, cerebral vasoconstriction occurs due to autoregulation, and cerebral blood volume is decreased. The second effect occurs through creation of an osmotic gradient across the blood-brain barrier, leading to the movement of water from the parenchyma to the intravascular space. Brain tissue volume is decreased and, therefore, ICP is lowered. Mannitol also acts as an osmotic diuretic, leading to free water clearance and an increase in serum osmolality. As a result, water moves from the intracellular to the extracellular space, inducing a prolonged dehydrating effect. Reduction in ICP secondary to mannitol administration is dose-dependent, occurring within 10 to 20 minutes with a peak effect seen between 20 and 60 minutes and lasting between 4 to 6 hours. Mannitol is available in concentrations ranging from 5% to 25%, with 20% and 25% concentrations primarily used in acute ICP management. Dosing has historically ranged from 0.18 to 2.5 g/kg/dose (based on actual body weight); however, published literature has found that more significant ICP reductions and sustained responses occur when mannitol is dosed between 0.5 to 1.5g/kg/dose. Administration of mannitol can occur every 4 to 6 hours. It is typically administered over 20 to 60 minutes; however, faster administration can be used in acute ICP management. When concentrations >20% are administered, use of 0.22 micron in-line filter is required.
MANNITOL CONTINUED To prevent renal dysfunction, mannitol administration should be avoided when serum osmolality is >320 mOsm/L, but more specifically when the osmolar gap is >20 Mannitol frequently causes hypotension due to its diuretic effect, making administration in hemodynamically unstable patients less appealing. Acute hypotension is most commonly seen with rapid infusions (<5 minutes) and can be partially mitigated with the use of prolonged infusion rates (15 30 minutes).
HYPERTONIC SALINE Hypertonic saline has been utilized for almost a century now, with its first use being documented to decrease brain bulk in 1919 to its use for decreasing elevated ICP and increasing CPP in the late 1980s. The mechanism of action behind this effect has several proposed theories, with the most common involving the creation of an osmotic shift of fluid from the intracellular space to the interstitial and intravascular space. Typical plasma osmolarity ranges between 280 and 295 mOsm/L, while HTS osmolarity can vary from 1026 to 8008 mOsm/L depending on HTS concentration (3% 23.4%), leading to the osmotic fluid shift. Further mechanisms include direct vasodilation, increased cardiac output, and potential neurochemical and immune-modulating effects.
HYPERTONIC SALINE HTS has been studied in various concentrations ranging from the more commonly used 2% and 3% to higher concentrations of 5%, 7.5%, and 23.4%. HTS can be administered as a continuous infusion or given as a series of bolus infusions. It is important to note that these agents should preferably be administered through a central IV line, but there is evidence available for the use of 3% HTS through a peripheral IV line. HTS has a rapid onset as quick as 5 minutes with effects lasting up to 12 hours without any rebound ICP increase.
MONITORING HTS ADMINSTRATION Patients receiving continuous HTS infusions should have their serum sodium levels checked at least every 6 hr. The main objective of continuous HTS therapy is to provide an optimal osmolar gradient while avoiding the dangerous effects of hypernatremia. Maintaining serum sodium levels of 145- 155 mmol/L is likely to achieve this goal (Qureshi & Suarez, 2000; Qureshi et al., 1998; Qureshi et al., 1999). Serum sodium levels should be maintained no higher than 155 mmol/L. Higher levels are dangerous. Patients with serum sodium levels higher than 160 mmol/L are at increased risk for treatment-related renal failure, pulmonary edema, and heart failure (Qureshi & Suarez, 2000). If serum sodium levels remain above 160 mmol/L for more than 48 hr, the risk of these problems increases even more. Furthermore, if serum sodium levels climb beyond 160 mmol/L, patients are at risk for seizures (Qureshi et al., 1998).
CONTINUED MONITORING Serum osmolarity levels should also be monitored. HTS is an osmolar agent, and it directly affects serum osmolarity levels. These levels, which do not change as rapidly as serum sodium levels, should be checked every 12 hr while patients are receiving continuous HTS infusions The target serum osmolarity is less than 320 mOsmol/L. Fluid status also needs to be closely monitored with therapeutic goal being euvolemia
MANNITOL VS HTS The decision to use salt-based (HTS) or sugar-based (mannitol) osmotherapy has been a long-standing point of contention in hyperosmolar research. Mannitol was the historical treatment of choice; however, HTS has become established as the preferred initial option for the treatment of elevated ICP based on recent data. Clinical determination of treatment should consider the differences in adverse-effect profiles of each agent. Mannitol can cause hypotension secondary to osmotic diuresis, which could potentially be deleterious in patients who are hypotensive or hypovolemic. In contrast, HTS restores intravascular volume and may increase blood pressure as well as lowering ICP. Along with hypotension, mannitol may also be associated with an increased incidence of rebound elevated ICP. This concern is also present with HTS; however, data suggesting this potential side effect is limited. HTS causes hypernatremia, which raises concerns for potential development of CPM with rapid increases in sodium after a hyponatremic state. Changes in serum sodium should not exceed 12 mEq/L in a 24-hour period to further decrease the risk of CPM. Both mannitol and HTS carry the risk of AKI. Patients receiving HTS are at risk for AKI if they have serum sodium >160 mEq/L for a prolonged period. Nephrotoxicity secondary to mannitol is potentially due to osmotic nephrosis, but the risk can likely be avoided by insuring that the osmolar gap is <20 prior to administration. In addition to varying adverse-effect profiles, potential differences in efficacy may exist between HTS and mannitol. Three meta-analyses comparing the efficacy of HTS and mannitol have shown greater ICP reduction with HTS and a lower incidence of treatment failure. Further studies confirm that HTS reduces the number of treatment failures compared with mannitol. For ICP elevations >30 mm Hg, HTS provides a more rapid and sustained ICP reduction compared with mannitol. Thus, HTS may offer greater efficacy to reduce ICP when other therapies have failed.
MANNITOL VS HTS CONTINUED Clinically, HTS appears to be more efficacious than mannitol in reducing ICP both by degree and length of reduction. HTS also appears to improve tissue oxygenation of the brain more than mannitol. Multiple studies have now shown a somewhat counter-intuitive observation that brain cells exposed to a hypertonic mannitol gradient ultimately swell far above their initial resting volume. This response is both qualitatively and quantitatively different from that of cells exposed to simple hypertonic saline, where little or no rebound swelling is observed. Historically mannitol has been considered the gold standard for treatment of cellular or cytotoxic edema, but new recommendations from multiple national governing bodies promote use of HTS in both acute and prolonged settings of management. Up to clinical discretion.
TREATMENT COMPLICATIONS Electrolyte imbalances (i.e., hypernatremia, hyperchloremia, hypokalemia) and a hyperosmolar state These can cause central pontine myelinolysis (CPM), metabolic acidosis, cardiac depression, and congestive heart failure. Other safety issues that have been reported in published literature include acute kidney injury (AKI), rebound increases in ICP, seizures, altered mentation, coagulopathies, and infusion-rate related hypotension. Intravenous administration of HTS can also cause local effects such as IV infiltration, thrombophlebitis, tissue ischemia, and venous thrombus.
FUTURE TREATMENT There are a number of non-selective cation channel blockers show promising salutary effects in cerebral ischemia or ischemic stroke models Types include trivalent cations, verapamil derivates, flufenamic acid, the "typical" TRP blockers 2-APB, ACA and SKF 96365 as well as ASIC blockers
REFERENCES https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2740913/#R142 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2740913/#R142 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4923559/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4923559/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4665128/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4665128/ https://www.uspharmacist.com/article/hyperosmolar https://www.uspharmacist.com/article/hyperosmolar- -therapy cerebral cerebral- -edema edema therapy- -for for- -the the- -treatment treatment- -of of- - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4793889/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4793889/
REFERENCES http://medind.nic.in/maa/t03/i4/maat03i4p326.pdf http://medind.nic.in/maa/t03/i4/maat03i4p326.pdf https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4776312/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4776312/