Association of Renal and Cerebral Near-Infrared Spectroscopy with Adverse Outcomes in Single Ventricle Patients after Stage I Palliation
Study investigates the association between renal and cerebral near-infrared spectroscopy (NIRS) values and low cardiac output syndrome in single ventricle patients post Stage I palliation. Data from infants who underwent surgery between 2010-2019 is analyzed to determine correlations with adverse outcomes such as cardiac arrest, need for ECMO, and mortality. Results show significant incidence of low cardiac output and adverse events in the study cohort.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Are renal and cerebral near infrared spectroscopy associated with low cardiac output and adverse outcomes in single ventricle patients after Stage I palliation Richard U. Garcia, MD Cardiac Critical Care Children s Hospital of Michigan
Background Low cardiac output syndrome is not uncommon in infants after cardiac surgery Near-infrared spectroscopy (NIRS) is a non-invasive, continuous method of oximetry based on the varying wavelengths of oxygenate and deoxygenate hemoglobin evaluating differential regional absorption tissue of Cerebral NIRS monitoring has been advocated as a surrogate measure of saturation mixed venous oxygen After saturation is difficult to obtain Stage 1 Palliation, a true mixed venous
Aims To determine if postoperative cerebral and renal NIRS values are associated with low cardiac output (LCO) To determine the relationship between NIRS values and adverse outcomes: 1. Cardiac arrest 2. Need for ECMO 3. Mortality
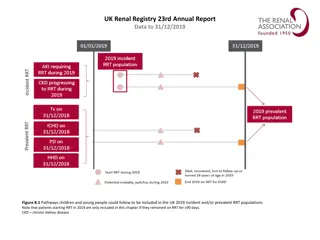
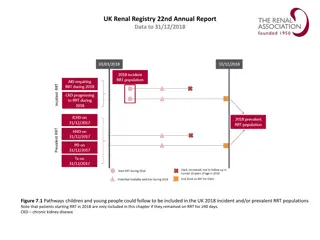
Methods Retrospective study approved by the Institutional Review Board, infants 6 months of age with single ventricle physiology who underwent stage 1 surgical palliation between January 2010 and December 2019 Cerebral and renal NIRS values at 1, 6, 12, 24 and 48 hours after surgery were recorded from the medical records Demographic data at the time of surgery and multiple perioperative variables were collected from the medical records
Methods LCO within the first 48 after surgery was defined as per the pediatric cardiac critical care consortium database: 1. Vasoactive inotropic score > 15 or tripling of the VIS at any point in the first 48 hours after surgery. 2. Documentation of LCO in the medical records by attending physician 3. A-V Saturation difference > 40% Cerebral and renal NIRS values were compared in patients with low and normal cardiac output as well as with other adverse outcomes such as cardiac arrest, need for ECMO and mortality
Results 91 patients with median (IQR) age of 10 days (6-26), weight of 3.3kg (3-3.5) and length of 51 cm (48.3-53) were included in the study Procedures Performed: Norwood with Sano shunt: 16 Norwood with right modified Blalock-Tausig shunt:18 Isolated aortopulmonary shunt: 57 LCO was seen in 42 (46%) patients in the first 48 post operative hours. Cardiac arrest: 20 (22%) VA ECMO: 16 (17%) Mortality: 15 (16.5%)
Results Cerebral NIRS at 6 hours (p=0.018), systolic blood pressure at 1 hour (p=0.04), and arterial lactate (p=0.024) at 1 hours remained independently associated with LCO after logistic regression analysis Cerebral NIRS of 57% at 6 hr had 91% sensitivity and 72% specificity in detecting LCO Mean cerebral NIRS saturation of 55% during the first 24 hours had 81% sensitivity, and 60% specificity to determine LCO There was no independent association between cerebral or renal NIRS with adverse outcomes such as cardiac arrest, need for ECMO and mortality.
Results Patients who underwent the Norwood procedure had significant higher incidence of: LCO p< 0.001 Need for ECMO p= 0.007 Mortality p= 0.001 Composite adverse outcome p= 0.005 In the Norwood and aortopulmonary shunt group, cerebral NIRS values at 6 hours after admission to the cardiac intensive care unit were associated with LCO
Results Norwood procedure (n = 34) Aortopulmonary Shunt (n = 57) Variables (mean (SD) or n %)* p value Age, days 6 (4) 32.6 (42) 0.002 Weight, kg 3.3 (0.7) 3.45 (0.6) 0.303 Length, cm 51 (3.1) 51.2 (3.3) 0.747 Gestational age, weeks 38.3 (1.3) 37.8 (2.1) 0.169 CPB time, min 265.9 (84) 101.3 (75.7) <0.001 Duration on MV, days 23.9 (23.9) 13.5 (12.8) 0.034 Length of Hospital stay, days 71.8 (69.3) 41.54 (51.8) 0.018 Low cardiac output 26 (76.5%) 16 (28.1%) <0.001 Cardiac arrest 11 (32.3%) 9 (15.8%) 0.091 VA ECMO 10 (29.4%) 5 (8.8%) 0.007 Mortality 11 (32.3%) 4 (7%) 0.001 Composite adverse outcome 15 (44.1%) 10 (17.5%) 0.005
Conclusions Cerebral NIRS 57% at 6 hours and mean cerebral NIRS 55% during the first postoperative day were indicative of LCO No association between NIRS values and adverse outcomes Future prospective studies may be necessary to determine whether NIRS directed interventions can improve postoperative outcomes
Acknowledgments Sanjeev Aggarwal, MD Pezad Doctor, MD