Acute kidney injury
Definition, staging, and complications of acute kidney injury (AKI) with Dr. Abdul Lateef. Understand the diagnostic parameters for differentiation and the evaluation process. Explore the etiological classification and common signs and symptoms of AKI.
Uploaded on Dec 22, 2023 | 6 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Acute kidney injury Dr Abdul Lateef PGR M -1
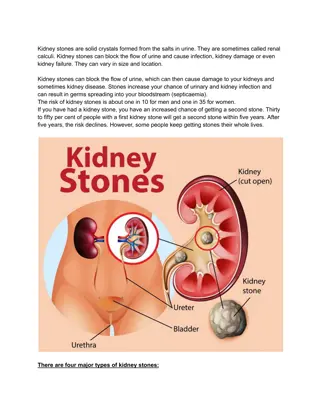
Definition of AKI AKI is defined as any of the following Increase in SCr by >0.3mg/dl (>26.5lmol/l) within 48 hours; or Increase in SCr to >1.5 times baseline, which is known or presumed to have occurred within the prior 7 days; or Urine volume <0.5ml/kg/h for 6 hours.
Definitions Azotemia = Elevation of the blood urea nitrogen level (BUN) This compound is one of many nitrogen based molecules that accumulates in AKI and CKD and may lead to the development of uremia. Uremia = The clinical side effects of excess accumulation of nitrogenous compounds (uremic toxins) Nausea,vomiting, confusion, anorexia, seizures Oliguria= <500 mL of urine output in 24 hours Anuria= < 50 mL of urine output in 24 hours
Evaluation History: meds, contrast, or other nephrotoxins; PO intake, Hypotension, infection/sepsis; trauma, rhabdomyolysis; BPH/retention Any history of volume loss i.e vomiting diarrhea, peritonitis, pancreatitis,hot environment and burns. Search for insult 24 48 hr prior Cr. Physical examination: Assess volume status of patient i.e Physical signs of orthostatic hypotension,tachycardia, Reduced JVP, skin turgor, And dry mucous membranes.
Sign and symptoms Peripheral edema,wight gain Nausea/voming/diarrhea/anorexia Mental status changes, fatigue Astrexis,Encephalopathy,seizures Fever, rash, arthralgias: drug induced or lupus nephris Shortness of breath Pruritus Volume depletion (prerenal AKI) Weight loss (prerenal AKI) Anuria alternating with polyuria (postrenal AKI) Abdominal pain radiang from flank to groin (postrenal AKI)
Work up Serum creatinine,serum electrolytes,ABGs ,ECG Urine evaluation: 24 hours urine output, urinalysis ( sediments, electrolytes, osmolality and fractional excretion of sodium. Renal ultrasound and CT to rule out obstruction and cortical atrophy in ckd. Serology if indicated Renal biopsy if etiology is unclear
Monitoring of patients with AKI Record Input and Hourly urine output to assess daily fluid balance Carefully monitor Daily weight of patient Daily serum creatinine, BUN,serum electrolytes ECG monitoring to avoid any arryhtmias Daily Ionized calcium and Total serum calcium And phosphate Monitor blood pressure,Heart rate and MAP
Management Short-term goals: Resuscitation and improve hydration status to maintain adequate cardiac output and tissue perfusion. Minimize the degree of insult to the kidney Reduce extrarenal complicaons. The ulmate goal: is to have the patient s renal function restored to the pre- AKI baseline. Prerenal sources of AKI should be managed with hemodynamic support and volume replacement. Postrenal therapy focuses on removing the cause of the obstrucon. Whereas treatment of intrinsic renal failure is more supportive in nature. Fluid, electrolyte, and nutrional support, RRT, and treatment of nonrenal complicaons such as sepsis and GI bleeding
Therapeutic options Eliminating medications associated with kidney damage Improving cardiac output and renal blood flow Hydration: Maintain intravascular volume: crystalloids such as isotonic saline or balanced solutions, Avoid too much fluid administration which can result in interstial edema, increased intra-abdominal pressure, renal venous congestion, and decreased GFR. Keep the patient Euvolemic If dehydraon is evident: fluid replacement therapy (oral or IV) Urine output 0.5 mL/kg/h is generally targeted during the inial fluid resuscitaon phase Consider slower rehydraon in anuric & oliguric patients to avoid pulmonary edema (100 ml/ hr).
Cntd Isotonic sodium chloride plus 50 mEq (50 mmol) of sodium bicarbonate per liter, administered as boluses followed by a continuous infusion (200 mL/h) until rehydration is complete. Intrinsic or post-obstructive AKI involve fluid and electrolyte management In ICU patients with vasomotor shock , vasopressors such as norepinephrine, vasopressin, or dopamine may be used in conjunction with fluids in order to maintain adequate hemodynamics and renal perfusion
Electrolyte Management Hypernatremia and fluid retention are frequent complications of AKI Hyperkalemia: most common Monitor K: more than 6mmol/l can lead to arrhythmias Phosphorus and magnesium. Both are eliminated by the kidneys and are not removed efficiently by dialysis. Restrict in diet Calcium-containing antacids should be avoided to prevent precipitation of calcium phosphate in the soft tissues.
Renal replacement therapy Can be administered either intermittently (IHD) or continuously (CRRT) Early RRT should be considered when life-threatening changes in fluid, electrolyte, and acid base balance are present IHD: is the most frequently used RRT Advantages: rapid removal of volume and solute and correction of most of the electrolyte abnormalities associated with AKI. The primary challenge is hypotension The use of daily versus three times weekly IHD in AKI is associated with a reduction in hypotension risk and a faster recovery