Acute Kidney Injury: Implications for Nurses
Acute Kidney Injury (AKI) is a sudden decline in kidney function with serious implications, including high mortality rates and significant healthcare costs. This content explores the definition, causes, and risks associated with AKI, emphasizing the importance of early detection and management in both community and practice nursing settings.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Acute Kidney Injury and the implications for community and practice nurses Claire Stocks Sister, Cardiac Arrest Prevention Team, County Durham & Darlington Foundation Trust
Disclaimer..Im no expert! | 2 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Learning Outcomes Define Acute Kidney Injury (AKI) Discuss the potential causes of AKI Top Tips for nurses | 3 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Is AKI really a problem? 100,000 deaths are year are associated with acute kidney injury. (NCEPOD 2009) Approximately 65% of Acute Kidney Injury Starts in the Community. (Selby et al 2012) Costs to the NHS estimated to be 1 billion per year. (Kerr et al 2014) | 4 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
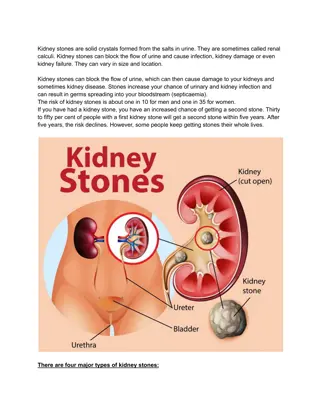
Acute Kidney Injury Acute kidney injury (AKI) is the sudden and recent reduction in kidney function resulting in a inability to maintain fluid, electrolyte and acid base balance. AKI is a syndrome that usually occurs in the presence of other acute illness such as SEPSIS or HEART FAILURE. Diagnosis of AKI is based on either the urine output or the creatinine level (or both) AND clinical assessment, history, presentation. | 5 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Risk of AKI Aged 75 or over Cardiac Disease Liver Disease Diabetes Chronic Kidney Disease Cancer Acute insult from conditions such as Sepsis. Patients susceptible to dehydration | 6 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Causes.. Pre Renal Most common cause of AKI Flow disruption to the kidney For example: Low blood pressure Heart Failure Low blood volume Blood flow reduced | 7 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Causes. Intrinsic Damage to the kidney itself For example: Glomerulonephritis Acute tubular Necrosis | 8 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Causes. Post Renal A consequence of urinary tract obstruction. For example: Blocked catheter Renal calculi Bladder tumours | 9 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Treatment of AKI Treatment of AKI is about identifying the cause and formulating a treatment plan to address this. Usually AKI requires fluid replacement. It is therefore essential that clinical assessment of fluid status has been completed. It a patient is hypotensive and hypovolaemic IV supplementary fluid will be required. Medications may need to be with held for a few days until the acute insult is recovering. A renal ultrasound should be considered. Fluid balance should be monitored alongside vital signs. Dipstick Urine and document the results in the patients medical record. Referral to renal teams may be indicated if the cause of AKI is unknown, or the patients AKI is severe or not responding to treatment, or the patient has had a renal transplant. Referrals to specialities should be senior clinician to senior clinician. Patients with life threatening complications (Acidosis, Pulmonary Oedema, Hyperkalaemia or uraemia should be referred to specialist services for possible renal replacement therapy. For further information regarding recognition and management of AKI see NICE CG169. | 10 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Top Tips for Nurses regarding Acute Kidney Injury 1) Maintain a healthy blood pressure. The kidneys play a pivotal role in the regulation of blood pressure through salt and water balance. Blood pressure that is too high or too low will ultimately lead to damage within the kidneys so its important to keep patients blood pressure within normal range. Pre-renal AKI is often due to hypo perfusion and low blood pressure. For any patients with low blood pressure they must be assessed and discussed with the GP as they may need escalation into hospital for treatment. Not all pre renal AKI is a consequence of dehydration. Worsening heart failure will reduce cardiac output thus resulting in a lower BP. Be aware of your patients who have established heart failure and ensure they are reviewed regularly by the GP. For further information regarding hypertension in adults see NICE CG127 Hypertension. | 11 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Top Tips for Nurses regarding Acute Kidney Injury 2) Urinalysis might alert you to an intrinsic kidney problem. Protein and blood should not filter through to the urine therefore if it is present on a urinalysis test this could indicate signs of renal disease. If more than 3+ of protein or blood is present discuss with your GP about what to do next. | 12 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Top Tips for Nurses regarding Acute Kidney Injury 3) Medication review is essential. UK Renal Pharmacy Group AKI Medicines Optimisation Toolkit (March 2012) Consider Acute Nephrotoxic Drug Action Contrast Media Ace Inhibitors NSAID s Diuretics ARB s Be aware of other drugs excreted by the kidneys such as Metformin, Opioids, Some antibiotics, Digoxin & Lithium. | 13 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Top Tips for Nurses regarding Acute Kidney Injury 4) Hydration is key. Dehydration is the underlying cause of many common conditions including: constipation; falls; urinary tract infections; pressure ulcers; malnutrition; incontinence; confusion and pre renal AKI. The elderly are more prone to dehydration because as we age we lost the ability to recognise thirst. Other factors such as poor mobility and reduced confidence can also affect a patients desire to keep hydrated. Elderly patients are likely to have more co-morbidities and poly pharmacy which could be attributed to worsening AKI. Education to patients and carers regarding hydration and medications is vital. Some patients may need further support in staying hydrated. For example patients may need beakers instead or cups or carer input to maintain fluid intake throughout the day. It could be as simple as set drink routines rather than relying on thirst alone. Signs of dehydration include: Thirst, sunken eyes, irritability, confusion, cool peripheries, low BP, Raised HR, headaches, reduced skin turgor, dry mucus membranes. | 14 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Top Tips for Nurses regarding Acute Kidney Injury 5) Consider the Kidneys in everything you do. The kidneys don t usually complain. The kidneys can lose up to 90% of their function before you may even begin to notice. The kidneys are clever organs but need a good blood supply to work effectively. Consider the kidneys in your daily visits. Ask if your patient has passed urine? Ask if they are well hydrated. Consider if your patient has risk factors for AKI and whether further investigations such as monitoring of creatinine levels are required. Consider if your patient has an acute insult that may warrant temporary cessation of medications. Consider further review by GP. | 15 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
Further Information References: Kerr M, Bedford M, Matthews B, O Donoghue D. The economic impact of acute kidney injury in England. Nephrol Dial Transplant (2014) 29: 1362 1368. National Confidential Enquiry into Patient Outcome and Death (NCEPOD) 2009. Acute Kidney Injury: Adding Insult to Injury. National Institute for Health and Care Excellence (NICE) 2013, Clinical guideline 169, Acute Kidney Injury. Selby NM, Crowley L, Fluck RJ, McIntyre CW, Monaghan J, Lawson N, Kolhe NV. Use of electronic results reporting to diagnose and monitor AKI in hospitalized patients. Clin J Am Soc nephrol. 2012 Apr;7(4):533-40. doi: 10.2215/CJN.08970911. Epub 2012 Feb 23 | 16 Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date
For further information regarding Acute Kidney Injury please see the Think Kidneys Website www.thinkkidneys.nhs.uk
Contact Think Kidneys How to find out more Richard Fluck National Clinical Director for Renal NHS England Richard.fluck@nhs.net Karen Thomas Think Kidneys Programme Manager UK Renal Registry Karen.Thomas@renalregistry.nhs.uk www.linkedin.com/company/think- kidneys www.twitter.com/ThinkKidneys Joan Russell Head of Patient Safety NHS England Joan.russell@nhs.net Teresa Wallace Think Kidneys Programme Coordinator UK Renal Registry Teresajane.Wallace@renalregistry.nhs.uk www.facebook.com/thinkkidneys www.youtube.com/user/thinkkidneys www.slideshare.net/ThinkKidneys Ron Cullen Director UK Renal Registry Ron.cullen@renalregistry.nhs.uk www.thinkkidneys.nhs.uk Julie Slevin Think Kidneys Programme Development Officer UK Renal Registry M 07810560766 | E julie.slevin@renalregistry.nhs.uk Acute Kidney Injury National Programme | Implications for community & practice nurses | Claire Stocks Date | 18