A diagnostic framework for hypercalcaemia
A diagnostic framework for hypercalcaemia through a clinical case analysis targeting medical students and above. Learn to assess symptoms, outline investigation pathways, and recognize common causes of high calcium levels. Dive into interpreting bone profiles and determining the best diagnostic test.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
A diagnostic framework for hypercalcaemia Dr. Mark Jacunski (FY2) Dr. Roby Rajan (ST7) Dr. Alex Graveling (Consultant) Aimed at 4thyear medical students and above
Learning outcomes By working through this case you will be working on your ability to: 1) Target your history and examination for the diagnosis of hypercalcaemia 2) Outline the investigation pathway for hypercalcaemia 3) Remember the two most common types of causes of hypercalcaemia 4) Recognise less common factors causing hypercalcaemia
You see a 54 year-old woman on the ward round The junior doctor gives a short description outside the room: She was admitted 2 days ago with breathlessness for a community acquired pneumonia We have been giving her amoxicillin and clarithromycin and she feels much better. She has been haemodynamically stable and afebrile Her bloods are all going in the right direction (CRP and WBC previously raised but trending down). But her calcium is high, though she didn t have any symptoms Her only other relevant history is that she has a 30 pack-year smoking history
Other blood tests In addition to calcium levels, what are the two other blood tests that are routinely part of a bone profile ?
No other symptoms? The junior doctor mentioned that there were no other symptoms. What might you expect in hypercalcaemia? This is often encapsulated by a mnemonic: _ _ _ones _ _ones _ones _ _oans _ _ _ _ _ _ _one _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ones
The patients bone profile comes back It looks truly out of range, not borderline, remarks the junior doctor with utter conviction Test Patient s result Normal range Calcium 3.02 2.20-2.60 mmol/L The majority of cases hypercalcaemia can be explained by two categories of conditions. What are they? Click below for hints Answer Phosphate 0.70 0.80-1.50 mmol/L Alk Phos 245 30-130 units/L Hint 1 Hint 2
What is the best next test to lead to the diagnosis? (Single best answer) A) Immunoglobulins and serum electrophoresis B) CT chest-abdomen-pelvis C) Parathyroid hormone D) 25-hydroxycholecaciferol (25-OH-vitamin D) E) Urea & electrolytes
Before finding out the answer, lets think about why hypercalcaemia happens This patient does not have chronic kidney disease and has not had longstanding hypocalcaemia. Assuming parathyroid hormone is still elevated, this would suggest a primary source (or rarely, ectopic). What are the causes of primary hyperparathyroidism?
Before finding out the answer, lets think about why hypercalcaemia happens This patient does not have chronic kidney disease and has not had longstanding hypocalcaemia. Assuming parathyroid hormone is still elevated, this would suggest a primary source (or rarely, ectopic). Bonus question (more relevant for 5th years and for postgraduate knowledge): Do you know of any genetic conditions linked to primary hyperparathyroidism?
Before finding out the answer, lets think about why hypercalcaemia happens The percentages and precise mechanisms may be outside the scope of what is expected as a medical student, but are written here for completeness and interest What are the causes of hypercalcaemia of malignancy?
Before finding out the answer, lets think about why hypercalcaemia happens Lastly, what sorts of conditions account for the outlying 10% of causes? Use the hints to help guide your answers (in no particular order) Hint 1 Answer 1 Hint 2 Answer 2 Hint 3 Answer 3 Hint 4 Answer 4 Hint 5 Answer 5 Hint 6 Answer 6
Back to our case! PTH results are as shown in the chart. What is the most likely diagnosis? (Single best answer) A) Multiple myeloma B) Squamous cell carcinoma of the lung C) Breast cancer D) Primary hyperparathyroidism due to a parathyroid adenoma E) Secondary hyperparathyroidism Test Patient s result Normal range Calcium 3.02 2.20-2.60 mmol/L Phosphate 0.70 0.80-1.50 mmol/L Alk Phos 245 30-130 units/L PTH 6.0 1.6-7.2 pmol/L
The patient most likely has a parathyroid adenoma The patient most likely has a parathyroid adenoma. The corrected calcium is elevated and phosphate decreased. PTH is therefore inappropriately high. Test Patient s result Normal range Calcium 3.02 2.20-2.60 mmol/L Phosphate 0.70 0.80-1.50 mmol/L Alk Phos 245 30-130 units/L PTH 6.0 1.6-7.2 pmol/L Are you satisfied with this diagnosis?
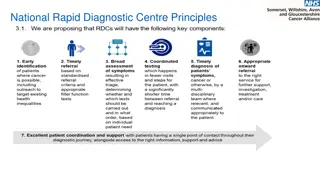
Investigation Algorithm Hypercalcaemia Recheck calcium & albumin, ensure corrected calcium calculated PTH normal or increased (inappropriate) PTH low (appropriate) Check PTH 90% of cases Primary hyperparathyroidism or Familial hypocalciuric hypercalcaemia (rare) or tertiary hyperparathyroidism (renal failure) Malignancy Drug causes
Further work-up and diagnosis Other features of her history, examination, laboratory results may prompt further work-up to rule out a malignancy . Apart from being a smoker, it would be sensible specifically ask about breast, lung, and renal cancer risk factors and examine accordingly. Immunoglobulins and electrophoresis would possibly be done for completeness, if PTH levels were equivocal or low. Myeloma screening is more appropriate in elderly patients presenting with anaemia, bone pain or deranged renal functions. Most community acquired pneumonia will be followed up with further imaging in 6-8 weeks (usually chest X-ray), which can help identify cancers previously hidden by consolidation
Definitive management Which of the following would be appropriate in the management of this patient? Fluid repletion Loop diuretics Thiazide diuretics Bisphosphonates Calcitonin Parathyroidectomy Cinacalcet Alfacalcidol Cholecalciferol Steroids
Outcome The calcium levels normalised with adequate hydration. She wanted to avoid neck surgery. She remained asymptomatic but a DEXA scan identified osteoporosis and she agreed to be referred for parathyroidectomy, which she underwent without adverse effect. A follow-up chest radiograph was performed 6-8 weeks later, the consolidation had resolved and there was no suggestion of an underlying mass lesion. This admission was nonetheless a teachable moment , and she undertook a smoking cessation programme.
Learning outcomes By working through this case you will be working on your ability to: 1) Target your history and examination for the diagnosis of hypercalcaemia 2) Outline the investigation pathway for hypercalcaemia 3) Remember the two most common types of causes of hypercalcaemia 4) Recognise less common factors causing hypercalcaemia
Further resources https://litfl.com/hypercalcaemia/ https://emcrit.org/ibcc/hypercalcemia/ https://www.endocrinology.org/media/4277/emergency- guidance_acute-hypercalcaemia-in-adults.pdf https://cks.nice.org.uk/topics/hypercalcaemia/