Extended Endocrine Therapy Guidelines for Breast Cancer Patients
Extended adjuvant endocrine therapy may benefit breast cancer patients with poor or intermediate prognosis, but may have little value for those with good prognosis. Risks include osteoporosis and venous thromboembolism. Different treatment options are available for postmenopausal and premenopausal women, requiring consideration based on individual patient status. Regular monitoring and assessment are recommended to optimize patient care.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
SWAG guidelines Mark Beresford
Oncotype DX testing in network Node negative NICE approved Node positive variable usage geographically since COVID access
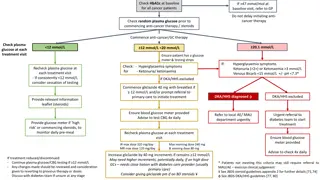
Extended endocrine letter Extended Endocrine Therapy in Breast Cancer Extended adjuvant endocrine therapy may be considered for patients who have already completed 5 years of endocrine treatment for early breast cancer. This does not usually require a further secondary care review please follow the guidelines below. Extended treatment is likely to be of overall statistical benefit for patients who presented with poor or intermediate prognosis carcinomas, but of little or debatable value for patients who presented with good prognosis carcinomas (tumours less than 2cm, Grade 1 or 2 with clear lymph nodes). The risks of extended treatment include osteoporosis (aromatase inhibitors, AI) or venous thromboembolism and endometrial carcinoma (tamoxifen). Stopping at 5 years is a good option for all patients who are experiencing side effects that impact on quality of life. Extended treatment options after 5 years of treatment Postmenopausal women: The majority of postmenopausal women will have been treated with an AI (anastrozole or letrozole) which may be continued to a total of 7 years if well tolerated. Trials have shown no additional reduction in breast cancer recurrence by continuing to 10 years, but an increase in bone fractures*. For women continuing beyond 5 years a repeat bone density assessment (DEXA scan) is advisable. Patients that have taken tamoxifen for 5 years may continue on tamoxifen or switch to an AI. Women who have previously switched at 2-3 years should continue on the drug they are receiving to a combined total of 7 years. Pre or Perimenopausal women: Pre- and peri-menopausal women can continue on tamoxifen for up to a maximum of 10 years. Consideration may be given to reassessing menopausal status at years 2-5 for perimenopausal women, with a view to switching to an AI if confirmed postmenopausal. However menopausal statusis difficult to determine whilst on endocrine treatment. FSH can be suppressed and oestradiol levels raised by tamoxifen. Caution should be exercised before recommending an AI for patients who have become amenorrhoeic whilst on treatment, particularly for women <50 years of age and an FSH should be checked after 3 months to confirm >35IU/L. Whenever there is reasonable doubt whether a woman has become permanently postmenopausal she should continue on tamoxifen. High risk premenopausal women may have been started on a GnRHa with either an AI or tamoxifen. The GnRHa should be stopped at 5 years post-surgery and endocrine treatment can be extended with a further 5 years of treatment, using tamoxifen alone. If a woman at high risk wishes to continue endocrine treatment but has unmanageable side effects please consider referral to the Oncology Menopause Service. (ruh-tr.oncologymenopauseservice@nhs.net)
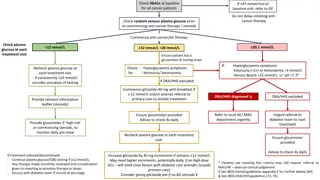
Extended adjuvant endocrine therapy may be considered for patients who have already completed 5 years of endocrine treatment for early breast cancer. This does not usually require a further secondary care review please follow the guidelines below. Extended treatment is likely to be of overall statistical benefit for patients who presented with poor or intermediate prognosis carcinomas, but of little or debatable value for patients who presented with good prognosis carcinomas (tumours less than 2cm, Grade 1 or 2 with clear lymph nodes). The risks of extended treatment include osteoporosis (aromatase inhibitors, AI) or venous thromboembolism and endometrial carcinoma (tamoxifen). Stopping at 5 years is a good option for all patients who are experiencing side effects that impact on quality of life.
Extended treatment options after 5 years of treatment Postmenopausal women: The majority of postmenopausal women will have been treated with an AI (anastrozole or letrozole) which may be continued to a total of 7 years if well tolerated. Trials have shown no additional reduction in breast cancer recurrence by continuing to 10 years, but an increase in bone fractures*. For women continuing beyond 5 years a repeat bone density assessment (DEXA scan) is advisable. Patients that have taken tamoxifen for 5 years may continue on tamoxifen or switch to an AI. Women who have previously switched at 2-3 years should continue on the drug they are receiving to a combined total of 7 years.
Pre or Perimenopausal women: Pre- and peri-menopausal women can continue on tamoxifen for up to a maximum of 10 years. Consideration may be given to reassessing menopausal status at years 2-5 for perimenopausal women, with a view to switching to an AI if confirmed postmenopausal. However menopausal status is difficult to determine whilst on endocrine treatment. FSH can be suppressed and oestradiol levels raised by tamoxifen. Caution should be exercised before recommending an AI for patients who have become amenorrhoeic whilst on treatment, particularly for women <50 years of age and an FSH should be checked after 3 months to confirm >35IU/L. Whenever there is reasonable doubt whether a woman has become permanently postmenopausal she should continue on tamoxifen. High risk premenopausal women may have been started on a GnRHa with either an AI or tamoxifen. The GnRHa should be stopped at 5 years post-surgery and endocrine treatment can be extended with a further 5 years of treatment, using tamoxifen alone. If a woman at high risk wishes to continue endocrine treatment but has unmanageable side effects please consider referral to the Oncology Menopause Service. (ruh-tr.oncologymenopauseservice@nhs.net)
Adjuvant abemaciclib Projected estimates for the introduction of a new cohort of patients on treatment for 2 years High risk ER+ve adjuvant We decided that it would be plausible that 50% of all HR+HER2- EBC patients who have had chemotherapy could be eligible for abemaciclib Therefore assume that once the new CDKI treatment has been in use for 2+ years, the following data would apply: Bath data: estimated 390 new EBC patients presenting each year 160 of these patients are referred to SACT 65 are HR+HER2- patients 45 HR+HER2- patients go on to have chemotherapy 23 HR+HER2- patients are considered high risk and could start Abemaciclib treatment
Abemaciclib eligible patient group We assume for our modelling purposes that the Abemaciclib eligible patient group will make up 50% of those HR+HER2-EBC patients falling within the 34% of all diagnosed early breast cancer patients requiring chemotherapy group. Abemaciclib follow-up schedule We assume that HR+HER2-EBC patients who are started on Abemaciclib will require 1-monthly medic role SACT oncology follow-up for the first 6 months of treatment and 3-monthly medic role SACT oncology follow-up thereafter until the 2-year treatment course is complete. We also assume that the Abemaciclib will be started an estimated 4 weeks after any primary chemotherapy or radiotherapy course is completed, so during month 7 or 8 of a patient s first year within the SACT oncology service. Abemaciclib drop-out rate: We assume that the estimated Abemaciclib patient drop-out rate will be the same as that witnessed within the MonarchE study which was 17.2%. We also assume that these 17.2% of patients will all need at least one month s worth of bloods and medic role oncology follow-up prior to discontinuing treatment. Only 2.8% of patients dropped out in the first month, with the remaining 14.4% of patients stopping treatment over the course of the 2 years. Patient demand is based on the drop-out rate seen over the two years.
Bath Total number of patients on new treatment (new, year 1 and year 2) 61 Number of follow-up appointments required per year 249 Number of follow-up appointments required per week 6