Handling Challenges with a Difficult Doctor
In dealing with a doctor facing various difficulties and behavioral issues, it is crucial to follow principles of fairness, confidentiality, and effective communication. Utilize available resources such as HR guidance, MSF feedback, and support from colleagues. Consider risks to both the doctor, patients, and colleagues, and maintain a clear, documented plan to address concerns and ensure the well-being of all involved parties.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Working with a Dr with Difficulties
TIMELINE FEB Didn t turn up for regional event hosted by own Consultant said was there when challenged. Didn t work the night shift Time owed to dept paid back MAR Late When challenged about being on time, said working elsewhere Reporting to senior when arrives APR Multiple concerns raised by nurses Distracted behaviour, disappearing concerns re mental health raised Not seeing patients asked to. Failing to self-care Sent home sick several times by senio Informal meeting Occ Health referral Time off JUN DNA Occ Health review letter written but received by dept 3/52 later Further instances of lateness. Provable that reason was not true Formal letter from Consultant colleague raising concerns, times & dates provided Formal meeting with HR present AUG Changeover. Dr pursued alternative career
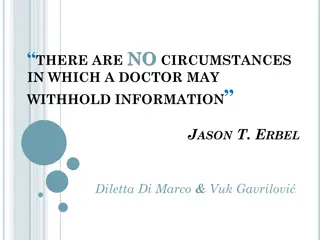
PRINCIPLES Be fair to both sides as it is likely there are facts you do not know: Follow Trust guidance, use HR expertise Avoid constructive dismissal What do you want your endpoint to be? What is best for patients, dept & that person Confidentiality But ensure those who need to know do in order to avoid undermining the interventions you are using
Drs specifics- who is available for advice? HR Responsible Officer GMC What tools do you have? MSF person to choose who asked. Can be used to disprove a general problem, too ES / CS College Tutor & TPD now available if trainee PSU - if trainee Occ Health self-referral vs management referral
TO Consider Risks to patients Underperforming Drs Not fitting in with system & processes Interpersonal skills Burden on colleagues If you need time off sick, you need time off sick. Cover can be arranged
Risks to Dr Continued deterioration Insight or guilt eg asking to stay late, may not be in best interests Should not be doing extra or later shifts at risk to normal shifts Risks to Others Driving Colleagues left with unexpected rota gaps
1. Importance of having everything in writing Cannot act on hearsay & rumour, or unless something happens Must have proof Accumulation of concerns may start small Not witch-hunt / bullying. Have to keep that person at the centre Leadership 2.Importance of clear plan eg Lateness - report to senior Everyone understands acting together no mixed messages /not being undermined. Not punitive
3. DOCUMENTATION Minimises comeback. Can demonstrate being fair Same format & reason as clinical notes Especially if lack of insight 4. Often multiple areas of concern Clinical , reliability / teamworking ePortfolio 5. Is this a Dr with difficulties / Dr in difficulty
SUMMARY Principles applicable to many other situations Curriculum Prioritisation of patient safety Team working & patient safety Communication & co-operation with colleagues CC15 Personal Behaviour Medical Ethics & confidentiality CC7 CC8 NTS CC24 CC17