Understanding Selenium Toxicity in Animals: Sources, Mechanism, and Clinical Signs
Selenium toxicity in animals can occur through various sources such as selenium-containing plants. The toxicokinetics involve absorption from the gut and distribution to different body parts. The mechanism of toxicity is linked to the incorporation of selenium in amino acids and proteins, leading to adverse effects. Clinical signs of selenium toxicity include acute gastrointestinal symptoms and subacute manifestations like blind staggers. Identifying and addressing selenium toxicity is crucial for animal health.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
SELENIUM TOXICITY Presented by:- Dr.Archana Assistant Professor_cum_Jr .Scientist Deptt.Of Pharmacology & Toxicology Bihar Veterinary College, Patna
Content of chapter * Sources * Toxicokinetic * Mechanism of toxicity * Clinical Signs * Treatment
Source :- Classification of selenium containing plants Obligate indicator plants : Require large amounts of selenium (10,000 15000 ppm) for growth and survival. These plants can accumulate high concentrations of selenium as water-soluble amino acid analogs of cysteine and methionine. E.g - Astralagus , Oonopsis & Xylorhiza. Facultative indicator plants: Absorb and tolerate large amounts of selenium (1500 ppm) if it is present in the soil, but they do not require selenium for growth. E.g - Sideranthus, Aster & Atriplex . Passive accumulator plants: May accumulate selenium if grown on seleniferous soils, especially where selenium ( 20 60 ppm) has been brought to the soil surface, while other plants cannot tolerate selenium and are stunted or killed by it. E.g - Corn, Wheat & Barley
Toxicokinetics :- Se is readily absorbed from the gut and distributed throughout the body particularly to the liver kidney and spleen. Chronic exposure results in large concentration in hairs and hooves. Se can cross the placental barrier in mammals and also enters into avian eggs causing foetal malformation and embryonic defects. Se does not penetrate in intact skin but may penetrate abraded or diseased skin.
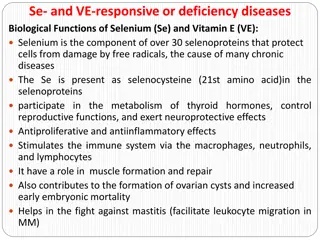
Mechanism of toxicity Acute or sub-acute G.I signs may probably result in parts from the irritant nature of Se in large concentration. The main mechanism of selenium is due to the incorporation of Se instead of Sulphur in some amino acids (Cysteine & Methionine) and in important proteins and enzymes containing SH group and possibly in other compounds containing Sulphur. Abnormal Se or other Se compounds are responsible for the chronic Se toxicosis as well as its carcinogenic effects.
Clinical Sign Acute Due to ingestion of obligate indicator plants clinical signs are noticed in 1 2 hours and animals may die between 2 hours to 7 days. Symptoms include rapid heart beat, dyspnoea, colic, bloat, dark watery diarrhoea, fever, weak pulse, pale and cyanotic mucous membrane are the cardinal signs followed by death from respiratory failure within a few days. Subacute (Blind staggers) (This condition in cattle manifested in three stage) Occurs due to ingestion of seleniferous plants and may develop after a relatively short period. Poor appetite, staring coat, wander aimlessly, circling, gradual loss of vision disregarding obstacles and stumbling over them or walking through them. Respiration and temperature are normal. In the second stage depression, in-coordination and fore leg weakness, animal goes down on its knees. In the third stage colic, subnormal temperature, emaciation, swollen eyelids, near blindness. Salivation, lacrimation, severe abdominal pain, inability to swallow, complete paralysis, collapse and death have also been reported.
Continue Chronic (Alkali disease) The name alkali disease has been attributed to consumption of alkali waters. Chronic poisoning is caused by daily ingestion of cereals, grains and other forage plants containing selenium. Lameness, hoof and hair abnormalities, partial blindness, paresis, in- coordination, emaciation and lethargy may be noticed. Lameness is due to erosion of the articulate surface of long bones. Hoof begins to shed. Shedding is incomplete and old hoof fuses with new hoof and form abnormally long rocker shaped hoof. In horses there will be loss of long hair from the mane and tail will occur. In cattle, there will be a rough coat, dullness and lack of vitality and emaciation with deprived appetite.
Diagnosis & Treatment Diagnosis Diagnosis is based on clinical signs and estimation of selenium in whole blood and liver. Elevated glutathione peroxidase level in liver and blood suggest Se poisoning. Treatment There is no specific antidote for Se toxicosis symptomatic & supportive care of affected animals should be started as early as possible. Removal of the source and high protein diet are said to be useful. Addition of inorganic arsenicals enhances biliary excretion of selenium and increasing the dietary levels of sulphur containing proteins is also beneficial.
Cadmium Toxicity Commercially, Cd is used in television screens, lasers, batteries, paint pigments, cosmetics, and in galvanizing steel, as a barrier in nuclear fission, and was used with zinc to weld seals in lead water pipes prior to the 1960s. It impair Vitamin D metabolism in the kidney with deleterious impact on bone. This effect, coupled with direct Cd impairment of gut absorption of calcium and derangement of collagen metabolism, can produce osteomalacia and/or osteoporosis . The most extreme example of this process is itai-itai disease in Japan, which combines severe pain from osteomalacia with osteoporosis, renal tubular dysfunction, anemia, and calcium malabsorption EDTA significantly increased urinary elimination of cadmium.