The Economic Impact of Delayed Diagnosis of Axial Spondyloarthritis in the UK
Delayed diagnosis of axial spondyloarthritis in the UK leads to significant physical, emotional, and financial burdens for patients. This research aims to quantify the full economic cost of diagnostic delays, highlighting the need for timely identification and management of this incurable form of inflammatory arthritis.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
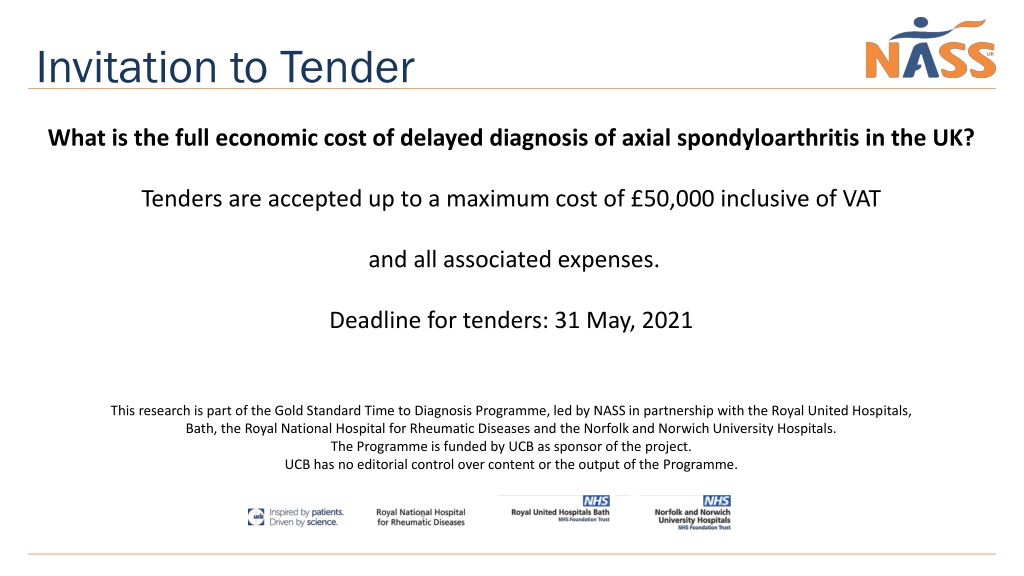
Invitation to Tender What is the full economic cost of delayed diagnosis of axial spondyloarthritis in the UK? Tenders are accepted up to a maximum cost of 50,000 inclusive of VAT and all associated expenses. Deadline for tenders: 31 May, 2021 This research is part of the Gold Standard Time to Diagnosis Programme, led by NASS in partnership with the Royal United Hospitals, Bath, the Royal National Hospital for Rheumatic Diseases and the Norfolk and Norwich University Hospitals. The Programme is funded by UCB as sponsor of the project. UCB has no editorial control over content or the output of the Programme.
Background Axial Spondyloarthritis (axial SpA) is a painful, incurable form of inflammatory arthritis. It mainly affects the spine but can also affect other joints in the body, including the hips, knees, feet, shoulders, elbows and hands. Additionally, it can affect the eyes, gut and skin. People with axial SpA live with daily pain, stiffness and high levels of fatigue. The condition is managed through medication to reduce the inflammation and regular exercise. However, it lasts a lifetime and is characterised by regular flare ups of the disease. An estimated 1 in 200 of the adult population in the UK have axial SpA. About NASS NASS is the oldest patient organisation in the world with a specific focus on supporting people living with axial SpA. For 45 years we ve been providing specialist support, advice and the most up-to-date information. We aim to empower people living with axial SpA not only to manage their condition but to stay in control of their lives. We are driven to ensure that health professionals around the country deliver tailored and timely care to every patient, every time.
Context of the Study In the UK, it takes on average 8 years for someone living with axial SpA to be diagnosed. During this time people can experience significant amounts of pain and anxiety and they often pay a heavy physical and psychological price for this delay (1) . Symptoms typically begin in early adulthood (average age of 24) when people are trying to establish careers, start relationships and families, so a delay to diagnosis can be incredibly disruptive to someone during their formative years. To date, there have been no health economic studies of the impact of diagnostic delay in the UK. The indirect effect of delay (through greater disease severity) has been shown potentially. To date, there have been no health economic studies of the impact of diagnostic delay in the UK. The indirect effect of delay (through greater disease severity) has been shown potentially to double the cost to the NHS (2). An Egyptian study found that patients with longer delay had nearly 3-times higher number of visits to the doctor prior to diagnosis, amounting to a near-4-fold higher expenditure. This was replicated in an Australian study, where a quarter of patients with <5 year delay incurred high treatment costs (>3000 US Dollars), compared to two thirds among those with >10 year delay (4). These trends may well be present in the UK. (1) Martindale J, Goodacre L. The Journey to Diagnosis in AS/Axial SpA: The Impact of Delay: The Journey to Diagnosis in AS/Axial SpA. Musculoskeletal Care. 2014 Dec;12(4):221 31 (2) Cooksey R, Husain MJ, Brophy S, Davies H, Rahman MA, Atkinson MD, et al. (2015). The Cost of Ankylosing Spondylitis in the UK Using Linked Routine and Patient-Reported Survey Data PLoS ONE 10(7): e0126105 (3) Abdelrahman F, Mortada M. Impact of application of ASAS criteria for axial spondyloarthritis on the diagnostic delay in Egyptian patients. Ann Rheum Dis. 2018;77:1556 7 [abstract AB0858] (4) Grigg S, Martin B, Buchanan R, Schachna L, Inman R. 1308 - Burden of Delay to Diagnosis of Ankylosing Spondylitis. ACRARHP Sci Meet 2011 [Internet]. 2011 Nov [cited 2020 Feb 22]; Available from: https://acr.confex.com/acr/2011/ webprogram/Paper22233.html
Context of the Study Whilst there have been some health economic studies of diagnostic delay, these tend Aggregate Cost: 2.1Bn to focus on healthcare costs. There have been fewer studies into the costs of lost 20000 productivity or inappropriate out of pocket costs as a consequence of diagnostic delay. To our knowledge, there haven t been any studies worldwide that have sought 18000 Unpaid Assistance 349M to estimate the total cost of diagnostic delay. There is one study in the UK from 2015 16000 that looked at the total cost of ankylosing spondylitis in the UK which it estimated to 14000 be 19,016 per patient per year (1). 12000 Early Retirement 892M Cost per Time to diagnosis has not improved significantly in the UK (2). In response, NASS is 10000 patient in undertaking an ambitious programme to create the world s first Gold Standard Time 8000 to Diagnosis in axial SpA set at one year and a four-year national implementation 6000 Presenteeism 377M plan. We have recently undertaken a national consultation about our proposal. You Absenteeism 45M 4000 Out of Pocket 126M can read our consultation document here: https://nass.co.uk/wp- Prescription 99M 2000 Inpatient / A&E 79M content/uploads/2020/08/200821-Gold-Standard-Consulation-Document-FINAL.pdf . Outpatient 125M 0 (1) Cooksey R, Husain MJ, Brophy S, Davies H, Rahman MA, Atkinson MD, et al. (2015). The Cost of Ankylosing Spondylitis in the UK Using Linked Routine and Patient-Reported Survey Data PLoS ONE 10(7): e0126105 (2) Delay to Diagnosis in Axial SpA: Are We Improving in the UK? Sykes M, Doll H, Sengupta R, Gaffney K. Rheumatology (Oxford). 2015; 54(12):2283-4
Context of the Study The consultation sets out four reasons for diagnostic delay: Delay 1: People do not know that axial SpA may be a cause of their chronic back pain Delay 2: GPs / primary care professionals may not recognise features of axial SpA Delay 3. People may be referred to non-rheumatologists who may not promptly recognise axial SpA Delay 4. Rheumatology and radiology teams may not optimally request or interpret investigations. NASS has been working to create and use multiple policy, commissioning and practice levers to reduce the time to diagnosis. These include: Our All Party Parliamentary Group on axial SpA (formed in March 2019) and other Parliamentary mechanisms (questions, debates, Ministerial meetings) Our healthcare quality improvement programme Aspiring to Excellence https://nass.co.uk/homepage/health-professionals/aspiring-to-excellence/ Plans to develop a primary care clinical champions programme, and a secondary care services education programme Plans for national awareness raising campaigns.
Scope of the Study The study needs to answer the question: What does each year of delayed diagnosis in axial SpA cost the UK economy? The study should construct a single total figure that encompasses all of the costs of diagnostic delay. We will use this figure in our Parliamentary and campaigning work in order to support our other efforts to drive down the average time to diagnosis. The study assumes that a Gold Standard time to diagnosis (from first symptom onset to diagnosis by a rheumatologist) is one year. Therefore, any time to diagnosis greater than one year should be classed as diagnostic delay. We anticipate that this will be a UK-wide study, although we appreciate that data might not be available in each country for each part of the study. The study is likely to include: Healthcare costs, including healthcare visits, procedures, medications, hospitalisation, co-morbidity Lost productivity Inappropriate out of pocket expenses, including visits to osteopaths and chiropractors, carer costs, travel, purchase of over the counter medications, housing support, transport costs, home adaptations, etc. We anticipate that a modelling study is required whose components are likely to include: Prevalence (and incidence) of axial SpA in the UK Disease progression with and without diagnosis Relationship between disease progression and resource use. The research will build a model to make the best estimate possible with the available evidence, and will express uncertainties in the model. Identifying those uncertainties might also help to frame a future research agenda to reduce the uncertainty in the estimate. Data sources are likely to include registries, audits, research studies, and enriched populations (e.g. uveitis patients).
Prevalence and Incidence The study will need to consider the denominator population of people with axial SpA and the number of people whose diagnosis has been delayed, drawing on the existing literature.Methodologic challenges in conducting epidemiologic studies of axial SpA include screening methods, study design, and classification criteria (1). This latter is particularly important. Whilst historically studies looked only at those patients with radiographic progression (ankylosing spondylitis, or AS), we now consider the broader spectrum of disease of axial Spondyloarthritis which includes those who don t have radiographic change. AS and axial SpA are not equivalent, and reviewers comment on the challenges of interpreting data in the published literature because of this misuse of terminology (2). The prevalence of AS is estimated at 0.01 0.54%, and that for axial SpA is estimated at 0.13 1.4% (3). A recent systematic review of the global prevalence of AS found the mean AS prevalence per 10,000 was 23.8 in Europe (ie. 0.24%), with a weighted mean of 18.6 (4). With the advent of MRI technology to assess for inflammation (rather than just looking for structural damage on X-ray), and the routine availability of the HLA-B27 gene marker, we can more sensitively diagnose a wider spectrum of people with axial SpA. Using these more sensitive diagnostic approaches in patients presenting below the age of 45 with features of inflammatory back pain, axSpA may be seen in up to 1.4% of the population of the United States and in a similar frequency in Europe (5). A UK cross-sectional cohort study reported an axial SpA prevalence of 0.3% using the ASAS criteria and 0.15% using the modified New York criteria (which underscores the earlier point that many of the differences in estimates reflect differences in classification). A study in Scotland reported a prevalence of 0.13%. The Guideline Development Group set up in 2017 to advise NICE on the development of Guideline ng65 concluded that a base case value of 5% was reasonable, though a relatively conservative estimate. There are fewer studies on the incidence of axial SpA, and no published studies that deal with the full spectrum of axial SpA. Incidence is estimated at between 6 and 8 per 100,000. (1) Bohn R, Cooney M, Deodhar A, Curtis J & Golembesky A. Incidence and prevalence of axial spondyloarthritis: methodologic challenges and gaps in the literature. Clin Exp Rheumatol. Mar-Apr 2018;36(2):263-274 (2) Akkoc N, Kahn MA, Epidemiology of axial Spondyloarthritis in Mease P & Khan MA Axial Spondyloarthritis. 2020: Elsevier, Missouri (3) Barnett R, Ingram T, Sengupta R. Axial spondyloarthritis 10 years on: still looking for the lost tribe Rheumatology, Volume 59, Issue Supplement_4, October 2020, Pages iv25 iv37 (4) Dean L, Jones G, MacDonald A, Downhan C, Sturrock R & Macfarlane G. Global prevalence of ankylosing spondylitis Rheumatology (Oxford), 2014 Apr;53(4):650-7 (5) Mease P & Khan MA Introduction in Mease P & Khan MA Axial Spondyloarthritis. 2020: Elsevier, Missouri
Prevalence and Incidence A UK cross-sectional cohort study (1) reported an axial SpA prevalence of 0.3% using the ASAS criteria and 0.15% using the modified New York criteria (which underscores the earlier point that many of the differences in estimates reflect differences in classification). A study in Scotland reported a prevalence of 0.13% (2). The Guideline Development Group set up in 2017 to advise NICE on the development of Guideline ng65 (3) concluded that a base case value of 5% was reasonable, though a relatively conservative estimate (4). There are fewer studies on the incidence of axial SpA, and no published studies that deal with the full spectrum of axial SpA. Incidence is estimated at between 6 and 8 per 100,000. (1) Hamilton L, Macgregor A, Toms A, Warmington V, Pinch E & Gaffney K The prevalence of axial spondyloarthritis in the UK: a cross-sectional cohort study. BMC Musculoskeletal Disorders (2015) 16: 392 (2) Dean L, Macfarlane G & Jones G. Differences in the prevalence of ankylosing spondylitis in primary and secondary care: only one third of patients are managed in rheumatology. Rheumatology 2016: 55: 1820 1825 (3) NICE Guideline (2017) Spondyloarthritis in over 16s: diagnosis and management (4) NICE (2017) Spondyloarthritis. Full heath economic report: https://www.nice.org.uk/guidance/ng65/evidence/appendix-h-full-health-economics-report-pdf-4368823749
Disease progression with & without diagnosis A recent systematic review concluded that patients with delayed diagnosis tend to experience worse outcomes. Longer delay is consistently linked with higher disease activity, worse physical function including spinal mobility, greater damage on X-ray images, poorer quality of life and higher prevalence of depression. Diagnostic delay also comes with significant costs to the individual and society, including higher risk of work disability, unemployment and job loss. To be clear, disease progression is broader than structural damage, and includes functional impairment, employment, etc. At the moment we do not have sufficiently strong data to support an assumption of a year on year disease progression. Whilst there is a growing literature showing that NSAIDs and anti-TNF biologic therapies can delay radiographic progression we still don t know enough about the disease modification effects of treatment. In addition, we can t predict which people will develop severe disease, although we know risk factors for radiographic progressions such as smoking. We don t have longitudinal studies to look at this, although data from a cohort in Germany showed that 20% of those diagnosed had disease progression within two years. There are also data suggesting that there is little disease progression after the age of 55. Economists have dealt with this issue in axial SpA, and in other rheumatological conditions, by modelling a constant rate of disease progression after a defined period. This was the case, for example, in the anti-TNF appraisal (2). The current approach is therefore quite crude. Applicants will need to decide whether to use this approach or attempt some other ways of modelling disease progression. Relationship between disease progression and resource use The study will need to consider how best to model the relationship between disease progression and resource use. One option might be to mirror the kinds of models used in cost-effectiveness studies on drug treatments, which try to simulate the path of the patient in terms of BASFI over time, and link their health status to the costs. Using this approach, it won t matter when someone is diagnosed, or what treatment they were on, as long as we can link someone s health status to their costs and treatment costs. BASFI won t capture co-morbidities, which would also need estimation. (1) Yi E, Ahuja A, Rajput T, George AT, Park Y. Clinical, Economic, and Humanistic Burden Associated With Delayed Diagnosis of Axial Spondyloarthritis: A Systematic Review. Rheumatol Ther. 2020 Mar;7(1):65 87 (2) TNF-alpha inhibitors for ankylosing spondylitis and non-radiographic axial spondyloarthritis. Technology appraisal guidance [TA383] NICE: 2016
A final point about modelling This study may have potential use as a cost effectiveness approach for different technologies in axial SpA. If the model that is built is agreed upon by the clinical community, it may provide a reference case model for future cost effectiveness studies. Applicants will no doubt want to consider their engagement of the clinical community with this in mind. Phasing and Deliverables Given the potential complexities in trying to create a model and use multiple data sources, we propose that the study takes place in two phases, both of which are covered by this Invitation to Tender and funding amount. The first phase should assess the feasibility of the study as expressed - including the proposed modelling approach and the data to populate it - and make any recommendations for modification for consideration by NASS in an interim report. We will then take a decision on whether the study can move to the second phase and in what form. The provider will then complete the study and submit to NASS a final report along with an accompanying slide deck, that answers that core study questions.
For an informal discussion about the proposal, please contact NASS CEO Dr. Dale Webb dalewebb@nass.co.uk Please submit your tender using the Tender Response Form to lisaswingler@nass.co.uk Details on the Tender terms and Conditions can be found here Tenders are accepted up to a maximum cost of 50,000 inclusive of VAT and all associated expenses. Please note that NASS does not pay organisational overheads.