Prevention of Surgical Site Infections: Key Factors and Recommendations
Surgical site infections (SSIs) are a significant concern in healthcare settings, with 25% of healthcare-associated infections being SSIs. They are preventable, but still pose challenges due to multifactorial causes. Risk factors include uncontrolled diabetes, obesity, smoking, and length of preoperative stay. Prevention strategies include maintaining a sterile environment, proper surgical scrub protocols, antimicrobial prophylaxis, and addressing operative risk factors like contamination and hypothermia.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
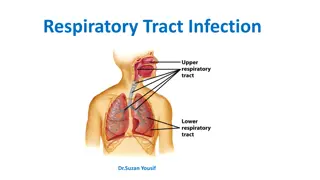
Prevention of Surgical Site Infections (SSI)
Learning objectives December 1, 2013 1. Explain the relevance and impact of SSI. 2. Identify the risk factors associated with SSI. 3. Describe the main recommendations to prevent SSI. 2
Time involved December 1, 2013 35-40 minutes 3
Background -1 December 1, 2013 One of the most important healthcare associated infections 25% of all HAIs 40% to 60% preventable High cost prolong hospital stay increase antimicrobial and laboratory costs require added health care interventions 4
Background -2 December 1, 2013 Sterilisation, aseptic technique, clean air, and prophylaxis have reduced SSI The numbers are still high Important cause of morbidity and mortality Multi-factorial Difficult to determine the exact cause Higher in developing nations 5
Factors that influence transmission of infection December 1, 2013 Patient risk factors Types of surgical procedures Operating room environment 6
Patient risk factors December 1, 2013 Proven Uncontrolled Diabetes Obesity especially in orthopaedic and cardiac Controversial Nutrition status Smoking Coexisting remote infection Colonisation with microorganisms Length of preoperative stay Perioperative transfusion 7
Operative Risk Factors - 1 December 1, 2013 Colonisation of the operative site Antiseptic bath Skin antisepsis (consider clorhexidine) Colonisation of the surgical team Surgical scrub with antiseptic No artificial nails Preoperative shaving Infected or colonised surgical personnel 8
Operative risk factors - 2 December 1, 2013 Duration of operation Contamination of the operative site Antimicrobial prophylaxis Foreign material in the surgical site sutures and drains Hypothermia Surgical technique 9
Environmental risk factors December 1, 2013 Operating room ventilation Number of people in OR Inanimate surfaces Inadequate sterilisation Surgical clothes, gloves and masks 10
Ventilation system December 1, 2013 11
Surveillance Shown to reduce SSI risk Post-discharge surveillance essential Should include Standard definitions Risk stratification Typical definition Purulent drainage from the incision site or from the site of a drain with either a positive or negative culture December 1, 2013 12
Risk stratification Based on a specific surgery Cholecystectomy, hernia repair, Caesarean section, hip replacement Specific risk of patients Type of surgery Clean, clean-contaminated, contaminated, or dirty Compare the clean wound SSI rates among different surgeons Patient index Standardised infection ratios December 1, 2013 13
Basic Recommendations for Prevention Preoperative - 1 December 1, 2013 Identify and treat all infections Good control of diabetes Minimum hospital stay Do not remove hair preoperatively If essential, use a non-invasive procedure, e.g., clipper Skin preparation with antiseptic 14
Basic Recommendations for Prevention Preoperative - 2 Surgical scrub with antiseptic (can be water- less); nail cleaner No brushes Exclude personnel with infections Prophylactic antibiotics Determine the level of experience required for surgeons in complex surgeries December 1, 2013 15
Surgical hand scrub/hand rub December 1, 2013 16
Basic Recommendations for Prevention Intraoperative - 1 December 1, 2013 Surgical checklist Limit the duration of the procedure Validate Sterilisation No flash sterilisation routinely Sterile gloves Water-repellent gowns and drapes, mask, cap Positive pressure ventilation (20 changes per hour) Filter air Doors closed 17
Basic Recommendations for Prevention Intraoperative - 2 Restrict entrance and movements Asepsis in interventions and invasive procedures Handle of tissue gently Drains only if is necessary Remove as soon as possible Normothermia Temperature between 36.5 and 37 C Normoglycaemia <200 mg/dL December 1, 2013 18
Basic Recommendations for Prevention Intraoperative - 3 Avoid artificial nails among surgical team Screening and decolonisation of carriers of S. aureus in high-risk patients No special procedures after contaminated or dirty operations No over-shoes and tacky mats December 1, 2013 19
Basic Recommendations for Prevention - Postoperative December 1, 2013 Don t touch the wound unless necessary Review daily the necessity of continuing drains and take out when no necessary Surveillance system for SSI with risk classifications Post-discharge surveillance for ambulatory surgery or short hospital stay 20
Minimal requirements for the prevention of SSIs Do not remove hair unless necessary Glycaemia control in cardiac and vascular surgery Antiseptic for skin preparation Surgical scrub with antiseptic Prophylactic antimicrobial Validate sterilisation Asepsis in interventions or invasive procedures Surveillance with standard definitions and risk classification December 1, 2013 21
Summary December 1, 2013 SSI development is multifactorial There are strategies like surgical techniques, skin preparation, and the timing and method of wound closure that influence it Antibiotic prophylaxis may have a positive impact in certain types of surgery 22
References December 1, 2013 Galway UA, Parker BM, Borkowski RG. Prevention of Postoperative Surgical Site Infections. International Anes Clinics 2009; 47(4): 37 53. Mangram, AJ, et al. Guideline for Prevention of Surgical Site Infection, 1999. The Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999; 20:250-278. Hranjec T, Swenson BR, Sawyer RG. Surgical site infection prevention: how we do it. (Report). Surg Infections 2010; 11 (3): 289-294. 23
References Ercole FF, et al. Applicability of the national nosocomial infections surveillance system risk index for the prediction of surgical site infections: a review. Braz J Infect Dis 2007;11(1):134-41. Edwards JR, Horan TC. Risk-Adjusted Comparisons. IN: APIC Text of Infection Control and Epidemiology. 3rd ed. Association for Professionalsin Infection Control and Epidemiology, Inc. Washington, DC. 2009: 7-1 to 7-7. Haynes AB, et al. A Surgical Safety Checklist to Reduce Morbidity and Mortality in a Global Population. N Engl J Med 2009; 360 (5): 91 99. Checklist at http://whqlibdoc.who.int/ publications/2009/9789241598590_eng_Checklist.pdf December 1, 2013 24
Further reading Potenza B, et al. Lessons learned from the institution of the Surgical Care Improvement Project at a teaching medical center. Am J Surg 2009; 198(6):881-8. Awad SS, et al. Implementation of a methicillin-resistant Staphylococcus aureus (MRSA) prevention bundle results in decreased MRSA surgical site infections. Am J Surg 2009; 198(5):607-10. Tom TS, Kruse MW, Reichman RT. Update: Methicillin-resistant Staphylococcus aureus screening and decolonization in cardiac surgery. Ann Thorac Surg 2009; 88(2):695-702. Akins PT, et al. Perioperative management of neurosurgical patients with methicillin resistant Staphylococcus aureus. J Neurosurg 2010; 112(2):354-61. December 1, 2013 25
Web sites CDC/NHSN Surveillance Definition of Healthcare-Associated Infection and Criteria for Specific Types of Infections in the Acute Care Setting US. http://www.cdc.gov/nhsn/PDFs/pscManual/17pscNosInfDef_curren t.pdf Institute for Healthcare Improvement (US). http://www.ihi.org/IHI/Topics/PatientSafety/SurgicalSiteInfections/ National Nosocomial Infection Program. Ministry of Health Chile. www.minsal.cl Surgical Site Infections National Healthcare Safety Network, US. http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf Surgical Site Infection Surveillance Service (UK). http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Surg icalSiteInfectionSurveillanceService/ WHO - Safe Surgery Saves Lives. http://www.who.int/patientsafety/safesurgery/en/index.html December 1, 2013 26
Quiz 1. A key in a surveillance system for SSI is to have risk stratification of the patients included. T/F? Which of the following is a risk factor for SSI? a) Controlled diabetes b) Type of suture c) Breaks in the aseptic technique during surgery d) Design of the operating room table Which statement regarding antimicrobial prophylaxis is correct? a) In all cases one dose is enough b) Has shown reduction in SSI in selected surgeries c) Must be used for more than 48 hrs. after the surgery d) All the available drugs are the same December 1, 2013 2. 3. 27
International Federation of Infection Control IFIC s mission is to facilitate international networking in order to improve the prevention and control of healthcare associated infections worldwide. It is an umbrella organisation of societies and associations of healthcare professionals in infection control and related fields across the globe . The goal of IFIC is to minimise the risk of infection within healthcare settings through development of a network of infection control organisations for communication, consensus building, education and sharing expertise. For more information go to http://theific.org/ December 1, 2013 28