Ensuring Long-Term Equitable Access to Telehealth in New York State
The report explores telehealth utilization trends, policy landscapes, and challenges in New York State post-COVID-19. Key findings include variations in telehealth usage based on demographic factors and the impact of the Public Health Emergency on telehealth services. Recommendations are made to expand access and improve equity in telehealth services in the state.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
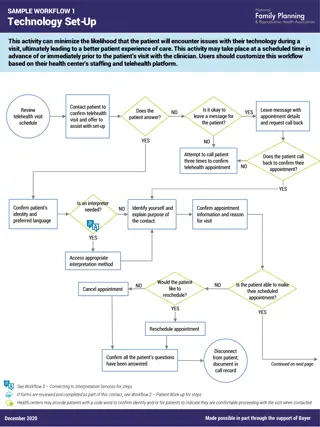
NYHF Report Development 1 Key Identifying Best Practices in Other States Landscape Assessment Report Stakeholder Interviews Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
NYHF Report Contents 2 Executive Summary Background Utilization Trends Pre- and Post COVID-19 Public Health Emergency (PHE) National and New York State (NYS) Policy Landscape Key Policy Recommendations to Expand Equitable Access to Telehealth in NYS Innovative Telehealth Programs Across NYS Conclusion and Appendices Telehealth Definitions Current Regulations Establishing Telehealth Coverage and Reimbursement in NYS Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
3 National Telehealth Policy Landscape Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
All-Payor Utilization Peaked in 2020 and Plateaued Above Pre-PHE Levels; Behavioral Health Now Accounts for More than Half of Telehealth Claims 4 All-Payor Telehealth Utilization: Behavioral Health vs. All Other Services 2019-2022 All-Payor Telehealth Visit Volumes 2019-2023 Sources: Trilliant Health; Trilliant Health. Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Telehealth Utilization Trends Varied by Demographic Factors Across Payors 5 Patients who were older, Black or Asian and did not speak English as a primary language at home were less likely to use telehealth. Telehealth use was also lower among individuals living in rural areas. Hispanic/Latino, Black, and Asian individuals utilized video visits at a lower rate relative to White individuals; conversely, these groups utilized audio-only visits at a higher rate. Similar trends were seen in NYS all payor telehealth utilization data. Sources: Assistant Secretary for Planning and Evaluation, Updated National Survey Trends in Telehealth Utilization and Modality (2021-2022) (April 2023); Datta et al, Telemedicine and Health Access Inequalities During the COVID-19 Pandemic (December 2022). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
The PHE Changed the Broader Telehealth Landscape 6 Changes brought on by the PHE have accelerated the implementation, adoption, and widespread use of telehealth services across the healthcare industry, leading to: Significant federal and state-level policy changes, including changes to telehealth reimbursement rates, expansion of covered modalities and services, allowing patients to receive care from any location, cross- state licensure flexibilities, among others. Significant changes in how providers practice and deliver care, with many providers operating a hybrid care model where they offer both in-person and telehealth visits. New challenges, including determining which services can be appropriately delivered via video vs. audio- only modalities, developing policies related to the establishment of provider/patient relationships via telehealth, addressing digital equity issues, and more. New opportunities to make permanent PHE flexibilities that meaningfully expanded access to care permanent, such as coverage parity, equitable payment, cross-state licensure allowances, among others. Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Key Telehealth Policy Changes: Federal 7 Among the many flexibilities enacted at the federal level, several notable examples include: Centers for Medicare and Medicaid Services (CMS) Medicare. Significantly expanded coverage and reimbursement for a wide range of telehealth services, provider types, and modalities (including audio-only). Enabled beneficiaries in both rural and urban areas to receive telehealth services in their homes. Health and Human Services Office of Civil Rights. Issued notice of enforcement discretion of Health Insurance Portability and Accountability Act (HIPAA), which created flexibility for good faith provision of telehealth services using non-public technologies that are not HIPAA compliant. U.S. Drug Enforcement Administration. Provided flexibility to prescribe buprenorphine via telehealth without an initial in-person appointment. Substance Abuse and Mental Health Services Administration (SAMHSA). Provided flexibility for Opioid Treatment Programs using telehealth for substance use disorder treatment (subject to certain requirements) and provided flexibility on 42 CFR Part 2 related to disclosure of patient-identifying information during a bona fide medical emergency. Sources: Bipartisan Policy Center, The Future of Telehealth After COVID-19 (October 2022). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Key Telehealth Policy Changes: States 8 Similarly, states enacted a number of significant telehealth policy changes, including but not limited to: Licensure. All states created licensure flexibility for out of state providers to practice in-state (though many states have since rolled back these flexibilities). Co-Pay Waivers. Many states required commercial insurers to waive co-pays for telehealth services delivered during the PHE. Payment Parity. Several states passed payment parity laws requiring payment for telehealth services at parity with in-person services. Audio-Only. Several states amended their telehealth statutes to include audio-only in the definition of telehealth. Medicaid Telehealth Coverage. All states expanded coverage of telehealth services within their Medicaid programs (to varying degrees). o Policy expansions included: payment parity, audio-only coverage, home as an eligible originating site, new eligible services and providers, among others. Sources: Manatt Analysis of State Telehealth Policy (July 2024 Publication Available here). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Medicaid Telehealth Policy Trends 9 Medicaid Telehealth Eligible Services and Providers, By Number of States 2019-2022 Medicaid Telehealth Eligible Modalities, By Number of States 2019-2022 Sources: ASPE, State Medicaid Telehealth Policies Before and During the COVID-19 Public Health Emergency: 2022 Update (November 2022). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
10 Key Policy Recommendations to Expand Equitable Access to Telehealth in NYS Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Policy Recommendation: Implement Payment Parity Across All Payors for Video Visits. 11 Coverage and payment parity ensure equal coverage and reimbursement for services delivered in-person and virtually, thereby providing the foundation for patients access to telehealth. Given continued demand for telehealth as an option for patients and providers alike, sustainable reimbursement is important. Without ongoing certainty regarding the long-term future of payment parity, providers will be reluctant to continue investing in maintaining their telehealth offerings, limiting patients access to virtual care and stifling innovation that could improve patient experience and clinical outcomes. Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Coverage And Payment Parity Landscape 12 States with Laws Requiring Insurers to Implement Telehealth Payment Parity for Video Visits July 2024 # of States with Payment Parity 29 Permanent Parity 22 Parity with Caveats 7, including NYS Sources: Manatt Health, Telehealth Policy Tracker: Tracking Ongoing Federal and State Telehealth Policy Changes (July 2024). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Policy Recommendation: Implement Payment Parity for Audio-only Visits Across all Payors, Adopting Medicaid-specific Requirements. 13 Another major lesson learned during the PHE was that audio-only visits are an important pathway to care for patients who do not have access to home internet, digital devices, or data plans to support video visits. All payor telehealth utilization data indicate there are disparities in access to video visits by race and ethnicity. Provider practices in communities with high social vulnerability were almost twice as likely as providers in communities with low social vulnerability to use telephones as their primary telehealth modality. Sources: ASPE, Updated National Survey Trends in Telehealth Utilization and Modality (2021-2022) (April 2023); Chang et al. Rapid Transition to Telehealth and the Digital Divide: Implications for Primary Care Access and Equity in a Post-COVID Era (June 2021). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Audio-Only Telehealth Policy Trends 14 PRE-COVID-19 PHE COVID-19 PHE CURRENT STATE Medicare is temporarily allowing coverage for certain audio- only services through December 31, 2024. Forty-three states/District of Columbia reimburse for audio- only telephone in some capacity in their Medicaid program. Many of these states have narrowed their audio-only coverage and payment policies by imposing limitations (e.g., by service type, geography, existing relationship with provider). For example: Audio-only was not a commonly recognized or covered form of telehealth. Very few state Medicaid programs covered audio- only. Medicare offered limited coverage for a narrow set of virtual check-in services. State insurance laws carved audio-only out of the definition of telehealth. Significant increase in temporary coverage and reimbursement. o Washington state requires patients receiving audio-only to have had a previous in-person or video visit with the provider in the previous three years. o Hawaii reimburses audio-only telehealth at 80% of comparable in-person rates. Sources: AMA/Manatt, State Telehealth Policy Trends: 2023 Year in Review (November 2023); RAND, State Medicaid Telehealth Coverage Policy Decisions Since the COVID-19 Public Health Emergency (May 2023). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
NYS Medicaid Audio-Only Policy 15 NYS current Medicaid policy is more expansive than many states to give providers decision-making autonomy, but it includes guardrails. Audio-only visits are covered when all the following conditions are met: Video visits are not available to the patient due to lack of patient equipment or connectivity, or audio-only is the preference of the patient; The provider must make either video visit or in-person appointments available at the request of the patient; The service can be effectively delivered without a visual or in-person component, unless otherwise stated in guidance issued by the NYS Department of Health (this is a clinical decision made by the provider); and The service provided via audio-only visits contains all elements of the billable procedures or rate codes and meets all documentation requirements as if provided in-person or via an audio-visual visit. Sources: NYS Medicaid Telehealth Guidance (May 2024). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Policy Recommendation: Reimburse Article 28 Health Centers at the Full Payment Rate for Video/Audio-only Visits When Both Provider and Patient are Located Offsite. 16 Under the Prospective Payment System (PPS), federally qualified health centers (FQHCs) are paid a predetermined rate that encompasses reimbursement for all services provided during a single visit, which is adjusted annually for inflation. Type of FQHC Either the Provider OR Member are On-Site Both the Provider AND the Member are Off-Site Examples with 2023 Rates: Downstate 121st Street Family Health Center PPS Rate: $234.41 Offsite Rate: $77.50 FQHC Operated Article 28 that has not opted into Ambulatory Patient Groups (APGs) Bill Off-Site Rate (rate code: 4012). APGs are NY s outpatient payment system, which groups similar procedures based on patient clinical characteristics and expected resources. Bill PPS Rate (rate code: 4013). Upstate Community Health Center of Buffalo PPS Rate: $144.03 Offsite Rate: $69.23 Bill the Professional Component only. FQHC Operated Article 28 that has opted into APGs Bill APG claim. FQHC Operated Article 31 (Office of Mental Health) or Article 32 (Office of Addiction Services and Supports ) that has not opted into APGs Bill Article 31 or Article 32 rate coded claim for PPS rate. Sources: NYS Medicaid Telehealth Guidance (May 2024). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
Policy Recommendation: Adopt a NYS-specific Approach to Cross-State Licensure such as Licensure Compacts, Special Licensure Pathway, or Exceptions. 17 Telehealth holds potential not just to expand patient access to care, but also to extend the reach of providers contending with workforce shortages and strains. NYS, like many states, adopted temporary licensure flexibilities during the PHE to allow physicians and other health professionals to practice across state lines and deliver telehealth to NYS residents without having to apply for a license. These flexibilities have expired, but many states have since recognized the benefits of cross-state licensure flexibilities in addressing workforce shortages and enabling continuity of care for established patients while clinicians are traveling. Sources: US Federation of State Medical Boards, U.S. States and Territories Modifying Requirements for Telehealth in Response to COVID-19 (May 2023). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges
State Approaches to Telehealth Licensure 18 Exceptions to In-State Licensure Special Purpose Telehealth Registry Interstate Compacts Idaho Florida Allowsa provider that is licensed in another state but not licensed in Idaho to provide telehealth services when the provider: 1. Has established a patient-provider relationship for a patient that 1. Is in Idaho temporarily, or 2. Requires short-term following up services for continuity of care; 2. Provides emergency care in time of disaster, and follow up services to ensure continuity of care; 3. Is employed by or contracted with an Idaho facility or hospital for which the provider has been credentialed; or, 4. Consults with or refers a patient to an Idaho-licensed provider. Offers out-of-state registration for physicians and other health professionals licensed outside of Florida. Registrants cannot have an in-state physical address or provide in-person services in-state. Registrants must maintain liability coverage for telehealth services provided in-state. As of July 2024, 39 states/District of Columbia participate in the Interstate Medical Licensure Compact (IMLC) and 41 participate in the Nurse Licensure Compact (NLC). Each of these compacts varies in the licensure flexibilities it provides. NYS has not yet adopted any of these strategies. Sources: AMA/Manatt, State Telehealth Policy Trends: 2023 Year in Review (November 2023). Ensuring Long-Term Equitable Access to Telehealth in New York State, Opportunities and Challenges