Medication Management Continuity: Improving Patient Safety in Hospitals
The issue of continuity in medication management can lead to errors and harm in healthcare settings. Incomplete medication histories at admission contribute to prescribing errors, with omissions of regular medications being a common mistake. Quality improvement initiatives and diagnostics, such as Ishikawa diagrams, are essential in addressing these challenges and creating a more reliable system. Local examples highlight the consequences of medication errors, emphasizing the importance of effective medication reconciliation processes.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Continuity of Medication Management Spreading Medication Reconciliation Improvements Hospital Presenter Month YYYY
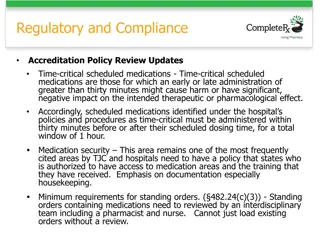
Continuity is an Issue in Health Care 10-67% of medication histories contain at least one error1 Incomplete medication histories at the time of admission have been cited as the cause of at least 27% of prescribing errors in hospital2 The most common error is the omission of a regularly used medicine3 Around half of the medication errors that happen in hospital occur on admission or discharge4 30% of these errors have the potential to cause harm3,5
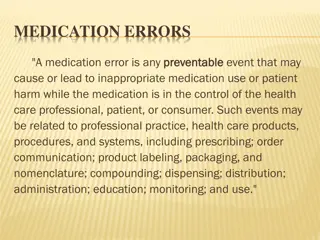
Local Examples - Medication Errors <Insert consequence e.g. contributed to death> <Insert resulting effect on patient> <Insert summarised case notes> <Insert consequence e.g. caused moderate to severe harm> <Insert resulting effect on patient> <Insert summarised case notes> <Insert consequence e.g. caused minor harm> <Insert resulting effect on patient> <Insert summarised case notes>
Quality Improvement <Insert name of ward/unit> <Insert names of Quality Improvement team members> <Insert Aim Statement> Specific, Measurable, Aspirational, Realistic, Time based
Diagnosis of Problem <Insert process undertaken e.g. - Process flow chart - Brainstorming - Ishikawa (cause and effect) diagram - Prioritising causes - Weighted voting - Pareto chart>
Problem Work Flow <Insert copy of flow chart>
Ishikawa (Cause and Effect) Diagram Insert group name Insert group name Insert group name Insert cause Insert cause Insert cause Insert cause Insert cause Insert cause Insert cause Insert cause Insert cause Insert cause Insert effect Insert cause Insert cause Insert cause Insert cause Insert cause Insert cause Insert cause Insert cause Insert group name Insert group name
Prioritising Causes <Insert copy of Pareto chart>
Highest Scoring Causes <Insert a description of each of the highest scoring causes on the Pareto chart>
Agreed Strategies <Insert agreed strategies and work plan>
Improvements <Insert improvement results e.g. run charts>
Lessons Learned <Insert what worked well, and what didn t work well>
Strategies for Sustaining Improvements <Insert strategies e.g. - Real time measuring and reporting - Continual training of new staff - Ingraining as standard process - Documentation of procedure, protocols and guidelines - Encourage feedback - Continually review and refine using feedback>
Strategies for Spread <Insert strategies e.g. - Form unit/ward quality improvement team - Compare existing process to trial teams experience - Are there any differences requiring consideration? - Review previous teams results - Are causes similar? - Trial existing or adapted strategies - Measure improvements and refine if required - Communicate to next unit/ward> - Are strategies achievable?
Further Information Clinical Excellence Commission (CEC) Enhancing Project Spread and Sustainability A Companion to the Easy Guide to Clinical Practice Improvement www.cec.health.nsw.gov.au/programs/clinical- practice
References 1. Tam V, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ 2005;173:510-5. 2. Dobrzanski S, Hammond I, Khan G, Holdsworth H. The nature of hospital prescribing errors. Br J Clin Govern 2002;7:187-93. 3. Cornish PL, Knowles SR, Marchesano R, Tam V, Shadowitz S, Juurlink DN, Etchells EE. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med 2005;165:424-9. 4. Sullivan C, Gleason KM, Rooney D, Groszek JM, Barnard C. Medication reconciliation in the acute care setting: opportunity and challenge for nursing. J Nurs Care Qual 2005;20:95-8. 5. Vira T, Colquhoun M, Etchells EE. Reconcilable differences: correcting medication errors at hospital admission and discharge. Qual Saf Health Care 2006;15:122-6.