Effective Communication Skills for Healthcare Professionals
This training focuses on improving communication skills for nurses, social workers, psychologists, and chaplains involved in goals of care conversations. It covers key aspects such as respect, documentation of patients' values, proactive conversations, and the distinction between advance directives and LST orders. Real-life scenarios, like Frederick's case, highlight the importance of clear communication and understanding patients' preferences for end-of-life care.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
GOALS OF CARE CONVERSATIONS TRAINING For Nurses, Social Workers, Psychologists & Chaplains Part 1: Key Communication Skills
Welcome Introductions Agenda Brief review of class materials Ground Rules Respect for privacy Respect for individual values Expectations
VA Life Sustaining Treatment (LST) Decisions Initiative National quality improvement project To improve personalized, proactive, patient- driven care for patients with serious illness by eliciting, documenting, and honoring their values, goals, and preferences Life-Sustaining Treatment Decisions Initiative
The LST Decisions Initiative promotes Proactive goals of care conversations with patients who have a serious illness Improved documentation of the patient s goals of care and LST decisions New progress notes to document goals of care conversations New LST order set to document patients decisions to limit LST
Frederick 85 y.o. male admitted with congestive heart failure Advance Directive reviewed in hospital, states No life sustaining treatments, ever Frederick was discharged Frederick collapsed at home, EMS responded, CPR initiated Transferred to ICU and intubated After 4 days of no improvement, health care surrogate made decision to withdraw LSTs, Frederick died
Different than Advance Directives Advance Directives LST Orders Document reflecting the patient s preferences for future treatment after loss of decision-making capacity Medical orders for current treatment Based on a goals of care conversation with a patient or the surrogate Not orders - guides health care decisions made by the surrogate after the patient can no longer speak for themselves
Different than Advance Directives CONTINUED Advance Directives LST Orders Completed by patients Completed by practitioners Used to appoint a health care agent
LST Decisions Initiative Tested in four VA sites Lovell Federal Health Care Center, VA Black Hills, VA Salt Lake City, and William S. Middleton Memorial VA Hospital in Madison To be fully implemented in all VA health care systems by July 2018
The Life-Sustaining Treatment Decisions Initiative Video
LST Decisions Initiative New policy (VHA Handbook 1004.03) New progress notes and orders Goals of Care Conversations Training For Physicians, Nurse Practitioners, and Physician Assistants For Nurses, Social Workers, Psychologists, and Chaplains This program!
When you finish this program, you will be able to: Conduct a goals of care conversation using key communication skills and a talking map Identify new process for documenting goals of care conversations Carry out a plan with your team to conduct goals of care conversations with high-risk patients
Part 1: What We Will Learn Nature and purpose of goals of care conversations Key communication skills to be used throughout a goals of care conversation
Part 1: How We Will Learn Presentation Examples Practice
What is a Goals of Care Conversation? Discussion to elicit the Veteran s values, goals, and preferences that serve as a basis for decisions about services and medical care, including LSTs
A Shift in Culture Earlier in the course of illness During a health crisis What do you hope for with your medical care? Do you want us to do everything for you? Proactive, patient-driven care!
Why are proactive goals of care conversations important?
When should goals of care conversations happen? When a patient is at high risk of a life-threatening clinical event in the next 1-2 years In any clinical setting; before a health crisis is best May take more than one conversation, involve more than one clinician When any patient wants to discuss or limit LST Ongoing conversation through the disease process
Roles and Responsibilities RNs/SWs/Ps/Cs/ MDs/APRNs/PAs MDs/APRNs/PAs ONLY Introduce the goals of care conversations Discuss role of the surrogate Elicit understanding of diagnosis and prognosis Deliver news about diagnosis and prognosis Elicit patient s values, goals Provide basic information about LSTs & services Document the conversation Establish a LST plan with patient (or surrogate) Complete LST Progress Note and Orders
Whats challenging when talking to patients or families about serious illness and care near the end of life?
Your Approach Matters Build a partnership with the patient by Creating an open, safe environment Believing in the patient s ability to make difficult decisions Allowing the patient to discover their own understanding
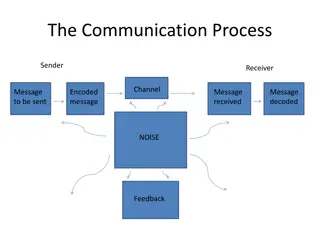
Communication Skills Many Purposes Everyday conversations with family, co-workers, patients, others Strong skills required for challenging situations (high emotion, resistance, ambivalence) Can be taught Require practice!
Expect Emotion Occurs frequently in goals of care conversations - loss, end of life and death are difficult subjects High emotion can impair: Communication process Elicits fight or flight response Cannot hear the information Reasoning and decision making
Recognizing Emotion Manifests differently in different people Not usually tears! Patient cues Shutting down/quiet Body language Intonation changes Ambivalence/resistance Questions - especially why
Recognizing Ambivalence Ambivalence: having two conflicting desires I don t like coming to the hospital, but it makes my breathing better. Coming to appointments is difficult. But I don t like the idea of people coming into my home.
Recognizing Resistance Resistance occurs when we expect or push conversation content when the patient isn t ready I already wrote everything down 20 years ago in my advance directive. I don t see why I need to talk about this right now.
Key Communication Skills Open-ended questions Reflective listening Exploring Affirmations I wish statements
Open-Ended Questions Elicit the patient s own knowledge, language, understanding and/or feelings Elicit details rather than one word answers How has your health affected your day to day life? You mentioned you have heart failure; what is your understanding of that disease?
Open-Ended Questions Practice CLINICIAN: Do you understand the role of a health care surrogate? CLINICIAN: What is your understanding of the role of a health care surrogate?
Simple Reflections Repeating or paraphrasing patient s statements Encourage continuation Confirm understanding Reinforce concepts or knowledge PATIENT: My breathing is bad I can t walk as far as I used to, and I have to wear oxygen all the time now. SIMPLE REFLECTION: Your breathing has really been giving you a hard time.
Simple Reflections Practice PATIENT: My mom was resuscitated and ended up on machines. I couldn t stand seeing her like that. CLINICIAN: You have seen someone close to you need machines to stay alive.
Complex Reflections Interpret patient s statements Validate feelings Explore deeper meaning PATIENT: I don t want to come to the hospital any more, but it makes my breathing feel a lot better. COMPLEX REFLECTION: You re feeling conflicted.
Complex Reflections Practice PATIENT: My doctors keep telling me there is no way to know if my cancer treatments are working. They won t know anything until my next scan. Why do we have to wait so long? CLINICIAN: It sounds like it s really hard to live with the uncertainty.
Affirmations Recognize strengths & acknowledge positive behavior Build rapport & patient s confidence You re saying this is difficult to talk about, and yet you came to today s appointment anyway. You have shown so much support for your dad.
Affirmations Practice PATIENT: I m a fighter, I know I can beat this thing. CLINICIAN: You ve been so strong through so much.
Exploring Seeks more information Clarifies meaning Builds deeper understanding Tell me more What else? What do you mean when you say life support ?
Exploring Practice PATIENT: I ve always told my kids don t keep me alive if I m a vegetable. CLINICIAN: Tell me what you mean when you say vegetable .
I wish Statements Recognize patient s hope Align with the patient I wish we had more effective treatments. I hope for a miracle, too.
I wish Statements Practice PATIENT: My breathing has gotten so bad. Why can t they find a way to get rid of my COPD? CLINICIAN: I wish you didn t have to deal with these lung problems.
Questions Can Signal Emotion Watch for questions that are actually expressions of emotion: Isn t there something else they can do for the cancer? Why is this happening to me? Respond to the EMOTION with EMPATHY rather than responding to the QUESTION with FACTS It must be so hard to be going through this.
Responding to Emotion Practice
Responding to Emotion Practice PATIENT: What do you mean CPR doesn t always work? CLINICIAN: This information seems really surprising.
Responding to Emotion Practice PATIENT: I just don t know how I m going to talk to my kids about this. I want to talk to them so they know what to do, but they ll be so upset CLINICIAN: You re worried about upsetting your kids, and at the same time you know it s important to talk to them about this.
Responding to Emotion Practice PATIENT: My doctor says the cancer is in my lung and liver. Why can t they just cut the cancer out? CLINICIAN: I wish we could remove it, too.
Practice Exercise We re going to practice using communication skills and inviting a patient to participate in a goals of care conversation
Practice Instructions Take out Offering a Goals of Care Conversation communication skills exercise Divide into pairs Decide who will be the clinician and who will be the patient Debrief with one another: How did it feel to say the words? One thing clinician noticed One thing patient noticed Switch roles and repeat See Handout
Large Group Debriefing What s one thing you noticed as the clinician? What s one thing you noticed as the patient?
For Your Reference Communication Skills Guide FRONT: examples of each communication skill BACK: sample responses to difficult statements made by patients and families See Handout
What surprised you? What do you want to take forward? Anywhere you might get stuck?
Summary Goals of care conversations are important to proactively elicit the patient s values, goals, and preferences, which serve as the basis for treatment decisions Use key communication skills throughout the goals of care conversation Recognize and respond to emotion
Goals of Care Conversations Goals of Care Conversations training materials were developed and made available for public use through U.S. Department of Veterans Affairs. Materials are available for download from VA National Center for Ethics in Health Care at www.ethics.va.gov/goalsofcaretraining.asp.