Understanding Cryptococcal Immune Reconstitution Inflammatory Syndrome
Cryptococcal Immune Reconstitution Inflammatory Syndrome (C-IRIS) is a condition where rapid reversal of immunodeficiency triggers exaggerated inflammatory reactions in response to Cryptococcus antigens. It can manifest as either Unmasking IRIS or Paradoxical IRIS, with common CNS presentations including headache, meningism, and seizures. Diagnostic criteria involve new or worsening clinical, radiographic, or histopathological manifestations during antifungal therapy. Predictors include high fungal burden and host immune factors. Management and prevention strategies are crucial to reduce mortality rates associated with C-IRIS.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Cryptococcal Immune Reconstitution Inflammatory Syndrome Dr. Tihana Bicanic Reader and Consultant in Infectious Diseases Centre for Global Health, Institute of Infection and Immunity, St. George s, University of London; St George's Hospital NHS Foundation Trust
Intended Learning Outcomes To understand what immune reconstitution inflammatory syndrome is To be aware of the predictors for C-IRIS To be aware of the different manifestations of C-IRIS To understand the management and prevention of C-IRIS
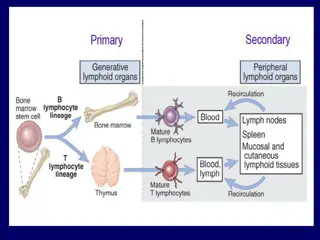
Immune Reconstitution Inflammatory Syndrome Rapid reversal of immunodeficiency leads to restoration of T-cell mediated Cryptococcus- specific immune responses, promoting an (exaggerated) inflammatory reaction to antigens (dead or alive) Two clinical scenarios: 1. Unmasking IRIS: NEW presentation of subclinical/ latent OI 2. Paradoxical IRIS: symptom recurrence in previously treated OI (clinical/ microbiologic response) Incidence: Paradoxical: 6-45% in HIV+ (usually 1-2 months post start of ART), 5-11% solid organ transplant recipients) Acute mortality 0-36%: lower if recognised early and managed appropriately Haddow et al. Lancet Infect Dis 2010; 10:791-802 Longley et al. Curr Opin Infect Dis. 2013;26(1) : 26 34
Immune Reconstitution Inflammatory Syndrome CNS presentation most common: headache, meningism, seizures Lumbar Puncture: CSF WBC, protein, glucose; fungal cultures sterile (paradoxical) or positive (unmasking) Non CNS Pneumonitis Lymphadenitis (including mediastinal) Rarely: skin, soft tissue, bone and joint lesions
Immune Reconstitution Inflammatory Syndrome Diagnostic criteria New appearance or worsening of the following: I. Clinical or radiographic manifestations consistent with an inflammatory process II. Histopathology showing granulomatous lesions III. Symptoms occurring during receipt of appropriate antifungal therapy with no alternative cause identified on investigation IV. Negative results of cultures, or stable or reduced biomarkers for the initial fungal pathogen during the diagnostic workup for the inflammatory process (Unmasking= NEW presentation with cultures positive) Haddow et al. Lancet Infect Dis. 2010; 10:791-802 Maziarz & Perfect: Infect Dis Clin N Am . 2016;30:179-206
Immune Reconstitution Inflammatory Syndrome Predictors: 1. High fungal burden at diagnosis and at start of ART: baseline CrAg titre >1:1024, fungaemia + poor fungal clearance positive CSF cultures prior to ART start 2. Host immune factors: rapid immune reconstitution (decline in HIV viral load , increasing CD4 count); poor CNS inflammatory responses (CSF WBC and cytokine responses pre-ART including TNF alpha and IFN gamma) Longley et al. Curr Opin Infect Dis. 2013; 26(1): 26 34
Immune Reconstitution Inflammatory Syndrome Management of C-IRIS No trials: based on expert opinion Check adherence to fluconazole/ ART Do LP / investigate to seek alternative explanations Modification of antifungals not indicated; Continue ART Minor cases improve without specific treatment Corticosteroid therapy if persistent/ severe CNS manifestations: 0.5 1.0 mg/kg per day of prednisolone or dexamethasone: 2-6 weeks reducing Anti-TNF- / thalidomide case reports Longley et al. Curr Opin Infect Dis. 2013; 26(1): 26 34 Maziarz & Perfect: Infect Dis Clin N Am. 2016;30:179-206 Therapeutic LPs if raised CSF OP
Prevention of IRIS Paradoxical: Use best available initial induction CM treatment regimen to sterilise the CSF (AmB 1mg/kg/d+5FC 100mg/kg/d OR Fluconazole 1200mg/d+5FC) Perform LP at 2 weeks to assess CSF culture status Prompt ART initiation: aim to start at 4-6 weeks from CM diagnosis: when CNS symptoms (incl raised ICP) resolved and CSF cultures sterile Unmasking Screen for serum CrAg in patients with CD4<100/uL: if positive, LP if symptoms; treat pre-emptively with fluconazole
Summary C-IRIS is due to exaggerated immune responses to Cryptococcus after immune restoration Can be both unmasking and paradoxical: diagnosis challenging (case definition) CNS manifestation most common (raised ICP, seizures) Corticosteroids for refractory symptoms; mortality low if recognised early and managed Can be prevented by good induction CM treatment, appropriate ART timing and CRAG screening programmes