Understanding Consent and Governance in Health and Social Care
The Health and Social Care Act 2008 outlines the importance of obtaining consent for the care and treatment of service users, incorporating regulations from the Mental Capacity Act 2005 and Mental Health Act 1983 where necessary. The Francis report emphasizes the need for informed consent or lawful authority for all treatments to prevent unlawful actions. Proper consent processes also tie into risk management standards, with the requirement for information disclosure to ensure valid consent. Essential elements of valid consent include voluntariness, capacity, and informed decision-making, free from undue influence. Failure to adhere to these principles can lead to legal and professional consequences.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
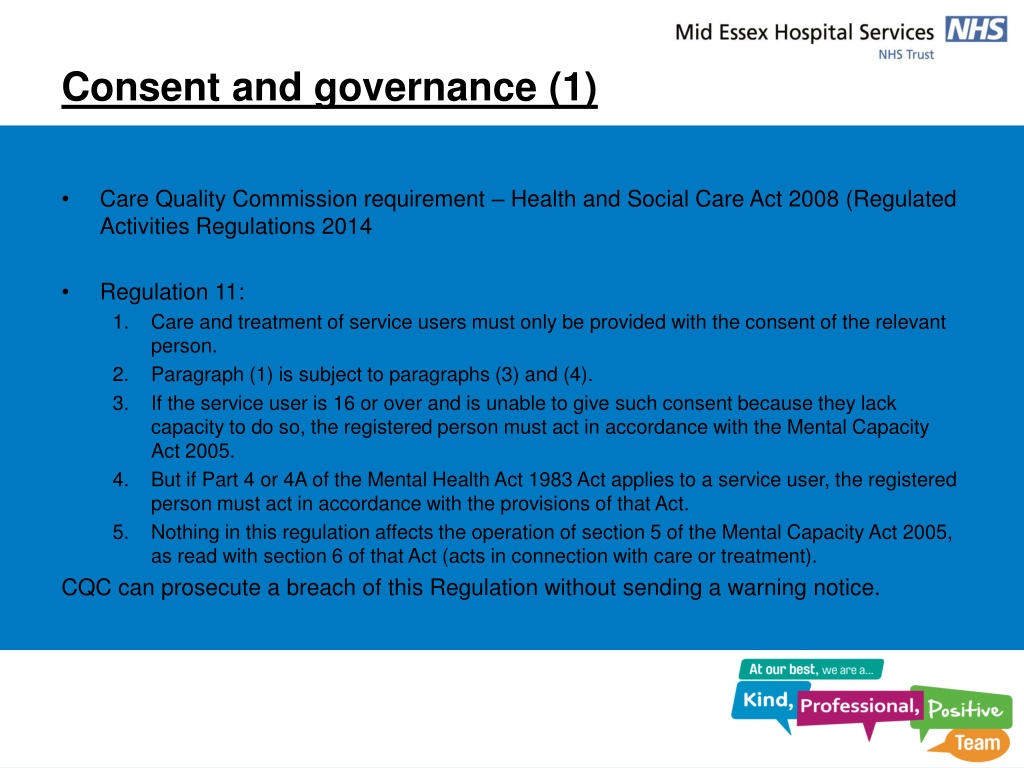
Consent and governance (1) Care Quality Commission requirement Health and Social Care Act 2008 (Regulated Activities Regulations 2014 Regulation 11: 1. Care and treatment of service users must only be provided with the consent of the relevant person. 2. Paragraph (1) is subject to paragraphs (3) and (4). 3. If the service user is 16 or over and is unable to give such consent because they lack capacity to do so, the registered person must act in accordance with the Mental Capacity Act 2005. 4. But if Part 4 or 4A of the Mental Health Act 1983 Act applies to a service user, the registered person must act in accordance with the provisions of that Act. 5. Nothing in this regulation affects the operation of section 5 of the Mental Capacity Act 2005, as read with section 6 of that Act (acts in connection with care or treatment). CQC can prosecute a breach of this Regulation without sending a warning notice.
Consent and governance (2) Francis report: It is unacceptable for treatment to be given to a patient without his or her informed consent or other lawful authority [there should be a] system that ensures consent or other lawful authority is obtained for all treatment. As giving treatment without consent is unlawful, it is reasonable to require the system to be infallible, as redress for the patient and sanctions should follow automatically
Consent and claims If you d properly explained the risks associated with what you were going to do, I d have said no! If you d properly told me why I needed treatment, I d have agreed to it! Appears on most claim forms Consent processes feed into NHSLA Risk Management Standard 5
Risks No information given at all = criminal/civil assault + battery Some information provided = consent itself is valid, but failure to give sufficient information could be negligent Breach of professional duties GMC good medical practice paragraph 49 NMC code paragraph 4
Three elements to valid consent Must be a voluntary decision: no undue influence Patient must have capacity to consent Patient must be informed Consent is not just a signature on a consent form!
1. No undue influence Valid consent has to be a voluntary decision: no pressure no coercion no duress Sources of coercion: family members friends religious leaders Clinicians?
Mental Capacity Act 2005 (MCA) s.1: The principles Presumption of capacity unless proved to contrary All practicable steps to help make decision May have capacity even if unwise decision Act/decision on behalf of P must be made in P s best interests Consider if purpose achievable in less restrictive way
MCAs. 2: People who lack capacity a person lacks capacity ... if at the material time he is unable to make decision for himself in relation to the matter, because of an impairment of, or disturbance in the functioning of, the mind or brain. Loss of capacity may be temporary or permanent May be capable of making some, but not all, decisions Decide on balance of probabilities
Common Law: Capacity Re C (Adult: Refusal of Treatment) [1994] The individual is presumed to have capacity to make a treatment decision; unless unable to take in and retain the information material to the decision, especially as to the likely consequences of having or not having the treatment; or is unable to weigh the information in the balance, as part of the process of arriving at the decision
MCA, s.3: Inability to make decisions A person is unable to make a decision for himself if, at the material time, he is unable to understand the information relevant to the decision retain that information use or weigh that information as part of the process of making the decision; or communicate his decision
Mental Capacity Act Advance Decisions (3)
Mental Capacity Act - Lasting Powers of Attorney (1) P can create an LPA This gives the Donee (D) authority to make decisions for P on personal welfare (to include consenting to or refusing treatment) The LPA must be registered with the Court of Protection to be valid Under Section 10 Donee must be over 18
What to tell the patient What to tell the patient