Efforts to Improve Healthcare Access and Enrollment in Virginia
The Virginia Department of Medical Assistance Services, under the leadership of Deputy Director Rachel Pryor, is implementing various initiatives to enhance member engagement, streamline eligibility and enrollment processes, increase coverage for parents and children, and improve application processing and retention at renewal. These efforts include specialized units for pregnant women, alignment of policies, and collaborations with health plans to automate renewals effectively. By focusing on outreach, enrollment, and system improvements, Virginia aims to ensure better healthcare access for its residents.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
VIRGINIA DEPARTMENT OF MEDICAL ASSISTANCE SERVICES Rachel Pryor, JD, MSW Deputy Director, Administration
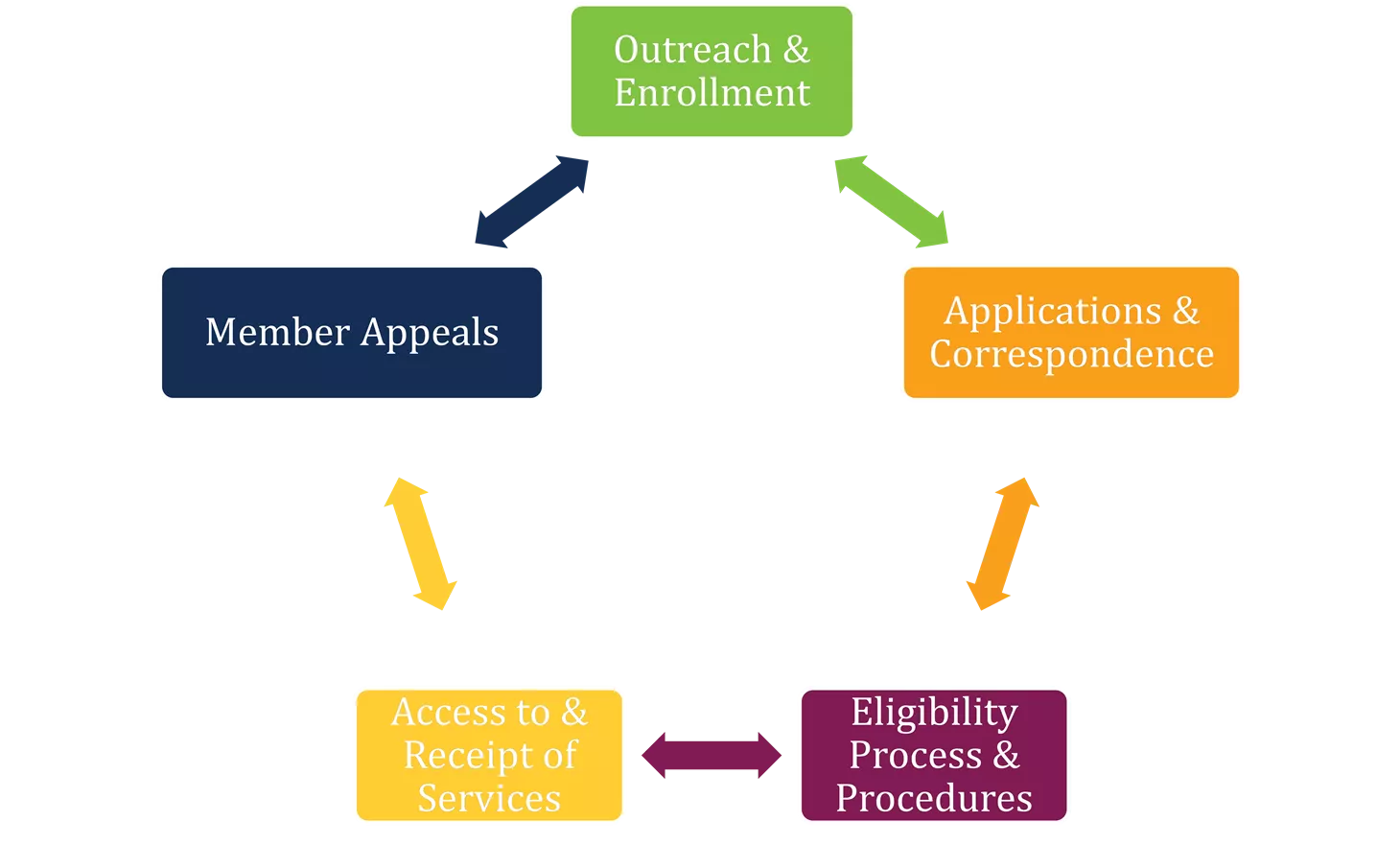
Member Engagement Initiatives . Outreach & Enrollment Applications & Correspondence Member Appeals Target Mapping Access to & Receipt of Services Eligibility Process & Procedures 2
Parent and Caretaker Enrollment Children with uninsured parents have a greater chance of being uninsured; expansion in Virginia has resulted in more eligible parents and caretakers; increasing enrollment of covered children. Enrolling Children Newly Enrolled Parents Parent and Caretaker Participation Medicaid Expansion: as of January 16th, more than 372,000 newly eligible adults are enrolled Over 115,000 newly enrolled adults are parents Coverage for parents results in increased enrollment for children 3
Alignment of Policy Streamlining Eligibility & Enrollment Exploring Medicaid & SNAP Policy Options Policy and system changes to streamline eligibility processes. Benefit enrollment alignment policy options Evaluating systems and procedures to streamline enrollment into Managed Care Organizations 4
Application Processing Improvements Specialized Unit for Pregnant Women: In the summer of 2020, a new specialized unit for processing pregnant woman applications is planned at the Cover Virginia Call Center Shorter Application Processing Time Frame: Previously, applications for pregnant women were processed in ten days. Virginia has a new performance goal to be implemented in 2020 to process pregnant women applications within seven days. 5
Retention at Renewal Through system improvements and collaborations with health plans, Virginia has worked to increase the success rates of automated renewals and increase member retention at renewal 74% of renewals for parents and children successfully complete the renewal process automatically Ex Parte Renewals Health plans are provided with listing of renewals that do not complete the ex parte process Telephonic, text, and mail outreach sent members Renewal Data & Health Plans 6
Planned Coverage Improvements Extension of postpartum coverage for FAMIS MOMs from 60 days to 12 months to provide continuous care for mothers to promote health and well-being of moms and babies. MCO Contract Changes - updates to the MCO contracts to further support maternal and child health and wellness initiatives to include: Care coordination for the high-risk maternity program in order to ensure continuity of care across MCOs Maternal mental health screening Implementation of the evidence-based practice of Screening, Brief Intervention, and Referral to Treatment (SBIRT) to identify, reduce and prevent problematic use, abuse, and dependence on alcohol and illicit drugs Behavioral Health Redesign Proposed plan will implement six critical services that target perinatal populations. In addition, the services will focus on early childhood interventions to prevent child welfare involvements. 7
Future Initiatives Home Visit Services to promote health and well-being of women, children and their families. Home visiting provides social, health and/or educational services to parents and young children that can help support healthy child development prevent health and social problems such as child abuse and neglect. ARTS/SUD IMD as a Covered Benefit for FAMIS MOMS - To allow FAMIS MOMS (pregnant, non-Medicaid-eligible women below 205 percent FPL covered through CHIP) to access medically necessary treatment for a substance use disorder in an Institution for Mental Diseases (IMD) under the Addiction and Recovery Treatment Services (ARTS) waiver. Doula Services to provide individualized care for women, coordinating both healthcare and non-healthcare-related services that women need during pregnancy. Doula services have been demonstrated to decrease delivery times, increase birth weights, decrease pre-term birth, and increase rates of breastfeeding among pregnant women. 8
Marketing and Outreach Community Outreach Coordinators Radio Online Advertisement Advertisement Partnership with WIC Offices Community Partners 9
Member Communications In 2019, Virginia focused on improvements to member communication Improvements to all member eligibility notices and letters to improve member readability providing clearer information regarding eligibility and covered services to consumers, facilitating timely access to needed care Improved translation services; to include top 17 languages in Virginia implemented in systems that generate member communications 10
Medicaid Member Advisory Committee (MAC) Integral piece in providing feedback to proposed changes & input from personal experience To obtain the insight & recommendations of enrollees to help improve enrollment & health care delivery. New Advisory Committee to the Director Members targeted outreach & enrollment difficulties & standardization across health plans First Quarterly meeting held April 1,, 2019 11
Medicaid Member Advisory Committee (MAC) Examples of member-selected themes in 2019: DMAS outreach and enrollment strategies Feedback from the MAC on new changes to consumer Medicaid correspondence Member discussion on member services and consumer accessibility in Medallion 4.0 and CCC Plus Opportunity for free discussion on other topics desired by members 12
THANK YOU 13