Understanding Congestive Heart Failure: Causes, Pathophysiology, and Management
Congestive heart failure (CHF) is a condition where the heart cannot pump enough blood to meet the body's needs, often caused by conditions like hypertension and coronary artery disease. Factors affecting cardiac output include preload, heart rate, stroke volume, afterload, and contractility. The pathophysiology of CHF involves decreased stroke volume, compensatory mechanisms like SNS stimulation, and hormonal responses triggering vasoconstriction and fluid retention. Proper diagnosis and management are crucial in addressing CHF.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
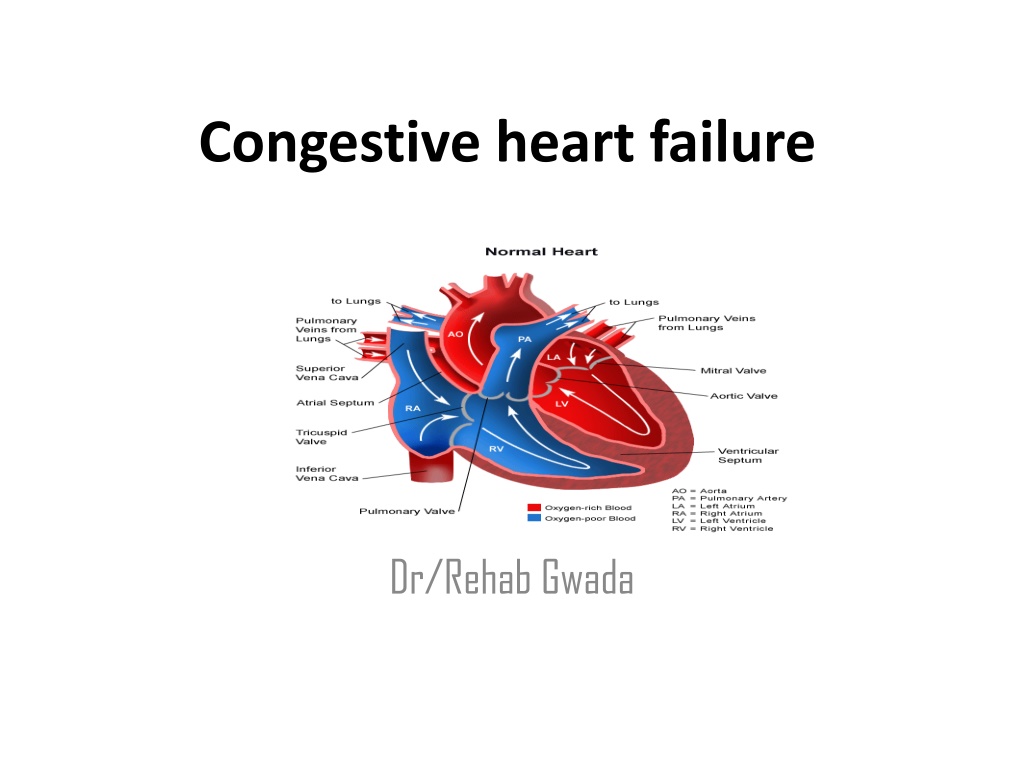
Congestive heart failure Dr/Rehab Gwada
Objectives Define Congestive Heart Failure. Outlines the Factors Affecting Cardiac Output Discuses the Causes and pathophysiology differentiate between Types of heart failure Identify Clinical manifestations outlines Classification of heart failure identify Diagnostic evaluation Explain the management
What is the Congestive Heart Failure Impaired cardiac pumping such that heart is unable to pump adequate amount of blood to meet metabolic needs Not a disease but a syndrome Caused by long-standing HTN and CAD The heart pumps blood inadequately, leading to reduced blood flow, back-up (congestion) of blood in the veins and lungs, and other changes that may further weaken the heart.
Factors Affecting Cardiac Output Preload X = Cardiac Output Heart Rate Stroke Volume Afterload Contractility
Factors Affecting Cardiac Output 1) 2) Heart Rate Preload The volume of blood/amount of fiber stretch in the ventricles at the end of diastole (i.e., before the next contraction) It is affected by venous blood pressure and the rate of venous return. Preload increases as vasoconstriction, and fluid volume increase. 3) Afterload The resistance against which the ventricle must pump. Excessive afterload = difficult to pump blood reduced CO/SV Factors that increase afterload include: stenosis, systemic & pulmonary HTN, vasoconstriction. Contractility Ability of the heart muscle to contract; relates to the strength of contraction. aortic and pulumonary 4) Infarctions, Ischemic tissue decreases contractility.
Pathophysiology of CHF Pump fails decreased stroke volume /CO. Compensatory mechanisms kick in to increase CO 1. SNS stimulation release of epinephrine/nor- epinephrine 1. Increase HR 2. Increase contractility 3. Peripheral vasoconstriction (increases afterload) 2. Myocardial hypertrophy: walls of heart thicken to provide more muscle mass stronger contractions
Pathophysiology of CHF 3. Hormonal response: renal perfusion Thus: Kidneys release renin, which stimulates conversion of angiotensin I angiotensin II, which causes: 1. Aldosterone release Na and water retention 2. Peripheral vasoconstriction.
Pathophysiology of CHF Compensatory mechanisms may restore CO to near-normal. But, excessive the compensatory mechanisms can worsen heart failure. Why?.
Pathophysiology of CHF 1. Vasoconstriction: the resistance against which heart has to pump (i.e., afterload), and therefore CO 2. Na and water retention: fluid volume, which preload. If too much stretch (too much fluid) strength of contraction and CO (Starling s Law ) 3. Excessive tachycardia diastolic filling time ventricular filling SV and CO
Causes of congestive heart failure Coronary artery disease High blood pressure vasoconstriction causes a higher pressure which causes CHF when hypertrophy from working too hard, because the heart tires out. Heart valves disorders The valves don't close regurgitation. Inflammation of Heart cardiomyopathy) Heart attack(MI as it changes the functioning of the heart). properly allowing muscle (myocarditis,
Causes of congestive heart failure (cont) Severe hypertension) Severe anemia Overactive thyroid gland (hyperthyroidism) Underactive thyroid gland (hypothyroidism) Abnormal heart rhythms ( atrial fibrillation) Atrial fibrillation (usually an electrical problem) the blood is not going into the ventricles properly. Kidney failure lung disease ( pulmonary
Congestive heart failure Types Left-sided heart failure There are two types of left-sided heart failure Systolic dysfunction Diastolic dysfunction Right-sided heart failure
Congestive Heart Failure Types of Congestive Heart Failure Left-sided failure Most common form Blood backs up through the left atrium into the pulmonary veins Pulmonary congestion and edema Eventually leads to biventricular failure
Cont. Right-sided failure Blood backs up into right atrium and venous circulation Venous congestion Peripheral edema Hepatomegaly Splenomegaly Jugular venous distension
Chronic Congestive heart failure Clinical manifestations Symptoms Dyspnea Paroxysmal nocturnal dyspnea (PND) Orthopnea Reduced exercise fatigue Nocturnal cough Ankle swelling Anorexia tolerance, lethargy,
Chronic Congestive heart failure Clinical manifestations ( cont ) Signs Cachexia and muscle wasting Tachycardia Pulsus alternans Elevated jugular venous pressure Crepitations Third heart sound Lower extremity edema Hepatomegaly (tender) Ascites
Congestive heart failure Diagnostic evaluation Patient history Physical examination Diagnostic tests 1. Electrocardiography 2. Echocardiography(ejection fraction) 3. Chest x-ray 4. Blood tests 5. Radionuclide 6. magnetic resonance 7. computed tomography imaging 8. cardiac catheterization with angiography 9. a biopsy of heart muscle is needed
Management Strategies for Congestive heart failure Medication CHF Cardiac rehabilitation surgery exercises Lifestyle changes
Congestive heart failure Treatment lifestyle change 1. Salt restriction 2. Exercises 3. Smoking and alcoholism cessation. 4. Body overweight (daily weight) 5. Elevate the feet and legs if they are swollen. 6. Avoid Excessive emotional stress and/or depression 7. Control HTN & cholesterol level 8. Control Diabetes . As ,Diabetes deteriorates blood vessel walls because glucose causing the walls to be sticky.
Congestive heart failure Treatment Medication: Diuretics Inotropic drugs Vasodilators -Adrenergic blockers Opioids ACE inhibitors Cardiac rehabilitation (this program can monitor a person's exercise capacity).
Congestive heart failure Treatment (cont ) (surgical intervention) Percutaneous (Angioplasty) Coronary revascularization) Valve replacement Biventricular pacemaker Heart transplantation coronary intervention artery bypass grafting (