Comprehensive Intervention Plan for Type 2 Diabetes Management in Older Hispanic Female
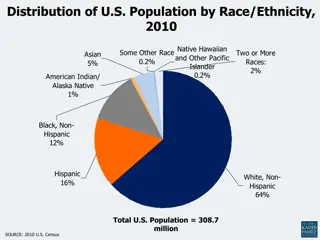
This intervention plan focuses on addressing the challenges of type 2 diabetes in a 78-year-old Hispanic female who lives alone. It includes elements of leadership, collaboration, communication, change management, policy advocacy, and improving quality of care. The plan emphasizes the importance of multidisciplinary teams, clear communication, and adherence to nursing ethics to provide optimal care and support for the patient.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Assessment 4 Part I: Intervention Plan for the Patient Student's Name Institutional Affiliation Course Instructor s Name Date
Introduction This intervention plan is aimed at addressing the health problem, type 2 diabetes, that a 78-year-old Hispanic female encounters. In essence, this plan considers the age factor, the fact that the woman stays alone even though she is in close proximity with the daughter and the family, and the challenges that type 2 diabetes causes to an individual. In that regard, the plan integrates leadership, collaboration, communication, change management, policy, quality of care, patient safety, cost, technology, care coordination and community resources.
Leadership and Change management Effective leadership is necessary in addressing the needs of this patient with type 2 diabetes. Based on this element, the first step is to appoint a multidisciplinary team that includes physicians, dietitians, pharmacists, social workers, and other healthcare professional who will be responsible for providing care to the patient. It is apparent that the leadership provides vision, sets goals for care, allocates adequate resources, and fosters collaboration to ensure optimum care (O Donovan et al., 2021). If there is a need for change, the leadership will spearhead the change management process through open communication, availing resources, and implementation of education programs thus ensuring patient-centered care.
Collaboration and Communication The successful implementation of this plan will necessitate collaboration amongst healthcare providers, multidisciplinary teams, government agencies healthcare providers, and other stakeholders. Collaboration aids in leveraging different expertise and pooling the resources together to address different risk factors of type 2 diabetes (Abdulrhim et al., 2021). Consequently, clear, open, and effective communication is also mandatory in informing the patient and the stakeholders concerning the program. The audience is also given a chance to ask questions and seek clarification.
Policy At the nursing level, healthcare providers will be expected to adhere to the basic code of ethics in nursing which includes; informed consent, beneficence, non-maleficence, justice, and confidentiality. At the national, state, and local level, nurses are expected to advocate for policies that can conducive environment for managing type 2 diabetes, reducing readmission rates, and optimizing quality care. Matters of priorities for advocacy are improving healthcare access, promotion of healthy food options, and insurance coverage.
Quality of Care During the care, the nurses are to adhere to evidence-based practices to ensure optimum outcomes of care. These evidence-based practices include timely intervention, monitoring of patient health indicators, and patient education amongst others. This strategy will ensure quality care for the patient.
Patient Safety In this plan, ensuring patient safety is an issue of priority. Therefore, during the management of type 2 diabetes, the nurses will ensure comprehensive risk assessment, medication management, and education of patients on self-care practices. These strategies will prevent any further complications or adverse effects linked to type 2 diabetes.
Costs to the System and Individual This plan aims at reducing the cost of acquiring healthcare services. For instance, the plan recommends continuous monitoring, early intervention, complications prevention, and promotion of healthy lifestyles. Moreover, the plan adapts the use of telemedicine, promotes group education sessions, and integrates community resources to assist in mitigating excessive financial burdens that relate to the management of type 2 diabetes.
Technology Utilization of technology is another issue of priority in this plan. Technologies such as electronic health records, wearable devices, remote monitoring devices, telemedicine, and mobile apps will be integrated into type 2 diabetes management. Technologies are essential in promoting remote monitoring, real-time communication, medication adherence, and accuracy in data processing amongst others (Li et al., 2023). Therefore, the technology will assist in reducing cost, enhancing access, and minimizing instances of error thus optimizing patient outcomes.
Care Coordination The leadership of the healthcare setting establishes a care team that includes nurses, physicians, dietitians, and social workers to improve the continuity of care and the outcome of the patient. This care team will ensure a seamless transition between different healthcare providers and settings. The effectiveness of care coordination will fill the gaps that usually arise in the fragmented healthcare system.
Community Resources During the care management for type 2 diabetes community resources such as support groups, nutrition programs, and fitness centers are engaged. These community resources are essential in providing additional support for individuals with diabetes. Leveraging existing infrastructure and partnering with local organizations enhance the reach and sustainability of the intervention.
Conclusion Effective implementation of this community-based plan to manage type 2 diabetes will translate to positive outcomes. In essence, this plan aims at ensuring the quality of care and the safety of the patient while minimizing the cost of medical services. Nevertheless, every stakeholder has to effectively play their individual role in ensuring the success of this plan.
References Abdulrhim, S., Sankaralingam, S., Ibrahim, M. I. M., Diab, M. I., Hussain, M. A. M., Al Raey, H., Ismail, M. T., & Awaisu, A. (2021). Collaborative care model for diabetes in primary care settings in Qatar: a qualitative exploration among healthcare professionals and patients who experienced the service. BMC Health Services Research, 21(1). https://doi.org/10.1186/s12913-021-06183-z Li, C., Wang, J., Wang, S., & Zhang, Y. (2023). A Review of IoT Applications in Healthcare. Neurocomputing, 127017. https://doi.org/10.1016/j.neucom.2023.127017 O Donovan, R., Rogers, L., Khurshid, Z., De Br n, A., Nicholson, E., O Shea, M., Ward, M., & McAuliffe, E. (2021). A Systematic Review Exploring the Impact of Focal Leader Behaviours on Healthcare Team Performance. Journal of Nursing Management, 29(6), 1420 1443. https://doi.org/10.1111/jonm.13403