Pharmacology of the Autonomic Nervous System Part 2 Summary and Learning Objectives
Explore the pharmacology of the autonomic nervous system focusing on cholinergic and adrenergic agents. Learn about cholinomimetics, direct and indirect acting cholinergic agonists, their therapeutic indications, and adverse effects. Discover the mechanism of action and uses of nicotinic agonists. Dive into the complexities of drug interactions and their impact on bodily functions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Pharmacology of the Autonomic Nervous System Part 2 Thomas E. Tenner, Jr., Ph.D. Dept. of Medical Education Dept. Pharmacology & Neuroscience tom.tenner@ttuhsc.edu 743-7169 1
Recommended Background Reading : Chapters 7, 8, 9, and 10 Basic and Clinical Pharmacology Bertram Katzung (13th Edition) 2
Learning Objectives: 1) List and describe the mechanism of action, therapeutic indications, and adverse effects of cholinergic agonists and cholinesterase inhibitors. 2) List and describe the mechanism of action, therapeutic indications, and adverse effects of muscarinic and nicotinic receptor antagonists. 3) List and describe the mechanism of action, therapeutic indications, and adverse effects of direct, indirect, and mixed acting adrenergic agonists. 4) List and describe the mechanism of action, therapeutic indications, and adverse effects of adrenergic and - adrenergic blocking agents. 3
ANS CHOLINERGIC PHARMACOLOGY 4
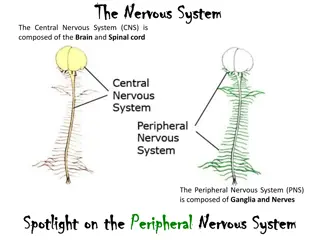
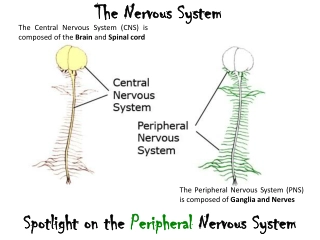
PARASYMPATHOMIMETICS (CHOLINOMIMETICS): Drugs that facilitate or mimic some or all of the actions of the parasympathetic nervous system. Direct Acting Indirect Acting Anticholinesterases Nicotinic receptor agonists Muscarinic receptor agonists Reversible Irreversible 5
Direct Acting Cholinergic Agonists Acetylcholine *not used therapeutically N/M Carbachol * (Miostat) N/M Bethanechol * (Urecholine) M Pilocarpine (Pilocar, Ocusert) M Indications Urinary retention after surgery or postpartum, Glaucoma Adverse effects Muscarinic (M): salivation, flushing, bronchospasm, sweating, nausea, abdominal pain acid indigestion and GI cramping, diarrhea, and possibly, decreased blood pressure. Nicotinic (N)- Fasciculations, respiratory arrest 6
Direct Acting Cholinergic Nicotinic Agonists Nicotine MOA**- Low doses ganglionic stimulation causing euphoria and arousal. CNS effects cause relaxation and improves attention (Acute) Indications None Adverse effects Vomiting, convulsions, hypertension, cardiac arrhythmias, Respiratory arrest (depolarizing blockade), Muscarinic effects - PNS ganglia stimulation. Succinylcholine *: MOA - Overstimulation results in depolarizing blockade Indications muscle relaxation/paralysis associated with intubation, other procedures Adverse effects Fasciculations, respiratory arrest, malignant hyperthermia 7
Indirect Acting Cholinergic Agonists - Reversible Edrophonium*(Tensilon) Neostigmine * Pyridostigmine* (Mestinon,) Physostigmine MOA - Prolongs duration of acetylcholine by binding with and blocking acetylcholinesterase. Therefore both Nicotinic(N) and Muscarinic(M) effects! Indications Myasthenia Gravis, Glaucoma, Atropine Poisoning Adverse effects salivation, flushing, bradycardia, bronchospasm, sweating, nausea, abdominal pain, diarrhea, decreased blood pressure, muscle fasciculations (N), and respiratory arrest (N). 8
Indirect Acting Cholinergic Agonists Reversible - CNS Used in Alzheimer s : Donepezil(Aricept, Aricept ODT) Galantamine (Razadyne, Razadyne ER) Rivastigmine(Exelon) tertiary amine Mechanism of action Increase cerebral concentrations of acetylcholine by inhibiting acetylcholinesterase Adverse effects Same as other reversible ACHase Inhibitors 9
Indirect Acting Cholinergic Agonists - Irreversible Echothiophate* (Phospholine) MOA- Prolongs duration of acetylcholine by permanently inactivating acetylcholinesterase. Therefore both Nicotinic(N) and Muscarinic(M) effects! Indications Glaucoma Adverse effects salivation, flushing, bradycardia, bronchospasm, sweating, nausea, abdominal pain, diarrhea, decreased blood pressure, muscle fasciculations (N), and respiratory arrest (N). 10
SLUDWARMF Sweating Lacrimation Urination Diarrhea Wheezing Accommodation Rhinorrhea Miosis Fasciculations Muscarinic Nicotinic 11
PARASYMPATHOLYTICS (ANTICHOLINERGICS): Drugs that reduce or inhibit some or all of the actions of the parasympathetic nervous system. Nicotinic receptor antagonists Muscarinic receptor antagonists Neuromuscular blocking drugs (Nm) Ganglionic blocking drugs (Nn) 12
Parasympatholytics Muscarinic receptor antagonists MOA- Block muscarinic receptors on the effector organs of the parasympathetic nervous system and on the sweat glands Indications Varied - specificity for muscarinic receptors is a key reason behind their usefulness. Adverse effects Autonomic PNS - dry mouth, blurred vision, tachycardia, urinary retention, and constipation SAS - Inhibition of sweating CNS - restlessness, confusion, and hallucinations Common mnemonic: hot as a hare, blind as a bat, dry as a bone, red as a beet, and mad as a hatter" 13
Parasympatholytics Muscarinic receptor antagonists Atropine Sulfate Cholinesterase poisoning, ACLS: Bradycardia, Pulseless Electrical Activity and Asystole Benztropine (Cogentin) Parkinsonism Dicyclomine (Bentyl) Irritable Bowel Syndrome Ipratropium *(Atrovent) COPD, Rhinorrhea Tiotropium * (Spiriva) COPD, Rhinorrhea Oxybutynin (Ditropan) Overactive bladder Tolterodine (Detrol) Overactive bladder Tropicamide (Mydriacyl) - Mydriasis (short duration) Scopolamine - Motion Sickness, Amnesia 14
Parasympatholytics Nicotinic receptor antagonists- Ganglionic Blockers (NN) Mecamylamine Non-depolarizing, competitive blocker Nicotine Depolarizing blocker High doses ganglionic blockade causing respiratory paralysis and hypotension No selectivity - block receptors on both the parasympathetic and sympathetic ganglia Adverse Effects Intolerable Hypotension, Orthostatic Hypotension, atony of bladder and GI Tract, cycloplegia, xerostomia, sexual dysfunction, hyperthermia Rarely used therapeutically 15
Parasympatholytics Nicotinic receptor antagonists- Neuromuscular Blockers (NM) Tubocurarine* - Prototype Atracurium* Pancuronium * Rocuronium* Vecuronium* Indications muscle relaxation/paralysis associated with intubation, other procedures MOA - Competitive blocker - action can be reversed by increasing concentration of Ach** Adverse Effects Respiratory arrest. 16
ANS ADRENERGIC PHARMACOLOGY 17
Raymond Ahlquist (1948) on Adrenergic receptor function Alpha receptors are excitatory everywhere but the gut Beta receptors are inhibitory everywhere but the heart 18
Adrenergic Agonists Catecholamines - Name is based on their chemical structure (hydroxyl groups at the 3 and 4 position of a benzene ring): High potency - activate both alpha and beta receptors Rapid inactivation - Destroyed by COMT (Catechol O- methyltransferase) and by MAO (Monoamine oxidase) which are both located at the neuron and in the gut wall. Catecholamines are not effective when given orally Poor CNS penetration - They are polar but they still may cause some CNS effects 5 catecholamines - epinephrine, norepinephrine, dopamine, dobutamine, and isoproterenol 19
Epinephrine: Basic Catecholamine Structure H HO CH CH2 N 1 3 4 CH3 HO OH 20
Adrenergic agonists Cont. Non-catecholamines - Not destroyed by COMT and MAO deactivation is limited, so they have longer half lives Better CNS penetration due to increased lipid solubility 25
SYMPATHOMIMETICS: Drugs that facilitate or mimic some or all of the actions of the sympathetic nervous system. Direct Acting Indirect Acting Mixed Acting -adrenergic agonists Drugs that facilitate NE release Both Direct and Indirect Actions Drugs that block NE uptake -adrenergic agonists Drugs that inhibit enzymatic breakdown of NE 26
Mechanism of action of adrenergic agonists Direct-Acting Agonists - Mimic NE and EPI. They bind to the adrenergic receptors without interacting with the prejunctional neuron. (EPI, NE, ISO and Phenylephrine) Indirect-Acting Agonists: Displace norepinephrine from storage sites (Amphetamine, hydroxyamphetamine, and tyramine) Block the uptake of norepinephrine at storage sites (Cocaine, Tricylic Antidepressants, SNRI) Inhibit enzymatic breakdown of norepinephrine (Monoamine Oxidase Inhibitors, i.e., phenelzine) Mixed-action agonists - Both stimulate receptors and displace NE from storage sites. (Ephedrine, pseudoephedrine)
Catecholamines: Rank Order of Potency Isoproterenol: 1 = 2 = 3 >>>> 1 = 2 Norepinephrine : 1 = 2 = 1 = 3 >>>> 2 Epinephrine: 1 = 2 = 1 = 2 = 3 Dopamine : DA 1> 1> 1 28
Adrenergic Receptor Subtypes -adrenergic receptors (Epinephrine > Isoproterenol) -adrenergic receptors (Isoproterenol > Epinephrine) 1-adrenergic receptors (Phenylephrine > Clonidine) 1-adrenergic receptors (EPI = NE) 2-adrenergic receptors (EPI>NE) 3-adrenergic receptors (NE>EPI) 2-adrenergic receptors (Clonidine > Phenylephrine) 29
Direct Acting Alpha1 - Adrenergic Agonists Phenylephrine (Neo-Synephrine) Oxymetazoline ( Afrin, Visine L.R.) Indications Nasal decongestant, mydriatic, and systemically as a vasopressor for hypotension to raise BP. Adverse effects Hypertension, Nervousness, Headaches 30
Direct Acting Alpha 2 - Adrenergic Agonists Clonidine (Catapres) Apraclonidine a (Lopidine) Brimonidine a(Alphagan P) Indications : Hypertension - produces inhibition of sympathetic vasomotor centers, reducing blood pressure. ADHD and impulsive behavior Glaucoma a Adverse effects Bradycardia, Hypotension, Headaches, Sedation, Depression, Caution for Withdrawal Supersensitivity with Chronic use 31
Direct Acting Beta 1- Adrenergic Agonists Dobutamine (Dobutrex) Mechanism of Action Primarily a beta 1 agonist. Increases cardiac output with few heart rate or vascular effects Indication - Congestive heart failure Adverse actions tachycardia, palpitations, severe hypotension (alpha antagonist effect). Can increase ventricular rate in atrial fibrillation 32
Direct Acting Beta 2- Adrenergic Agonists Albuterol (Proventil, Ventolin) Terbutaline (Brethine, Bricanyl) Metaproterenol (Alupent) Long Acting Beta Agonists (LABA) Salmeterol (Serevent) Formoterol (Perforomist) Indications : Bronchodilator, Asthma; LABA only in COPD. Adverse effects Nervousness, muscle tremors, tachycardia. Systemic route: Hypokalemia and hyperglycemia 33
Indirect Acting Adrenergic Agonists Amphetaminea Hydroxyamphetamine Cocaine TCA s, SNRI sb MAOI sb Indications : Attention Deficit Disorder (ADD) a Narcolepsya Depressioni/Neuropathic painb Adverse effects Similar to direct acting Adrenomimetic drugs. (See next slides). 34
Amphetamines - Adverse Effects: CVS GI CNS confusion insomnia irritability weakness vertigo/dizziness tremor hyperactive reflexes delirium panic suicide amphetamine psychosis palpitations arrhythmias hypertension angina circulatory collapse headache chills sweating anorexia nausea, vomitinmg & diarrhea abdominal cramping
Cocaine Adverse Effects: 1) Anxiety* reaction (hypertension, tachycardia, sweating & paranoia) 2) Depression 3) Agitation* 4) Cardiac Arrhythmias 5) Seizures* 6) Incidence of MI unrelated to dose, duration of use or route of administration (no marker) * Can be treated with Benzodiazepines-Diazepam
SYMPATHOLYTICS: Drugs that reduce or inhibit some or all of the actions of the sympathetic nervous system. Ganglionic blocking drugs -adrenergic antagonists -adrenergic antagonists Adrenergic neuronal blocking drugs
Adrenergic Neuronal Blocking Drug Reserpine Discontinued in US MOA: Prevents uptake of biogenic amines (DA, NE, EPI, 5HT) in both central and peripheral neurons (also adrenal chromaffin granules) Results in Biogenic amine depletion - denervation Indications : Hypertension . Adverse effects Diarrhea, cramps, GI acid secretion, postural hypotension, bradycardia, sexual dysfunction, sedation, depression (suicide). Caution for Supersensitivity with Chronic use. 38
Nonselective Alpha Adrenergic Blocking Agents Phentolaminea (Regitine) reversibleand competitive Phenoxybenzamineb (Dibenzyline) irreversibleand non-competitive MOA block both Alpha1 and Alpha2 Indications : Diagnosisa and Treatmentb of Pheochromocytoma Adverse effects Orthostatic hypotension, exaggerated reflex tachycardia (why), nasal stuffiness, ejaculatory dysfunction 39
Alpha-1 Selective Adrenergic Blocking Agents Prazosin (Minipress) - Prototype Doxazosin (Cardura) Terazosin (Hytrin) Tamsulosin (Flomax) Selective for Alpha 1Aa Indications: Hypertension not monotherapy Benign Prostatic Hypertrophya- relaxes bladder neck and prostate smooth muscle 40
Alpha-1 Selective Adrenergic Blocking Agents Adverse effects : First Dose Effect - Exaggerated hypotension that can lead to syncope especially when patient stands after sitting or lying down (orthostatic hypotension) less reflex tachycardia (why) sodium and water retention (prazosin) (limits use in high blood pressure) nasal stuffiness ejaculatory dysfunction 41
Beta Adrenergic Blocking Agents Propranolola (Inderal) Timolol a(Timoptic) Nadolola (Corgard) Atenolol b(Tenormin) Metoprololb (Lopressor) Esmololb (Brevibloc) MOA : aNonselective - both beta-1 and 2 b Cardioselective Beta-1 specific 42
Beta Blockers Indications cont. Indications : Prevention of migraines - May prevent catecholamine vasodilation in the brain vasculature (Beta-2?) Hyperthyroidism Thyroid storm Glaucoma (Timolol) Arrhythmias, Angina pectoris, Myocardial Infarction, Heart failure Protective effect against sympathetic overstimulation improved survival !! Adverse reactions Bradycardia, Heart block, Heart failure, Raynaud s (peripheral vasospasm), Vivid dreams, depression, Bronchoconstriction in asthmatics/COPD, Sexual dysfunction, Decreased glycogenolysis and glucagon secretion Caution for Withdrawal Supersensitivity with Chronic use 43
Alpha and Beta Adrenergic Blocking Agents Labetalol a(Trandate, Normodyne) Carvedilolb(Coreg) MOA block both Alpha1 and Beta Adrenoceptors. Result in peripheral vasodilation that lowers blood pressure with reduced cardiac rate and contraction Indications : Hypertension a and Congestive heart failure b Adverse effects Combines BOTH Alpha and Beta adrenoceptor blocker adverse effects. 44
Process Affected Receptor Activation or Blockade Drug Example Bethanechol, Pilocarpine Atropine Site Muscarinic Receptor Activation Muscarinic Receptor Blockade Nicotinic Receptor Activation Nicotinic Receptor Blockade 1, 2, 1, 2, 3 Receptor Activation 1, 2, 1, Receptor Activation 1 Receptor Activation 1, 2, Receptor Blockade 1 Receptor Blockade 1, 2, 3 Receptor Activation 1, 2, 3 Receptor Blockade Action Parasympatho- mimetic, Parasympatholytic Nicotine Skeletal muscle activation Muscle paralysis, respiratory arrest Sympathomimetic Tubocurarine Epinephrine Norepinephrine Sympathomimetic Phenylephrine Phentolamine Sympathomimetic Sympatholytic Prazosin Isoproterenol Sympatholytic Sympathomimetic 45 Propranolol Sympatholytic
Target Organ Responses Adrenergic and Cholinergic Receptors Adrenergic 1 2 Cholinergic M 1 2 N Subtype: Agonist Antagonist Location Importance 46
Prototype Drugs Adrenergic Cholinergic Synthesis/storage Release Receptor Agonist Antagonist Removal 47
Control of Blood Pressure Arterial - Afterload mABP = CO x TPR HR SV Cardiac - Chronotropy CF VR Venous Preload Cardiac - Inotropy 48