Understanding Ventricular Septal Defect (VSD) and Treatment Options
Ventricular Septal Defect (VSD) is a common congenital heart condition characterized by a hole in the septum between the heart's ventricles. This defect can lead to various complications and is often associated with chromosomal disorders. Different types of VSD exist, each requiring tailored treatment approaches, including surgical closure or percutaneous device placement. Understanding the types, causes, and treatment options for VSD is crucial for managing this condition effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
VENTRICULAR SEPTAL DEFECT
Henri roger French paediatrician Maladie de Roger (Roger's disease or defect small muscular VSD bruit de Roger (Roger's murmur)- loud pansystolic murmur of VSD
Most common congenital heart disease excluding bicuspid aortic valve 20%of VSD occur as a part of complex CHD 80% occurs as an isolated defect
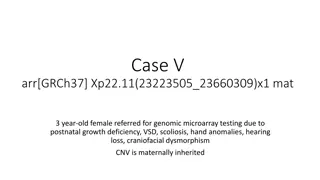
CHROMOSOMAL DISORDERS ASSOCIATED WITH VSD Trisomy 21- 40% will have inlet VSD Trismy 13 patau s Trismy 18 Edwards Digeorge syndrome 22q11 deletion Holt oram syndrome
Mostly muscular VSD refers to trabecular VSD , although muscular part includes both inlet and outlet
TYPE 1 OUTLET VSD : CONAL , SUBPULMONARY, INFUNDIBULAR , SUPRACRISTAL , DOUBLY COMMITED TYPE II MEMBRANOUS VSD PERIMEMBRANOEUS, CONOVENTRICULAR, SUBAORTIC TYPE III ATRIOVENTICULAR SEPTAL DEFECT :INTELT VSD, AVSD, ENDOCARDIAL CUSHION DEFECT TYPE IV MUSCULAR VSD , TRABECULAR, SWISS CHEESE VSD
MEMBRANOUS VSD Most common VSD 80% PerimembranousVSD with outlet extension TOF type PerimembraneousVSD with inlet extension ECD type PerimembranousVSD with muscular extension MembraneousVSD can be partially closed by septal leaflet of tricuspid valve. The conduction pathway passes adjacent to the membranous VSD It directly does not cause any conduction defects , but during surgery , suturing can hamper the conduction pathway leading to a post op RBBB
TREATMENT 1/3rd resolve spontaneously Surgical closure standard treatment Percutaneous device- off label
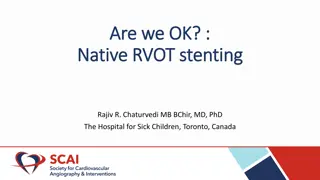
OUTLET VSD Outlet septum separates the pulmonary arteries from aorta and also seperates the RVOT from LVOT In outlet VSD, there is a communication between RVOT and LVOT LV directly ejects blood through the pulmonary artery and aorta , doubly commited Incidence rare
MECHANISM OF AR IN OUTLET VSD VENUTRI EFFECT On either side of a high velocity jet , a low pressure zone is created
The low pressure created in the pulmonary artery pulls the coronary cusp into RVOT during systole The cusp goes back to the normal location during diastole Repeated movement of cusp , damages the cusp , creating AR OR SOVA
AR in VSD is independent of size , its location matters. OuletVSD , rarely perimembranous can cause AR . VSD+AR cause Additional LV volume overload . Eisenmenger is rare. Occurs around 3-8 years of age . Cuspal prolapse can partially close VSD
TREATMENT Never close Surgical closure Mild AR surgical VSD closure only Moderate AR repair of aortic valve is considered along with surgical VSD closure. Severe AR aortic valve repair or replacement with surgical VSD closure is mandatory .
INLET VSD AV canal defects / endocardial cushion defects Down syndrome, Ellisvancrevald syndrome Never close
MUSCULAR VSD Trabecular VSD Single or multiple (swiss cheese septum)
May spontaneously close due to septal contractions. 2/3 rd of muscular VSD can close Device closure Amplatzer muscular VSD cccluder Surgery
HEMODYNAMICS Depends on 3 factors Size of the VSD RV and LV pressure PVR and SVR
SIZE OF THE VSD In small VSD , the large pressure difference between LV and RV during a systole , a high velocity get is created. This creates a loud pansystolic murmur with thrill In case of large VSD , LV and RV behave as a common chamber due to pressure equalization , so murmur will not that much audible
WHEN DOES L TO R SHUNT ESTABLISHES? Around 4-6 weeks of age This is the time taken for fall in RV pressure below LV pressure. At birth , VSD shunt murmurs are not present
HEMODYNAMIC CLASSIFICATION Restrictive- LVSP > > RVSP Pulmo /Aortic systolic pressure ratio < 0.3 Qp / Qs < 1.4 : 1 Moderately restrictive RVSP high, but less than LVSP Qp/Qs 1.4 - 2.2 : 1 Pulmo/aortic systolic pressure ratio<0.66
Non restrictive/ large - >1.0 cm2 ( equal to or greater than to the size of aortic orifice Qp/Qs > 2.2. Pulmo/ aortic systolic pressure ratio>0.66 Flow determined by PVR Large hemodynamically significant L to R shunt Equal LV and RV pressure- act as single chamber during systole . SBP of LV and RV are identical Present as LA, LV volume overload + RV pressure overload.
As the size of the VSD increases More left to right shunt More blood flow through pulmonary arteries Hyperkinetic pulmonary artery hypertension
RA/RV IN VSD WITH L TO R SHUNT Blood is ejected into RV during systole , when it is contracting and ejecting blood into pulmonary artery . No volume overload / no dilatation of RV Some times VSD may be directed towards pulmonary artery , pumping into it directly .
LARGE / NON RESTRICTIVE VSD Pulmonary artery , LA, LV volume overloaded RV pressure overload leads to increased pulmonary vascular resistance Signs PSM -mitral MDM + LVS3 -loud P2 - Narrowed S2 split Eisenmenger single sound s2.
Hyperkinetic PH develops by 2 months later develops into PVOD (pulmonary vascular obliterative disease) PAH Eisenmenger syndrome RV failure Initially hyperkinetic PH , later due to PVR
CLINICAL FEATURES Retarded growth and development Exercise intolerance Recurrent respiratory tract infection CHF
SMALL/RESTRICTIVE VSD <0.5 cm2( smaller than aortic valve orifice area) Small L to R shunt Normal RV output 75% close spontaneously < 2 years Present as loud PSM LLSB or early systolic murmur in a small muscular VSD . Thrill + Increased Infective endocarditis risk high pressure jet ,on RV side
TIME OF CLOSURE Most destined to close by 1 year 60% by 3 year 90% by 8 years Max age 46 years
Common in smaller VSD Asymptomatic VSD (45% vs 7% in CHF) Partial closure occurs equally in small and large But total differs (71% in small and 54% in large ) Even large VSD can spontaneously close
SPONTANEOUS CLOSURE IS RARE IN Inlet VSD Outlet VSD MalalignedVSD
COMPLICATIONS CHF ( seen beyond 1 month upto 6 months of age ) AR (outlet VSD) SOVA Infective endocarditis(usually > 1-2 years of age , but can occur at any age ) Eisenmenger syndrome (30-50% of large VSDs) Acquired PS gasula defect Jet of VSD . If hits pulmonary artery , causes pulmonary artery hypertrophy and leads to development of acquired PS Arrythemias VT , SVT , AF , sudden death can also occur.
INFECTIVE ENDOCARDIRITIS Membranous VSD - vegetation on the tricuspid valve Infundibular defects - aortic or pulmonary valve vegetation. MusclarVSD RV side of the defect. ACC/AHA -- no antibiotic prophylaxis for the acyanotic uncomplicated VSD with no prior history of endocarditis. Patients with a proven episode of endocariditis- increased risk of recurrent infection surgical closure may be recommended. Patients with a proven episodpate of endocarditis increased risk for recurrent infection so surgical closure may be recommended
IE PROPHYLAXIS The 2007 guidelines of the AHA recommend no antibiotic prophylaxis in children with an isolated VSD except : During the first six months after the repair with prosthetic material or device Repaired VSD with a residual defect at the site or adjacent to the site of a prosthetic device Prophylactic antibiotics is recommended for dental and respiratory tract procedures
IMPROVEMENT OF SYMPTOMS IN VSD. Closing defect - soft S2, high frequency & shorter murmur Increasing PVR : increased RV pulsations ,S2 loud & narrow split Infundibular hypertrophy & resulting decreased L to R shunt : S2 decreases in intensity ,crescendo-decrescendo systolic murmur in the ULSB Cyanosis (shunt reversal ).
INVESTIGATION LV volume overload and and RV pressure overload Small VSD normal ECG Large VSD-BVH+LAE RAD
KATZ-WACHTEL PHENOMENON :Tall diphasic QRS complexes (>50 mm in height) in the mid-precordial leads (leads V2, V3 or V4) typically associated with Biventricular Hypertrophy (BVH).
CHEST X RAY LA, LV VOLUME OVERLOAD INCREASE IN PULMONARY BLOOD FLOW
ECHOCARDIOGRAPHY TTE+TEE Size of defect Location of defect Shunt direction Rims of defect QP/QS Chambers enlarged Function of chamber PA pressure Associated abnormalities