Understanding Trauma in Pregnancy and Intimate Partner Violence
Pregnancy introduces unique challenges in trauma care due to anatomical and physiological changes. Major physiological alterations impact injury patterns and responses, necessitating specialized management strategies. Blunt trauma incidents during pregnancy, including motor vehicle crashes and falls, pose significant risks to both the mother and baby. Early consultation with obstetricians and surgeons is crucial to mitigate potential complications and ensure optimal outcomes for both patients.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Trauma in Pregnancy and Intimate Partner Violence Kampala Advanced Trauma Care Course
Outline Global context Epidemiology Pathophysiology Anatomic and Physiologic Differences During Pregnancy Management strategies/ Ideal treatment Adaptations for resource-limited settings/ context appropriate treatment Case for discussion
Global context and epidemiology Blunt trauma in Pregnancy Motor vehicle crashes/ pedestrians = 60% Falls = 22% Direct Assault = 17% Other = 1%
Initial Trauma Assessment Pathophysiology Kampala Advanced Trauma Care Course Last Edited August 2016 by Maija Cheung MD & Michael DeWane MD
Pathophysiology Major physiologic changes and altered anatomic relationships during pregnancy change the pattern of injury and the physiologic response to injury Remember there are two patients: mother and baby! The best initial treatment for the baby is optimal resuscitation of the mother. Pregnant trauma patients have higher risk of premature delivery, pregnancy complications, and fetal death Consult a surgeon and an obstetrician early
Initial Trauma Assessment Anatomic and Physiologic Differences During Pregnancy Kampala Advanced Trauma Care Course Last Edited August 2016 by Maija Cheung MD & Michael DeWane MD
Anatomic Differences: Uterine Growth Intrapelvic organ until 12th week Level of umbilicus at 20 weeks At costal margins at 34-36 weeks As the size of the uterus increases, the bowel is pushed toward the head and as a result is somewhat protected in blunt trauma however the uterus, fetus, and placenta are at a higher risk of injury. Amniotic Fluid Can cause amniotic fluid embolism or disseminated intravascular coagulation following trauma if the fluid gets into the maternal intravascular space
Anatomic Differences Continued: Baby Position Third trimester the fetal head is usually within the pelvis Pelvic fracture can result in skull fracture or serious intracranial injury Placenta Vulnerable to shear forces at utero-placental interface Placental Abruption obstetric emergency for mom and baby Placental Vasculature Sensitive to catecholamine stimulation Decrease in maternal intravascular volume -> increased uterine vascular resistance ->reduced fetal oxygenation despite normal maternal vital signs
Changes in Blood Volume and Composition: Relative Anemia: Plasma volume increases steadily until 34 weeks gestation (~40%) Smaller increase in red blood cell volume (~ 25%) Hct 31-35% in late pregnancy is normal Mother may lose 1200-1500 mL of blood before showing signs of hypovolemia however the fetus may be in shock with distress evident by an abnormal fetal heart rate WBC increases to 12-15K during pregnancy and 25K during labor Increased serum fibrinogen and clotting factors (higher risk of DVT) Normal fibrinogen may indicate early disseminated intravascular coagulation Shortened PT, PTT but unchanged bleeding and clotting times
Hemodynamic Changes: Cardiac Output Increased by 1-1.5L/min after 10th week due to increased plasma volume and decreased vascular resistance Supine, vena cava compression can decrease cardiac output by 30% due to decreased venous return from the lower extremities Heart Rate Increases by 10-15 beats per minute
Hemodynamics Continued: Blood Pressure 5-15 mmHg fall in systolic and diastolic pressures during second trimester, returns to near-normal levels at term Can occur when supine due to vena cava compression -> correct by placing patient LEFT side down EKG Axis may shift leftward by 15 degrees Flattened or inverted T waves in III and AVF Increase in ectopic beats
Respiratory Changes: Increased minute ventilation due to increased tidal volume Decreased residual volume associated with elevated diaphragm Hypocapnia (PaCo2 of 25-30 mmHg) common in late pregnancy PaCO2 of 35-40 may indicate impending respiratory failure
Gastrointestinal System: Relaxed lower esophageal sphincter + delayed gastric emptying = Increased Risk of Aspiration Consider early gastric tube decompression Remember anatomic changes due to uterus cause intestines to be displaced towards the head
Renal Function: Glomerular filtration rate and renal blood flow increased Serum creatinine and urea nitrogen fall to 50% normal levels Glycosuria is common Mild hydronephrosis in response to uterine compression of ureters can be seen
Musculoskeletal System: By 7th month: Symphysis pubis widens to 4-8 mm Sacroiliac joint spaces increase Can create confusion when interpreting pelvic x-rays Large, engorged pelvic vessels surrounding gravid uterus can contribute to massive retroperitoneal and pelvic bleeding
Neurologic System: Eclampsia Can mimic head injury Consider especially if seizures with hypertension, hyperreflexia, proteinuria, peripheral edema
Initial Trauma Assessment Initial Assessment and Management Kampala Advanced Trauma Care Course Last Edited August 2016 by Maija Cheung MD & Michael DeWane MD
Primary Survey & Resuscitation: ABCs same in all patients! Assess and resuscitate the mother first. Airway If intubation is required remember to maintain appropriate PaCO2 for stage in pregnancy (30mm Hg in late pregnancy) Breathing Diaphragm elevated Supine position may be difficult for pregnant patient
Primary Survey Continued: Circulation Uterine compression of vena cava reduces venous return thereby decreasing cardiac output and aggravating shock state Place the patient left side down to relieve pressure If patient requires immobilization the spine board can be logrolled 4-6 inches to the left to maintain spinal precautions and decompress the vena cava Due to increased intravascular volume, pregnant patients can lose a significant amount of blood before they become tachycardic and hypotensive but the fetus may be in distress! Give fluids and blood avoid pressors if possible due to reduction in uterine blood flow and resulting fetal hypoxia
Adjuncts to Primary Survey: Abdominal Exam Main cause of fetal death is maternal shock and maternal death Second most common cause of fetal death in trauma is placental abruption Abruption suggested by vaginal bleeding (70%), uterine tenderness, frequent contractions, uterine irritability (contracts when touched) Ultrasound may be helpful but not definitive Uterine Rupture Rare but often fatal for mother and fetus Suggested by abdominal tenderness, guarding, rigidity, rebound tenderness, abnormal fetal lie, easy palpation of fetal parts, inability to palpate fundus Continuous fetal monitoring Heart tones heard by 10 weeks gestation Normal range 120-160 beats per minute
Secondary Survey: Same pattern as for non-pregnant patients Indicated radiographic studies should be performed if necessary as the benefits outweigh the risks to the fetus Diagnostic Peritoneal Lavage If performed, catheter should be placed above the umbilicus using open technique Perineal Evaluation Formal pelvic examination (ideally by obstetrician) Presence of amniotic fluid (pH 7-7.5) suggests rupture of membranes
Additional Considerations Obtain obstetric consult early All pregnant Rh-negative trauma patients should receive Rh immunoglobulin therapy unless the injury is remote from the uterus (ex: isolated distal extremity injury) Give within 72 hours of injury Kleihauer-Betke Test used to detect fetal cells in mother s serum Negative test does not exclude minor degree of feto-maternal hemorrhage
Additional Considerations Continued: Radiologic Concerns Benefits to mother outweigh risk to fetus Radiation Risk to fetus Greatest risk if <25 weeks Teratogenicity Increased lifetime risk of malignancy
Emergency Cesarean Section: Limited role Primarily in unstable mother who is not responding to interventions Little role for perimortem c-sections; rememberif mother has been in shock, fetus has likely been in shock longer For non-hypovolemic causes of maternal cardiac arrest, perimortem c-section occasionally may be successfully performed of within 4-5 minutes of the arrest
Anesthetic Drugs: Paralytic drugs do NOT cross the placenta Drugs used in Anesthesia are (with reasonable certainty) safe in pregnancy Inhalation anesthetics Local anesthetics Muscle relaxants Narcotics Benzodiazepines
Initial Trauma Assessment Intimate Partner Violence & Trauma Kampala Advanced Trauma Care Course Last Edited August 2016 by Maija Cheung MD & Michael DeWane MD
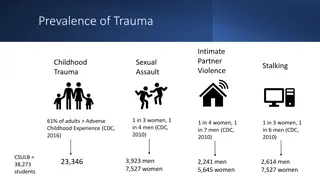
Intimate Partner Violence & Trauma: Major cause of injury to women during cohabitation, marriage and pregnancy regardless of ethnic background, cultural influences, or socioeconomic status Increased incidence during pregnancy 17% of injured pregnant patients experience trauma inflicted by another person 60% of those patients experience repeated episodes of intimate partner violence
Indicators of IPV: Injuries inconsistent with stated history Diminished self-image, depression, suicide attempts Self-abuse Frequent ED or doctors visits Symptoms suggestive of substance abuse Self-blame for injuries Partner insists on being present for interview and exam and monopolizes discussion
Screening Questions for IPV: Have you been kicked, hit, punched, or otherwise hurt by someone in the past year? If so, by whom? Do you feel safe in your current relationship? Is there a partner from a previous relationship who is making you feel unsafe now? These questions when asked in a nonjudgemental manner can identify 65-70% of victims of intimate partner violence.
Initial Trauma Assessment Case Study Kampala Advanced Trauma Care Course Last Edited August 2016 by Maija Cheung MD & Michael DeWane MD
Case: A 25 year old female who appears to be in her third trimester of pregnancy is brought into the emergency room after being struck by a car while crossing the street. What are the initial steps in management?
Useful Resources Trauma.org Trauma Care Manual - Ian Greaves, Keith Porter, Jim Ryan Trauma Management- Demetrios Demetriades, Juan A. Asenio
Collaborators Maija Cheung, MD - Yale General Surgery Resident Michael DeWane, MD - Yale General Surgery Resident Naomi Kebba, MD Surgeon, Uganda Heart Institute Michael Lipnick, MD - UCSF Anesthesiologist Doruk Ozgediz, MD - Yale Pediatric Surgeon Last Edited February 2017 by Maija Cheung MD & Michael DeWane MD