Understanding Marginal Productivity in Health Economics
Learn about the concept of marginal productivity in health economics, the difference between average and marginal productivity, and how it applies to the productivity of medical care. Discover examples of how productivity changes along the extensive margin in specific medical interventions like screening for breast cancer. Explore the implications of varying medical practices and resource use in healthcare.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
MODERN LABOR ECONOMICS THEORY AND PUBLIC POLICY Charles E. Phelps Health Economics 12THEDITION 6THEDITION 3 CHAPTER CHAPTER The Transformation of Medical Care to Health 1 23 November 2024
Learning Goals Understand the meaning of marginal productivity, the difference between average and marginal productivity, and the meaning of extensive and intensive margins. Review estimates of the productivity of medical care in producing health at an aggregate ( all medical care ) level. Become familiar with examples in health care of the marginal productivity of specific medical interventions using cost-effectiveness measures, and understand how these vary along the extensive and intensive margins. Learn how cross-regional medical practice variations signal that providers (doctors) don t always agree about when to use various medical interventions. Learn about how, even within a single region, variations in practice style (and consequent medical resource use) occur. 23 November 2024 2
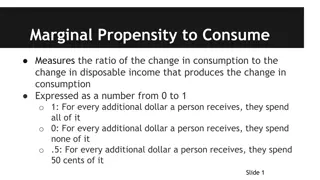
3.1 The Productivity of Medical Care Marginal and Average Productivity The marginal productivity of an input is the additional amount that is added when the last input is added. The average productivity of inputs is total output divided by the number of inputs. The extensive margin refers to how much of the input is used. The intensive margin refers to the rate at which the intensity of use of the input is varied. 23 November 2024 3
3.1 The Productivity of Medical Care Productivity Changes on the Extensive Margin Marginal productivity generally falls as more of a given input is added. Marginal productivity of health care resource is high when there is little health care. Falls as more and more health care resources are used. Could become negative. For example, consider screening for breast cancer (mammograms) Screening gives a yield of positive cases, negatives, false positives, and false negatives. Per 1,000 cases. 23 November 2024 4
3.1 The Productivity of Medical Care Productivity Changes on the Extensive Margin Screening example, continued. Probability of detecting true cases (sensitivity of the test) = p Probability of a false positive = q Let the probability of true positives in the population be f. Then the yield rate of the test is [? ?] + [(1 ?) ?] Suppose that currently, the test is given to women most susceptible to breast cancer, women over 50. Could expand on the extensive margin by adding women 40-49, women 30-39, etc. The number of true cases detected per 1,000 tests would fall as the extensive margin increased because there are fewer true cases in the younger populations. At some point, the marginal product could become negative, if the very slight radiation used in mammograms actually induced some cancers in younger age groups. 23 November 2024 5
3.1 The Productivity of Medical Care Productivity Changes on the Intensive Margin Increasing intensity on the intensive margin would also lead to increasing, decreasing, and possibly negative productivity. In the mammography example, should women in the original group be tested every 10 years, 5 years, 2 years, 1 year, 1 week, 1 day? Testing too rarely means tumors may not be detected Testing too often increases risks and wastes resources. Current recommendation is 1-2 years. 23 November 2024 6
3.1 The Productivity of Medical Care Evidence on Aggregate Productivity of Medical Care Aggregate Data Comparisons Compares the health status of various nations and their use of medical care resources. Simple measures: life expectancy, mortality, infant mortality Could also measure within country Studies invariably show that per capita income, per capita education, medical care use, and good health outcome move in parallel. One exception is in white males in the U.S., where income and mortality are positively correlated, perhaps because higher incomes allow the purchase of more goods that decrease health. Difficult to separate the effects of per capita income, education, medical care use from each other, because they tend to move together. Difficult to estimate how much medical care is used. Currency issues Payment and cost counting methods differ. 23 November 2024 7
3.1 The Productivity of Medical Care Evidence on Aggregate Productivity of Medical Care Aggregate Data Comparisons, continued Studies that use, for example, the same country over time avoid some of these problems. Must still adjust for inflation Shows similar results on per capita income, education, medical spending Hall and Jones (2007) used 1950-2000 data to estimate the production function for health as measured by life expectancy. Then broke down life expectancy by age group, and tied to age-specific patterns of medical care spending. Estimation of the health elasticity of medical spending by age group Percentage change in health (life expectancy) divided by the percentage change in medical care spending. Figure 3.1 23 November 2024 8
3.1 The Productivity of Medical Care Evidence on Aggregate Productivity of Medical Care Medical spending is most productive for small children. Relatively unproductive in the teen years where most causes of death are accidental or violent. Rises up to about age 50, then falls steadily with age, as stock of health is falling and medical intervention is less able to improve health. 23 November 2024 9
Hall and Jones (2007) also estimate the marginal cost of saving a life and the marginal cost per life saved for these groups (Figure 3.2) Cost per life saved is highest for young groups, then falling steadily up to the oldest group. Comparison across years shows a 4.7% rate of growth in cost of a life saved. 23 November 2024 10
3.1 The Productivity of Medical Care Evidence on Aggregate Productivity of Medical Care Cost per life-year saved shows a similar pattern up to the oldest groups. Falls to $48,000 by age 50-54, and then climbs rapidly to $500,000 for the 90-94 age group. Where is a reasonable cutoff for decision-making? Medical literature has suggested $50,000. More recently discussions suggest $100,000. Braithwaite et al (2008) used two approaches, giving base-case estimates between $183,000 and $264,000, which correspond well with the willingness-to- pay estimated in the Hall and Jones research. 23 November 2024 11
3.1 The Productivity of Medical Care Evidence on Aggregate Productivity of Medical Care Randomized Controlled Trial Data: RAND HIS Results from social science experiments using standard statistical techniques. Rand Health Insurance Study (RAND HIS) began in 1974. Examined the relationship between insurance coverage and health care use. Examined the resultant effects on health care outcomes. Four cities, two rural sites, 20,000 person-years of data (some enrolled for 3 years, some for 5) Randomly assigned to insurance plans, one which had full coverage, others with copays. By varying the price of health care, can observe differences in medical care choices, and thus the effect of those choices on health outcomes. 23 November 2024 12
3.1 The Productivity of Medical Care Randomized Controlled Trial Data: RAND HIS Three health outcome measures: Questionnaires on activities of daily living (ADL), self-perceived health status, mental well-being, and other self-reported health measures. Data on sick-loss days (from work, school, etc.) Physical examination at end of experiment on conditions that the health care system should be able to affect (weight, blood pressure, cholesterol, etc.) Measures collected statistically into a measure of health-status age, a physiological measure that reports the apparent age of people s bodies. Should age by a year for each year enrollees are in the study Large sample, so should be possible to detect small changes 23 November 2024 13
3.1 The Productivity of Medical Care Randomized Controlled Trial Data: RAND HIS What health differences occurred between the groups? Low coverage group used about 2/3 of the medical care used by the full coverage group Not much difference in health, except for: Low-income, full coverage group had better corrected vision. Same group had lower blood pressure (important because reduces risk of death in high risk groups) Problems with the study include short time horizon and potential lack of power to detect true effects (because the sample contained only 5,800 people) 23 November 2024 14
3.1 The Productivity of Medical Care Evidence on Productivity of Specific Treatments Randomized Controlled Trials (RCT) Best studies can provide information on consequences of extending treatments on either the intensive or extensive margins. Example: Table 3.1 (following slide) show the incremental cost-effectiveness (CE) ratios for a series of interventions. Comparison across target populations examines the extensive margin Changing the rate of use within a population examines the intensive margin Higher CE ratio signals a lower marginal productivity because cost remains same no matter what the population treated Similar patterns for most treatments: In highest-risk populations, marginal product is high, and CE ratio is low. As populations become less risky, marginal product falls and the CE ratio rises. 23 November 2024 15
Similarly, the studies show changes along the intensive margin. Increasing frequency of PAP smears to two years, as compared to three years, hugely increases the CE ratio. New approaches compare the procedures used and their costs in treating a specific medical condition and investigates how these cost have changed over time. Example: Cutler et al, 1998, measures costs and outcomes for treating heart attacks, found that costs increased by $10,000, but life expectancy increased by a year, giving a cost per life-year of $10,000. 23 November 2024 16
3.1 The Productivity of Medical Care Evidence on Productivity of Specific Treatments More Finely Grained Outcome Measures Most studies consider life expectancy as the outcome but do not consider quality of life. Canadian system rations availability of treatments while U.S. system does not: what is the marginal value of these extra treatments? Focused on invasive treatment for heart disease (coronary bypass, etc.) Looked at mortality of the two populations. U.S. Medicare population received far more early treatment, which resulted in very small improvements 1 month out, but virtually no difference a year later. But this does not consider potentially important health improvements form the interventions. A year later, U.S. patients were less likely to have chest pain and shortness of breath, so their quality of life was better, something missed by looking only at mortality. 23 November 2024 17
3.1 The Productivity of Medical Care Evidence on Productivity of Specific Treatments Quality of Life Adjustment Many illnesses that are not necessarily life-threatening by are improved by medical intervention do not appear in mortality measures. Treatment of depression through medication Hip and knee replacements which improve mobility One approach uses the ratio of incremental costs to incremental effectiveness (ICER) with a quality of life-year adjustment (QALY) to measure bang for your buck. Quality adjustment requires evaluating the reduction in quality of life from each specific problem. E.g., if you were in perfect health, your score might be 100. If you were in perfect health EXCEPT blind, your score might be 60. Values obtained in a variety of subjective ways. 23 November 2024 18
3.1 The Productivity of Medical Care Evidence on Productivity of Specific Treatments Quality of Life Adjustment An alternate measure is disability-adjusted life-years (DALYs) Starts with the highest achievable life span , and subtracts losses from disease and disability (YLL = years of life lost) Years lost due to disability (YLD) is the product of years lived with disability (L) and a disability weight (DW) Weights determined by a panel of experts Different weights place on outcomes depending on the person s age (Table 3.2, next slide) Figure 3.3 (next slide) shows a typical age-weighting profile. 23 November 2024 19
3.1 The Productivity of Medical Care Quality of Life Adjustment 23 November 2024 20
3.2 Confusion About the Production Function: A Policy Dilemma The medical profession, both domestically and internationally, has strong internal disagreements about the marginal productivity of many medical procedures, particularly about the extensive margin. Medical Practice Variations on the Extensive Margin Studies focus on the rate at which standard populations have received specific medical interventions. Studies define a geographic area and look at rates at which a specific procedure has been used and their effect on hospital admissions. Coefficient of variation (COV) is the ratio of the standard deviation ( ) to the mean ( ). Larger COVs show greater variability relative to the mean. Studies show a surprisingly uniform picture of medical practice variations (Table 3.3, next slide) Procedures with large variations in one area will be likely to have large variations in others. Absolute variability differs between regions or countries, but relative variation is largely stable. 23 November 2024 21
3.2 Confusion About the Production Function: A Policy Dilemma 23 November 2024 22
3.2 Confusion About the Production Function: A Policy Dilemma Medical Practice Variations on the Extensive Margin, continued Wennberg et al., 1990, compared the use of various medical practices in Boston and New Haven. In both cities, nearly all hospitalizations occur at hospitals affiliated with medical schools. Cities otherwise very similar. Showed substantial variation in medical practice even within the academic community, which should be best informed Age-adjusted patterns of use uniformly higher in New Haven Large differences in certain minor surgery and some other categories Similarly large variations in admission rates for surgical procedures in a 16 hospital study (Table 3.4, next slide) As a rule of thumb, the ratio of highest to lowest rates of use will approximately correspond to 10 times the COV. 23 November 2024 23
3.3 Physician-Specific Variations (Medical Practice Styles) A statistical problem underlies all studies: large sample sizes are necessary to be statistically reliable, and thus patients (with a single illness) must be aggregated across regions. Requires the assumption that every region has the same age and gender composition. But to study individual physicians choices, this cannot be done because usually one doctor does not treat enough patients with the same illness. Newer methods have been developed to standardize an individual doctor s patient mix and thus estimate the medical costs in each practice (and estimate each doctor s style ). 23 November 2024 25
3.3 Physician-Specific Variations (Medical Practice Styles) A study used claims data from several hundred thousand patients in a Blue Cross and Blue Shield insurance plan that had no deductibles, and covered a wide array of inpatient and outpatient services (Phelps et al., 1994). Focused on the treatment patterns of primary care doctors because in this insurance plan, patients could not be treated without first seeing their primary care doctor. About 500 primary care doctors in the Rochester, New York, region. Analyzed the medical care use of individual patients in the Blue Choice plan, using two new methods to calculate the severity of illness that each patient had during the year. After controlling for the illness of each patient, the unexplained portion was averaged over each patient in each doctor s practice, and those average unexplained amounts provide an estimate of each doctor s style. 23 November 2024 26
3.3 Physician-Specific Variations (Medical Practice Styles) Figure 3.4: Distribution of primary care doctors practice styles in Rochester, New York. Score of zero: the doctor s style is at the average spending. Score of 0.1 means that the doctor s patients, on average, had 10 percent less medical care used for them than the overall average. Score of 0.2 means that those patients cost 20 percent more than average 23 November 2024 27
3.3 Physician-Specific Variations (Medical Practice Styles) On average, the lowest cost 10 percent of doctors used about half the medical care resources as the top 10 percent of the doctors. 23 November 2024 28
3.3 Physician-Specific Variations (Medical Practice Styles) Welch, Miller, and Welch (1994) used 1991 Medicare data, controlling for case mix, to profile 6,802 physicians from Florida and 1,101 from Oregon, selected from a larger group because they had at least ten Medicare hospital admissions during the year. Oregon: the mean relative value unit (RVU) per hospital admission was about 30 (equivalent to the work of 30 routine office visits), with a range from 10 to 70. Florida: mean RVU use in Florida was half again as large (46 RVU per admission). 23 November 2024 29
3.4 Extensive and Intensive Margin Differences: Are They Similar? Do regions (or doctors) that disagree about the extensive margin of care have related disagreements about the intensive margin of use? Studies are limited, but suggest that disagreements about extensive and intensive margins may be very different. The Policy Questions: What Should We Do About Variations? How do medical interventions become accepted as standard medical practice, and what causes the medical community to change its beliefs about therapeutic efficacy? What is the proper way to create and disseminate information about the efficacy of medical interventions their marginal productivity? These questions are considered in further chapters. One approach is to create guidelines for treatment strategies (physicians organizations, NIH consensus panels, patient outcome research teams) 23 November 2024 30