Understanding Dysphotopsia After Cataract Surgery
Dysphotopsia, a common issue post successful cataract surgery, can cause patients distress with unwanted images. Learn why patients complain, the nature of the problem, and how patient reactions play a significant role in resolving the issue. Recognize the visual symptoms patients experience and the importance of patient perception in managing dysphotopsia effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
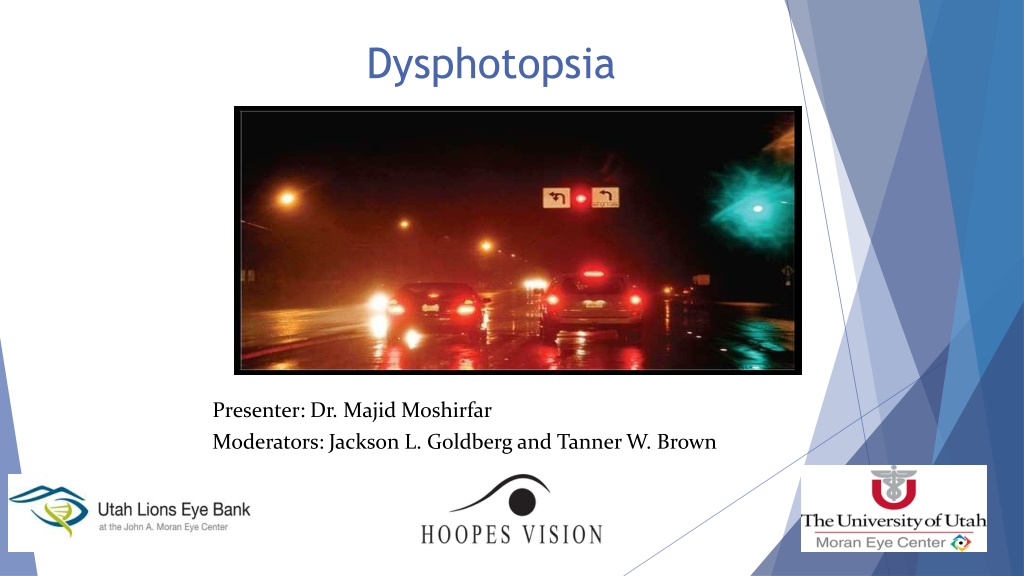
Dysphotopsia Presenter: Dr. Majid Moshirfar Moderators: Jackson L. Goldberg and Tanner W. Brown
Imagine This You've just performed successful, uncomplicated cataractsurgery Your patient is 20/20 and the surgery looksbeautiful You're ready to becongratulated
Instead, your patient says, "I hate it! These unwanted images are driving me crazy! You've got to do something about this
Of course, this isn't what you want to hear. But the reality is that dysphotopsia has become the number one problem following uncomplicated, successful cataract surgery. And it doesn't go away easily once a patient becomes focused on it.
Unfortunately, many of these patients are incredibly unhappy Most of whom are told that they're crazy Your surgery is perfect!" "There's nothing wrong here!" This has entirely the wrong effect, making the patient angrier and even more focused on the unwanted image
The Nature of the Problem The number of patients who actually require an intraocular lens exchange is only about 1 in a 1000 However, the number of patients complaining about dysphotopsia is closer to 1 in 10
So what's behind the current wave of dysphotopsia complaints? The first element is what the patient is actually seeing. The second element is how the patient reacts to the symptom The patient's reaction can be the most significant factor in resolving (or not resolving) the problem
What the Patient Sees Temporal darkness Arc Flare Central flash
In the literature, terms such as photopsias, entoptic phenomena photic phenomena have been used to describe these images. In June 2000, the term dysphotopsia was first used
Positive and Negative Dysphotopsia Positive dysphotopsia is usually related to bright artifacts of light on the retina Negative dysphotopsia is manifested by a dark crescent or curved shadow
The exact etiology of negative dysphotopsia remains an enigma The question of why this dark shadow of light occurs temporally Because the nasal retina may extend further anteriorly than the temporal retina as well as because light coming in nasally may be somewhat tempered by the nose, eyebrow and cheek
Continued However, light coming from the temporal side of the eye that projects to the nasal-most retina may be deflected by the edge of the IOL or even reflected internally by the relatively square edge of the IOL away from the nasal retina This results in a crescent-shaped shadow noted in the temporal field of vision
Temporal Darkness Temporal darkness, or negative dysphotopsia, is the most prevalent symptom today 30 to 40 %* In this case, the patient detects a black shadow temporally, in the periphery of vision *V mosi P, Cs k ny B, N meth J. Intraocular lens exchange in patients with negative dysphotopsia symptoms. J Cataract Refract Surg. 2010;36(3):418-24.
Arc Patient perceiving the edge of the IOL, which usually only happens at night It's a common complaint and rarely a serious problem It usually resolves over time especially if the capsule overlaps the IOL edge
Flare This is also a scotopic symptom produced by coma Correcting minimal cylinder with night driving glasses will often get rid of it Making the pupil a little smaller at night will also help
Central Flash This appears to be caused by a peripheral light source reflecting off the internal edge of theIOL Recent advances in edge design have minimized this symptom
Haloes These may be caused by a multifocal IOL. Produces haloes around lights from each ring transition zone. Most patients will adapt to this, and a smaller scotopic pupil can help in the meantime.
Night haloes are the number one reason these IOLs are explanted If patients see haloes with a monofocal IOL, it usually indicates the presence of spherical aberration New aspheric-optic IOLs will help
How the Patient Reacts Difficult to eliminate all unwanted images from patient's vision. The brain is adapt at eliminating unwanted visual input by phenomenon of central adaptation. the most obvious example is the hole in our visual field where the optic nerve enters the eye.
Physiology In addition, weget: front- and backscatter off our naturallens pupils are irregular blood vessels in ourretina that we can't seethrough There are a lot of unwanted images in our field of vision, but our brain adapts and eliminates themall
Managing Dysphotopsia It is inevitable that some patients will experience unwanted images In these cases, doing the right things before and after surgery can avoid the greaterproblem
Create Accurate Expectations Before Surgery Explain to patient about dysphotopsia preoperatively Then, the patient won't be surprised if some new, unwanted visual effect accompanies the new lens
Minimize the Problem Surgically Use the right lens Certain IOL characterstics appear to correlate with reduced dysphotopsia Newer lenses have helped by increasing the front curvature of the lens, which minimizes front and back light scattering
Optic size is important, because a smaller lens may create more edge problems D0n't implant a lens any smaller than 6 mm
All the IOLs studied variably increased internal and external surface reflections when compared to the human crystalline lens.
Square Edge Design While the square-edge optic is clearly favored for reducing the risk of PCO, the trade-off for that benefit is an increased rate of pseudophakic dysphotopsia
Pseudophakic Dysphotopsia Square-edged optic is one responsible factor causing dysphotopsia The other factors responsible are: the index of refraction of the IOL material corneal curvature pupil size
Truncated posterior edge offers barrier effect to lens epithelial cells Sloped edge-minimises internally reflected rays that form arc like images Rounded anterior edge- eliminates mirror effect
Continued.. Round edge of the optic causes greater dispersion of the internally reflected rays of light, reducing edge glare by 90% Increasing the front curvature of the newer lenses has helped minimize front and back light scattering, reducingglare
Double Square Edge When light hits the double-square edge lens at 23 degrees, little edge glare at 35 degrees, one begins to see arcs at 55 degrees, transmitted as well as reflected glare becomes significantly more evident
Continued. silicone lens with a rounded edge and lower refractive index seems to be most forgiving, producing the fewest complaints about unwanted images.
Place the lens carefully A well-centered, in-the-bag lens prevents unnecessary optical problems
Overlap the capsulorhexis rim over the edge of the lens The edge of the capsulorhexis will tend to opacify overtime The opaque overlap will eliminate many symptoms associated with the edge of theIOL The brain seems to ignore the edge of the capsule, reacting as it does to the edge of thepupil
Another Major Benefit This strategy has another major benefit If we overlap the capsule, we will significantly decrease posterior capsule opacification. Two recent studies, show that overlap of the capsule is more effective at preventing "after cataract" than switching to an IOL with a truncated edge
Continued Making a smaller capsulorhexis has some potential downsides It can be more difficult to access the lens, particularly if we use the Phaco technique Also, we don't want to risk capsular contracture by making the opening too small
Continued To minimize dysphotopsia and PCO, the opening should be roughly 1 mm smaller than the size ofthe optic, to ensure 360-degree overlap And use at least a 6-mmoptic
After surgery, don't take the wrong attitude if a patient complains The worst thing you can do if a patient complains is tosay, "Your result is perfect. Nobody else is complaining.What's your problem?" This virtually guarantees that the patient will "turn up the gain," and fail to adapt to the unwantedimages
Resolving a Dysphotopsia Crisis Talk to the patient (and say the right thing). First of all, let the patient know that he/she's not crazy. That alone will improve matters. Try night time pupil constriction
Don't Open the Capsule Whatever you do, don't open the capsule Some ophthalmologists, thinks maybe patient got after cataract. So let's go ahead and do a YAG capsulotomy and see if that will make it better If the problem truly is dysphotopsia, a capsulotomy won't have any positive effect at all
When we try to take the lens out after a YAG capsulotomy, vitreous comes forward. We often can't put the lens back in the capsule because the capsulotomy tears further. The risk of endophthalmitis and retinal detachment increase dramatically.
Lens Exchange? Only resort to lens exchange if it really makes sense First of all, make sure the patient has had enough time toadapt If even after six months problems continued then a lens exchange can be consider only if it improve on the existing lenssituation. Otherwise, switching lenses will be a waste of time
Factors Deciding Lens Exchange The size of the existing capsulorhexis If the optic is small then larger optic will create more overlap of the edge, this can solve problem Edge design If the current IOL doesn't have an up-to-date edge design, then switching to an updated lens wouldbe helpful
Refractive index If the current lens has a high refractive index, switching to a rounded-edge silicone lens may be curative, particularly if there is negative dysphotopsia. Condition of the capsule If another surgeon has performed a YAG capsulotomy, a lens exchange will involve more risk.
If All Else Fails For some patients, nothing will relieve the symptoms, and IOL exchange may not makesense if thepatient already has the most beneficial typeand size of IOL In thatcase, talk tothe patientagainand do bestto help him or her torelax And advise the patient to stop thinking about it so much, so the brain has a chance to adapt
Pseudophakic Dysphotopsia with Various Intraocular Lens One study was conducted on Pseudophakic Dysphotopsia with Various Intraocular Lens at Laxmi Eye Institute Highlights of study The incidence of dysphotopsia found to be 51.12% The incidence of negative dysphotopsia has been found to be 22.47% The eyes implanted with Tecnis ZCB00 IOL showed less negative temporal shadow/darkness Hydrophilic Acrylic IOLs showed greater dysphotopsia score in comparison to those with Silicone IOLs
Highlights Continued Hydrophilic versus Hydrophobic Acrylic, the latter was found to be significantly better with a lower dysphotopsia. Hydrophobic Acrylic IOLs when compared to Hydrophilic Acrylic IOLs and Silicone IOLs showed decrease in night-time glare/halo/circles An increase in the optic-haptic angle caused an increase in night-time glare/halos/circles around lights.
Conclusion Tecnis ZCB00 emerged as least troublesomelens While Auroflex FH5575 which was reported to have the highest Dysphotopsia Hence, we may conclude that different brands of intra-ocular lenses display varying degrees of dysphotopic symptoms
Recent Updates New hypothesis, resolution of negative dysphotopsia symptoms depended on intraocular lens (IOL) coverage of the anterior capsule edge rather than on collapse of the posterior chamberalone. Negative dysphotopsia was not attributed to a particular IOL material or edgedesign Pseudophakic negative dysphotopsia: Surgical management and new theory of etiologyJournal of Cataract & Refractive Surgery, 06/24/2011
New Concept Two rays, coming in from the temporal side at 90 , are bent by the cornea by about 45 As they come through, one ray, if there is a space between the iris and the anterior surface of the lens, can miss the front part of the lens According to Dr. Holladay, Hawaiian Eye meeting