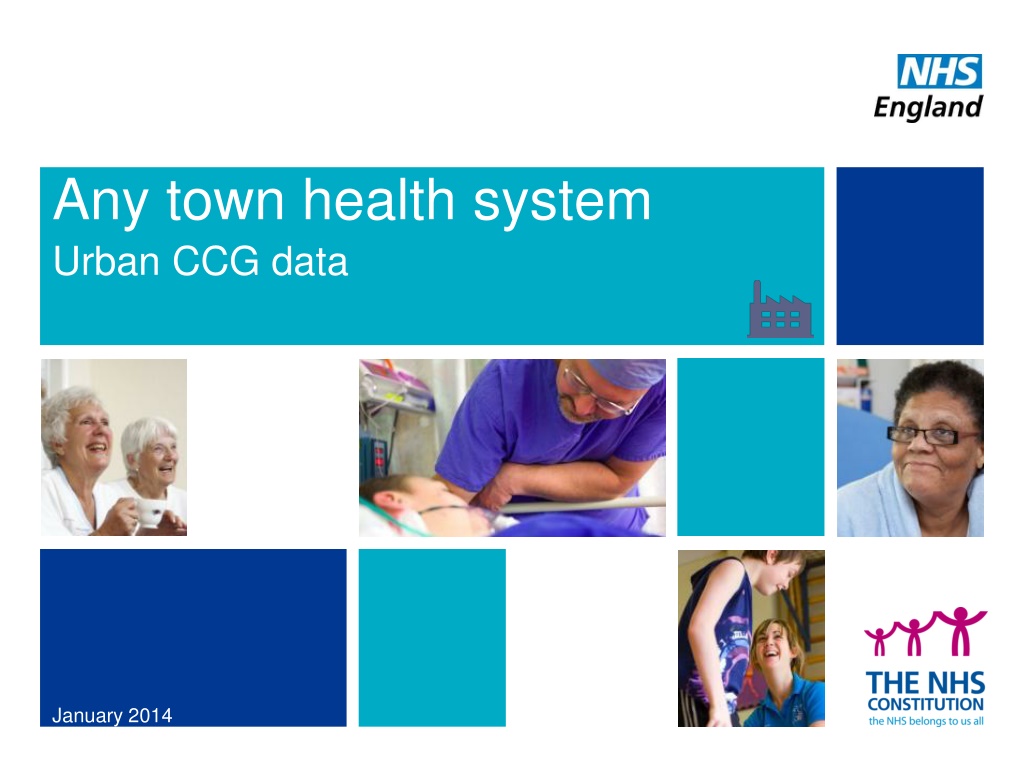
Understanding Any Town Health System Urban CCG Data
The Any Town Health System Urban CCG Data for January 2014 provides insights into interventions, scenario CCGs, and results in healthcare planning. It outlines a call to action by NHS England for strategic planning and highlights key questions. The report works on assumptions and aims to support local health economies in developing sustainable plans.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Any town health system Urban CCG data January 2014
The key questions What is Any town health system and how does it relate to a call to action? 1 What interventions are included in the report? 2 What are the three scenario CCGs and how do they differ? 3 What will the results look like? 4 How do I get started? 5 3
1 | A call to action The objectives of a call to action NHS England has set out a call to action to the public, patients, staff, and politicians to help the NHS meet current quality challenges, future demand and tackle the funding gap through honest and realistic debate. It sets out challenges facing the NHS and how we must change to overcome these challenges. The results of these call to action debates will be captured in five year strategic plans Health systems are asked to provide locally owned, outcome focused, sustainable plans, developed and co-signed in partnership with the wider health and social care economy that address the challenges identified in a call to action. This is a five year strategic planning exercise, within which is a two year detailed operational plan. What is Any town? Any town health system is an additional resource planners can refer to when developing their local strategic plans with the support and input from local communities. It is called Any town as the data is of interest to all health economies. It contains A set of evidence-based interventions that could be applied in a local health economy, some of which will also support BCF planning; A calculation of how quality and finance could be affected through the impact of the interventions, using the seven outcome ambition metrics as our marker for quality. What it isn t A collectively exhaustive list of interventions that fill the financial gap; A provider-side reconfiguration tool; A mandate to include these interventions in all strategic plans. Additional interventions In addition to the interventions included in Any town we have also found further interventions that we were unable to model at this stage but may provide additional resource for planners. These additional interventions are shared in the report and further information guide but the results shared should not be viewed as robust as the modelled interventions. Some of the interventions have been provided by Public Health England and we are grateful for their contribution. 4
1 | The report works on several assumptions To make projections over a five year period, the workings make various assumptions that support the estimates. These assumptions over inflation, productivity and demand will be subject to change over the time period and therefore the results are dependent upon the information available at the time of publication. In addition to these assumptions, we recognise that not all health economies are the same: Their demographic make-up and the prevalence of conditions among the population will vary considerably; and Some health economies may already have begun implementing some of the initiatives we have discussed. Furthermore, we recognise that implementing each of these interventions could pose a significant challenge. For all interventions included in the detailed model, the impact will be shown net of investment costs required for implementation, although it is noted this is often challenging to estimate from the literature. The actual impact in any local health economy will depend on: Their starting position in relation to the interventions described; How the interventions are implemented locally; and Other / existing interventions being implemented at the same time. T We recommend all health systems use the data provided in the reports with these caveats in mind and that appropriate local validation is undertaken prior to implementation decisions being made. 5
2 | The Any town health system interventions High impact interventions Early adopter interventions A set of evidence-based interventions that could be applied in a local health economy. Selected for their high impact and robust evidence of real-world impacts delivered. Promising ideas which may offer commissioners further benefits. They have not yet been widely adopted or fully impact assessed. Selection criteria: 1. Fully impact assessed for financial and quality impact. 2. Contribute to the financial and quality challenges articulated in this report. 3. Have a clear narrative to guide implementation. 4. Scalable across a broad population group. Selection criteria: 1. The intervention is innovative and cutting edge. 2. There are demonstrated quality impacts. 3. It appears likely to be either cost-neutral or cost-saving. 4. It has a clear narrative and is appropriate for wide scale adoption by commissioners. To select these interventions we have reviewed: Over 270 self-reported case studies of healthcare interventions currently being implemented by CCGs around the country. Over 100 additional examples of interventions provided by NHS stakeholders. Awide range of material from academic reviews and third sector organisations. 6
2 | The high impact interventions (HIIs) Early diagnosis Early detection and diagnosis to improve survival rates and lower overall treatment costs 1 Reducing variability within primary care by optimising medicines use and referring Reducing unwanted variation in primary care referring and prescribing 2 Self-management: Patient-carer communities Self-management programme for those suffering with a long-term condition 3 Telehealth/Telecare Health apps, telehealth and telecare equipment which help people to manage their own long term conditions in conjunction with their clinicians, introduced to empower people whilst at the same time ensure that their own actions remain embedded in the care they receive from the NHS 4 Case management and coordinated care Multi-disciplinary case management for the frail elderly and those suffering with a long-term condition 5 Mental Health Rapid Assessment Interface and Discharge (RAID) Psychiatric liaison services that provide mental health care to people being treated for physical health conditions 6 Dementia pathway Fully integrated network model to improve health outcomes and achieve efficiencies in dementia care 7 Palliative care Community based, consultant-led palliative care service 8 7
2 | The early adopter interventions (EAIs) Cancer screening programmes Early diagnosis of colorectal, breast and lung cancer to increase survival rates GP tele-consultation Systemic approach to tele-consultation in primary care, as a complement to practice-based consultations Medicines optimisation Pharmacist-led interventions to support optimal prescribing and use of medicines Safe and appropriate use of medicines Reducing the number of preventable deaths from medication-related incidents through Eclipse Live Acute visiting service Reducing demand for emergency care through providing a rapid-access doctor at home Reducing urgent care demand Acute GP unit to triage emergency arrivals; occupational therapists in A&E to reduce low-risk admissions 24-hour asthma services for children and young people Reducing unnecessary hospital admissions through a 24-hour home nursing service Service user network Mental health co-designed support service developed for and by people with emotional/behavioural problems Reducing elective caesarian sections Campaign for Normal Births to lower rate of unnecessary elective Caesarian sections 10 Acute stroke services Creating a hyper-acute stroke unit to optimise acute stroke services and ensure 24/7 access to specialist care 11 Integration of health and social care for older people Integrating care through organisational, procedural and cultural changes 12 Electronic palliative care coordination systems (EPaCCS) Improving care and helping patients to die in the location of their choice through a shared electronic record 1 2 3 4 5 6 7 8 9 8
2 | Additional ideas to be considered Following the HIIs and EAIs, there are several additional international case studies that could be implemented within a local health economy which may lead to quality improvements and cost savings. Further Ideas A set of programmes that, although not impacted assessed to the level of other interventions, could lead to improvements in a local health economy. Selected for their ambitious and aspirational nature, having not been widely adopted or implemented nationwide. The modelling of these ideas does not follow the same rigorous methodology as the HIIs and EAIs, with savings presented as gross savings, and should be viewed as indicative only. Selection criteria: 1. Aspirational in design and implementation. 2. Relevant to be implemented for a health economy, as well as open to further development and refinement. 3. Have some indication of financial and quality impacts. 9
2 | Further ideas Urgent and emergency care networks Regional networks of urgent and emergency care centres, consolidating specialist expertise onto fewer major centres 1 Elective specialty centres Centres of excellence for single specialties focusing on strong clinical outcomes and operations excellence 2 Wellness programmes Prevention programmes that incentivise healthy behaviours, improve quality of life, and reduce the overall cost of healthcare 3 Interoperability of systems and patient records * Interoperability of systems and patient records aims to break down the barriers between types of care, enabling presentation of patient information in a way that is accessible and cross-compatible for all those involved with patient care. 4 Public Health England case studies * Additional interventions received from Public Health England, covering a variety of conditions and points of delivery. 5 10 Notes: * Not quantified financially
3 | The three scenarios We know there is no such thing as an average CCG. To help understand the impact different interventions will have in different settings, we have created three scenarios, Urban CCG, Suburban CCG and Rural CCG. There is a version of Any town for each scenario. The impact of the interventions have been modelled for each scenario, allowing us to see how the results differ for different population groups. For some interventions the impact is broadly consistent but for others we have found differences in the impact assessment. In comparison to the weighted average CCG (by type) Suburban CCG Urban CCG Rural CCG Younger demographic than average Older demographic than average Same age demographic as average Lower prevalence of LTCs than average Average prevalence of LTCs compared with average Higher prevalence of LTCs than average Higher levels of deprivation than average Higher levels of deprivation than average Higher levels of deprivation than average 11
4 | What will the results look like? Urban CCG We will label the pages clearly to illustrate which scenario the results relate to. Interventions: Quality Benefits Interventions: Financial Benefits The three scenarios intend to show both the quality and financial impact of implementing the interventions. Impact on Quality Ambitions Intervention Net benefit Early Diagnosis 0.7m Ambition 1 Qualitative evidence Reducing variability within primary care 4.8m 7.9% improvement in QoL Ambition 2 Self-Management: Patient- Carer Communities 0.9m The impact will be based on the characteristics identified of each scenario (Population size, disease prevalence etc.). 6.6% improvement in ACS admissions Ambition 3 Telehealth / Telecare 0.7m Case Management and Coordinated Care 2.9m 41.2% improvement in 91day rehab. Ambition 4 Mental Health Rapid Assessment Interface and Discharge 1.5m Ambition 5 Qualitative evidence Additional analysis will show the results visually and in more depth. Dementia Pathway 0.4m Palliative Care 1.0m Ambition 7 - Overlap ( 1.3m) Total: Quantified benefit for 3/6 Ambitions & Qualitative benefit for 5/6 CCGs will need to adapt the impact assessment to suit their own local demographics. We would recommend further local analysis occurs before any decision are taken at local level regarding implementation. Total net benefit 11.7m The report will show the impact the interventions have on the seven quality ambitions. This will be both quantitative impact and qualitative impact. Commissioners will be able to see results from the ambitions interventions view. The report will show the impact the interventions have on the financial challenge. The impact will be shown net of investment costs required for implementation, although it is noted this is often challenging to estimate from the literature. An overlap has been created to eliminate double counting. 12 view or the
5 | How do I get started? 3 1 2 Refer to the further information guide Interrogate the results Select a scenario 1. Select one of the three scenarios to view the results of the impact assessments: - Urban CCG; - Suburban CCG; - Rural CCG. 2. The results will show the cumulative and individual impact of the interventions on both quality and financial metrics. This will allow readers to interrogate the appropriateness of individual interventions. 3. Should you wish to learn more on a particular intervention, a further information guide is available that contains case studies for these interventions but also additional interventions identified that have not yet been fully impact assessed. Additional interventions have also been provided by Public Health England and we are grateful for these contributions. 4. Additional resources are also available from NICE. NICE provides support for the commissioning process by providing access to all its guidance and standards in a Pathway format: http://pathways.nice.org.uk NICE also collates specific disinvestment suggestions from across the NHS, which are available at www.evidence.nhs.uk/qipp. 13
Navigation home Urban CCG Show me what an Urban CCG means: What demographics were used? Show me the methodology: A pack explaining the methodology is available. It is called Any town methodology module. What does the age profile look like? What difference in disease prevalence is there? Show me results: What impact do the interventions have on the seven outcome ambitions? What are the seven ambitions? What is the ambition do nothing baseline for 18/19? Show me where I can find more: A separate pack providing details of the case studies used further information is available. It is called Further Information. Which interventions impact which ambition? What impact do the interventions have on the financial baseline? What is the financial do nothing baseline for 18/19? Which interventions have the biggest financial impact? What does the financial bridge chart look like? What impact is there on activity across the provider setting? If fully implemented, how would activity change? If viewing this as a presentation, all questions that are underlined can be jumped to by clicking on the question. To return to this page, please click on the icon below How difficult is it to implement these interventions? How deliverable are the interventions? 15
Demographic comparison Urban CCG The Any town urban system is broadly representative of an average urban health economy. Where there are slight differences, the interventions will be correspondingly biased towards this demographic make-up. These factors will impact which suite of interventions will have the largest impact on the Any town urban system. Younger demographic Interventions focusing on the frail/elderly and LTCs could have less of an impact here. CCGs must also consider the effect of service utilisation across various settings of care. Lower prevalence of LTCs Higher levels of deprivation In comparison to the weighted average urban CCG. 17
Demographics age profile Urban CCG The Any town urban system has a slightly younger demographic compared to the weighted average urban CCG. Interventions focusing on the frail elderly could have a smaller impact here compared to locations with older demographics. However, the impact of other factors (e.g., per capita service usage) will modulate the effect of demographics alone. Urban CCG Population age breakdown, Any town urban system vs. All urban CCGs, Mid-2012 The Any town urban system appears to consist of a slightly younger demographic compared to a weighted average urban CCG, with: 27,046,552 100.0% 7.2% 9.6% 70+ A proportionally higher amount of the population in the 20-49 age category; and 16.5% 20.4% 50-69 75.0% A proportionally lower amount of the population in the 50-69 and 70+ category. This will impact which suite of interventions will have the biggest quality and financial impact on the Any town urban system, with those interventions focusing on the frail elderly population having less of an impact here. 51.9% 50.0% 46.2% 20-49 25.0% CCGs must also consider the effect of service utilisation across various settings of care. 24.5% 23.8% 0-19 0.0% Any town Urban CCG All "Urban" CCGs 18
Demographics prevalence rates Urban CCG The Any town urban system has a lower prevalence of many LTCs compared with all urban CCGs. It has a higher prevalence of COPD, mental health and depression. Urban CCG Prevalence rates, Any town health system vs. All Urban CCGs, 2010 CHD CVD HF Hyper- tension Stroke Obesity Diabetes CKD COPD Asthma Cancer Mental Health Depre- ssion Dementia LD Any town urban system All Urban CCGs 3.1% 1.2% 0.7% 12.7% 1.5% 10.7% 5.7% 3.8% 1.6% 5.6% 1.4% 0.9% 10.1% 0.4% 0.4% The Any town urban system has lower prevalence rates (compared to all urban CCGs) for CHD, HF, Hypertension, Stroke, Obesity, CKD, Cancer and Dementia. Conversely it has a higher prevalence in COPD, Mental Health and Depression. Interventions that focus on respiratory conditions, mental health and depression are expected to have a bigger impact in this location. 5% higher than all urban CCGs 5% c.f. all urban CCGs 5% lower than all urban CCGs 19 Source: NHS indicator tool.
Ambitions and quality indicators Urban CCG Quality indicators are mapped to levels of ambition against which the impact of an intervention is measured: Ambition 1 Ambition 2 Ambition 3 Ambition 4 Ambition 5 Ambition 6 Ambition 7 Securing additional years of life for the people of England with treatable conditions Improving health related quality of life of the 15 million+ people with one or more long-term condition Reducing the amount of time people spend avoidably in hospital Increasing the proportion of older people living independently at home following discharge from hospital Increasing the number of people having a positive experience of hospital care Increasing the number of people having a positive experience of care outside hospital Making significant progress towards eliminating avoidable deaths in our hospitals 1.1 Potential years of life lost (PYLL) from causes considered amenable to healthcare. 2 Health-related quality of life for people with long- term conditions. 2.6 Unplanned hospitalisation for chronic ambulatory care sensitive conditions. 2B (OF) [Proxy] Proportion of older people who were still at home 91 days after hospital discharge into rehab services. 4.b Patient experience of hospital care. 4a.i Patient experience of GP services. 5c Hospital deaths attributable to problems in care. 2.7 Unplanned hospitalisation for asthma, diabetes and epilepsy in under 19s. 4a.ii Patient experience of GP out of hours services. 3.1 Emergency admissions for acute conditions that should not usually require admission. 4a.iii Patient experience of dental services (national only). Captured in Direct Commissioning (not Any town health system) 3.4 Emergency admissions for children with lower respiratory tract infections. 21 Note: Indicator numbers refer to CCG, not NHS Outcomes Framework indicators, except where noted.
The Do Nothing scenario to FY 18/19 Urban CCG If no transformative action is taken, it is expected that health economies will endeavour to maintain constant quality standards by increasing their financial shortfall. In FY 2018/19, under a do nothing medium scenario, the urban Any town health system will face a financial gap of 40.8m. Quality baseline Financial gap pre-interventions Figures projected, in m Do Nothing scenario assumes that the quality of the NHS services is prioritised, and so remains effectively constant. 390 Financial resources Do Nothing expenditure - worst ( 60.3m) 380 Do Nothing exp. - mid ( 40.8m) 370 40.8 Do Nothing exp. - best ( 17.3m) Maintaining quality without intervention will result in increasing financial shortfall. 360 350 340 The Do Nothing scenario is therefore considered unsustainable in the long term. 330 320 310 The high impact intervention is modelled against this Do Nothing scenario. 0 2013/14 2014/15 2015/16 2016/17 2017/18 2018/19 22
The quality impact of the interventions Urban CCG Suspected benefit Qualitative benefit Some quantified benefit Strong quantified benefit Strength of quality benefit: Ambition 1 Ambition 2 Ambition 3 Ambition 4 Ambition 5 Ambition 7 High Impact 1. Early Diagnosis 2. Primary Care 3. Self-help 4. Telecare 5. Case Management 6. Mental Health 7. Dementia 8. Palliative Care Early Adopters 1. Cancer screening 2. GP teleconsultation 3a. Norfolk Med. Opt. 3b. PINCER 4. EclipseLive 5. AVS 6. Reducing urgent care demand 7. Asthma services 8. SUN 9. Reducing elective Caesarean sections 10. Acute Stroke 11. Torbay 12. EPaCCS 23 Notes: Ambitions: (1)Secure additional years of life; (2) Increase QoL for People with Long-Term Conditions; (3) Reduce unnecessary time spent in hospital; (4) Increase the proportion of older people living independently following discharge; (5) Reduce poor hospital care feedback; (7) Significantly reduce hospital avoidable deaths
Impact of all interventions on ambitions (1/2) Urban CCG The combined impact of HIIs and EAIs on indicator projections is represented as follows: 1.1 Potential years of life lost from causes considered amenable to healthcare - Adults 2,500 2,177.0 Ambition 1 Securing additional years of life for the people of England with treatable conditions 1,878.0 84.5 DSR per 100k 63.9 2,000 1,729.6 1,500 7.9% decrease in potential years of life lost. 1,000 500 0 5-year base line to date Cancer Services Acute Stroke Post-Ints FY 18/19 Do Nothing FY 18/19 2 Average health status score for individuals aged 18 and over with a LTC 0.8 0.7 0.7 0.8 0.1 0.0 Ambition 2 Improving the health related quality of life of the 15 million+ people with one or more long-term condition 0.6 7.9% increase in average health status of individuals with a LTC. EQ-5D 0.4 0.2 0.0 LA Dementia Pathways Self-mngt Post-Ints FY 18/19 Do Nothing FY 18/19 FY 12/13 2B Proportion of older people still at home 91 days after discharge from hospital into rehabilitation services 74.2 Ambition 4 80 3.9 57.1 57.1 Increasing the proportion of older people living independently at home following discharge from hospital 13.2 60 30.0% improvement in proportion of elderly people still at home (not readmitted) over 5 years. % 40 20 0 CCG FY 11/12 Case Mgmt Mental Health Post-Ints FY 18/19 Do Nothing FY 18/19 Notes: DSR = Directly Age-Standardized Rate; EQ-5D = Standardized EuroQol score measuring of patient health-related quality of life across five dimensions. 24
Impact of all interventions on ambitions (2/2) Urban CCG The combined impact of HIIs and EAIs on indicator projections is represented as follows: 2.6 Unplanned hospitalisation for chronic ambulatory care sensitive conditions 790.8 72.2 777.9 800 98.4 700 26.4 593.8 600 DSR per 100k Ambition 3 Reducing the amount of time people spend avoidably in hospital 500 24.9% decrease in unplanned hospitalisation for chronic ambulatory care sensitive conditions. 400 300 200 100 0 CCG FY 11/12 Appropriate/ safe meds use Acute visiting service Telecare Post-Ints FY 18/19 Do Nothing FY 18/19 2.7 Unplanned hospitalisation for asthma, diabetes and epilepsy in under 19s 350 312.8 314.1 35.0 300 155.5 250 DSR per 100k 60.6% decrease in unplanned hospitalisation for asthma, diabetes and epilepsy. Ambition 3 Reducing the amount of time people spend avoidably in hospital 200 150 123.7 100 50 0 CCG FY 11/12 Appropriate/ safe meds use 24-hr Asthma services Post-Ints FY 18/19 Do Nothing FY 18/19 25 Notes: DSR = Directly Age-Standardized Rate
Quality impact of further ideas Urban CCG The further ideas all show promising signs for benefits around clinical quality and patient experience. Whilst the evidence base is not as comprehensive as the HIIs and EAIs, some benefits have been highlighted below 41%complaints 15%waiting times Urgent and emergency care networks 1 post-surgery complications longer lasting joints waiting times Elective specialty centres 2 smoking cessation physical activity nutrition Wellness programmes 3 patient safety Interoperability of systems and patient records 4 Public Health England case studies 5 Various quality benefits please refer to the Further Information guide for greater detail. 26
Impact of the HIIs and EAIs on the financial challenge In 2018/19, under a Do Nothing medium scenario, the suburban Any town health system will face a financial gap of 40.8m. After the HIIs, this gap is narrowed by an estimated 11.7m (28.8% of the total gap), while after the HIIs and EAIs this gap is narrowed by an estimated 23m (56% of the gap). HIIs: Financial benefits EAIs: Financial benefits Intervention Cancer screening programmes Net benefit Intervention Net benefit 0.2m Early diagnosis 0.7m GP Tele-consultation Reducing variability within primary care 1.7m 4.8m Medicines optimisation 0.7m Self-Management: Patient- Carer Communities 0.9m Safe and appropriate use of medicines Acute visiting service Reducing pressure on urgent care 24-hour asthma services for children and young people*** 4.6m Telehealth / Telecare 1.8m 0.7m Case management and coordinated care 0.7m 2.9m 0.0m Mental Health Rapid Assessment Interface and Discharge 1.5m Service user network 0.6m Reducing elective caesarean sections Dementia pathways 0.4m 0.1m Acute stroke services** 0.0m Palliative care 1.0m Integration of health and social care for older people Overlap* ( 1.3m) 0.3m Total net benefit 11.7m ePaCCS 0.9m Overlap* ( 0.4m) Total net benefit 11.3m Notes: * The estimated activity changes and financial savings account for interactions and overlaps within the HIIs and the EAIs However, these do not fully account for the interaction between the HIIs and the EAIs. ** The Acute stroke services intervention has been assumed to be cost neutral. *** The impact of the intervention is negligible because it affects a relatively small population sub group (long term condition children). 28
Financial bridge of 2018/19 (1/3) Urban CCG After accounting for the on-going costs of implementing the interventions, the net savings generated by HIIs are 11.7m. This implies that, overall, the HIIs reduce approximately 28.8% of the financial gap. Move to page 2 of 3 HIIs Remaining gap to be filled through EAIs and international case studies 40.8 (100.0%) - 0.7 (1.8%) 45 - 4.8 (11.8%) Financial Gap (Figures in m) - 0.9 (2.1%) 40 - 0.7 (1.8%) - 2.9 (7.1%) - 1.5 (3.7%) 35 - 0.4 (0.9%) 1.3 (-3.1%) 29.1 (71.2%) - 1.0 (2.6%) 30 25 20 15 10 5 0 Dementia Pathway Overlap 2018/19 Post-interventions gap Mental Health (RAID) Tele-care Case Management Do Nothing 2018/19 baseline gap Palliative Care Early Diagnosis Patient-Carer Communities Reducing Variability in Primary Care 29
Financial bridge of 2018/19 (2/3) Urban CCG After accounting for the on-going costs of implementing the EAIs, the estimated net savings are an additional 11.3m. This implies that the HIIs and the EAIs together reduce the gap by c.56%.* Move to page 3 of 3 40.8 (100.0%) - 11.7 (28.8%) 45 EAIs Residual gap may be filled through looking at international examples 40 Financial Gap (Figures in m) 35 29.1 (71.2%) 30 - 0.2 (0.5%) - 1.8 (4.3%) - 1.7 (4.3%) 25 - 0.7 (1.8%) - 0.7 (1.8%) - 0.6 (1.5%) - 0.1 (0.2%) - 0.3 (0.6%) - 0.9 (2.1%) 0.4 (-0.9%) 20 - 4.6 (11.3%) See** See*** 13.8 (33.9%) 15 - 4.0 (-9.8%) 10 5 - 21.6 0 - 11.3 -5 0.0 -10 Residual gap Medicines Optimisation Acute Stroke Services*** EPaCCS Do Nothing 2018/19 baseline Stretch EAIs ***** Post HII Interventions gap GP Teleconsulation Cancer Screening Acute Visiting Service International examples to fill residual gap FY 18/19 Post-changes Reducing Urgent Care Pressure 24-hour Asthma Services** Service User Network Safe Use of Medicines Reducing Elective Caesarians Integration of Social Care**** Additional local QIPP Overlap within EAIs High Impact Interventions Notes: * The estimated activity changes and financial savings account for interactions and overlaps within the HIIs and the EAIs However, these do not fully account for the interaction between the HIIs and the EAIs. ** The financial benefits of 24-hout asthma services are less than 100,000. *** The Acute stroke services intervention has been assumed to be cost neutral. **** The full effects of this intervention would not be realised until 2019/20. For illustrative purposes, in the figure above the net savings from this intervention have been assumed to start in 2018/19. ***** Includes expansion of patient populations covered by EAIs. 30
Financial bridge 2018/19 (3/3) Urban CCG The HIIs and the EAIs together reduce the gap by 56%. We have estimated the impact of international examples and further ideas to help close the financial gap Return to page 1 of 3 Estimated savings Senior clinicians in the emergency department c. 6.2m Urgent and emergency care networks 1 Orthopaedics, heart surgery, maternity, cataracts c. 5.0m Elective specialty centres 2 Vitality programmes, Partnerships for Older People s Project c. 10.4m Wellness programmes 3 Interoperability of systems and patient records 4 Various programmes with some evidence of financial benefits please refer to the further information guide Public Health England case studies 5 Various programmes with some evidence of financial benefits please refer to the further information guide Note: Transformative changes have been largely calculated by applying the healthcare savings described in the evidence base to the healthcare expenditure for each CCG, segmented where appropriate into population sub-groups and points of delivery for each CCG. Savings are gross, with no non-recurrent or recurrent costs modelled. Not all transformative changes have been modelled due to data limitations within the evidence base. 31
Selecting interventions to implement (1): HIIs To aid with the prioritisation of interventions we have assessed the High Impact Interventions for their relative quality benefits and financial savings, as well as deliverability and scalability. Intervention Relative benefits Implementation Quality Ambitions Financial Savings Deliverability Scalability 1: Qual. 2: Qual. 3: Qual. Scalable across many conditions (e.g., diabetes, cancers). Applicable across geographies. 1. Early diagnosis 0.7m Taken from a small-scale local study. Buy-in across GP community may be challenging. Applicable across geographies. 2. Reducing variability within primary care 4.8m 4: Qual. Scalable across a wide range of low / medium-risk chronic conditions. Easily applicable across any geography. 3. Self-Management: patient- carer communities 0.9m 2: 7.7% Scalability dependent on technology / service. Potential for wide scalability, and most effective when deployed at scale. 1: Qual. 2: Qual. 3: 6.5% 4. Telehealth/telecare 0.7m 5. Case management and coordinated care 2: Qual. 3: Qual. 4: 23.2% Scalable across many chronic conditions and care for frail / elderly patients. Applicable across geographies. 2.9m 6. Mental Health Rapid Assessment Interface and Discharge (RAID) 2: Qual. 4: 6.8% 5: Qual. Only relevant for mental health patients, but applicable across geographies. 1.5m 2: 0.2% 4: Qual. 5: Qual. Only relevant for dementia patients, but applicable across geographies. 7. Dementia Pathway 0.4m 2: Qual. 3: Qual. 5: Qual. Only relevant for end-of-life patients, but applicable across geographies. 8. Palliative care 1.1m Notes: Ambitions: (1)Secure additional years of life; (2) Increase QoL for People with Long-Term Conditions; (3) Reduce unnecessary time spent in hospital; (4) Increase the proportion of older people living independently following discharge; (5) Reduce poor hospital care feedback; (7) Significantly reduce hospital avoidable deaths. Where financial, savings are shown as 0 this is due to rounding. Key financial savings 0 0-0.5m 0.5-1m 1-1.5m 1.5m+ Key quality impacts and deliverability Very low Low Medium High Very high 33
Selecting interventions to implement (2): EAIs Intervention Relative benefits Implementation Quality ambitions Financial savings Deliverability Scalability Scalable across a range of cancers. Applicable across all geographies. 0.2m 1. Cancer screening programmes 1: 4.5% 1.7m 2. GP tele-consultation Scalable across all primary care practices in any geography. 3. Qual. Scalable across a wide range of conditions. Applicable across all geographies. 2: Qual. 3: Qual. 0.7m 3. Medicines optimisation 4. Safe and appropriate use of medicines Potential for wide scalability, dependent on adoption of technology. Applicable across al geographies. 3: 9.1% 13.7% 4.6m Potentially applicable to a wide range of urgent care patients. Applicable across all geographies. 1.8m 5. Acute visiting service 3:13.7% Scalable across acute providers in a wide range of geographies. Applicable across multiple patient groups. 0.7m 6. Reducing urgent care demand 3. Qual. Relevant only for children and young people with severe asthma (previously requiring hospitalisation). Applicable across all geographies. 2: Qual. 3: 77% 5: Qual. 7. 24-hour asthma services for children and young people 0.0m Relevant only for mental health patients. Applicable across all geographies, but may have more impact in urban areas. 0.6m 8. Service user network 2: Qual. 9. Reducing elective caesarean sections Relevant only for maternity patients, but scalable across a wide range of geographies in select provider Trusts. 0.1m 1: 3.4% 5: Qual. 6: Qual. 2: Qual. 3: Qual. 4: Qual. 5: Qual. Relevant only for stroke patients. Applicable across urban areas and conurbations. 0.00m 10. Acute stroke services Primarily relevant for services for older patients, but potentially scalable across the wider health economy. Applicable across all geographies. 11. Integration of Health and Social Care for Older People 0.3m Relevant only to end of life care. Dependent on adoption of appropriate technology platforms. Applicable across all geographies. 12. EPaCCS 34 4: Qual. 5: Qual. 0.9m Notes: EAI4 impacts two indicators within Ambition 3
How will activity change if the interventions are implemented? 35
Activity impact on acute sector post HIIs and EAIs When implemented together, the HII and EAIs translate into the following percentage changes in activity by point of delivery within secondary care. 0.0% -20.2% -22.6% -21.3% -27.4% -16.4% 115% 115% 114% 114% 112% 112% 112% 100% 100% 100% 100% 100% 100% 91% 93% Relative changes in activity 88% 88% 81% A&E Outpatients 1st Outpatients follow-up Inpatients emergency Inpatients elective Inpatients maternity The HIIs and EAIs collectively impact activity within inpatients emergency, inpatients elective and A&E the most with 22.6%, 27.4% and 20.2% reductions respectively. 2013/14 2018/19 - Do Nothing 2018/19 - Post-intervention We also show the relative change from the 2013/13 baseline to 2018/19 post-interventions. This chart does not show the alternative provision required to implement the activity changes highlighted above 36 Whilst this work shows the high-level impact on the acute sector, we have not set out to understand the full impact, including the provider level of efficiency required in the sector.
Gross expenditure impact post HIIs and EAIs When implemented together, the HII and EAIs translate into the following percentage changes in gross expenditure by setting of care -5% 128% Relative changes in gross expenditure +4% -24% 121% 121% 116% 116% 100% 100% 100% 88% Secondary care Primary care (relating to CCG spend) Community care To facilitate the change in activity from the acute sector, alternative provision is required in primary care, community care and increased self-management. 2013/14 2018/19 - Do nothing 2018/19 - Post-intervention The chart above illustrates gross expenditure impact in different settings based on 13/14 expenditure levels and the two scenarios of do nothing and post interventions being implemented. The reduction in primary care expenditure (relating to CCG budgets only, not direct commissioning) is driven by the reductions in prescribing expenditure delivered by the interventions. 37
Glossary 38
Glossary Ambulatory Care Sensitive ACS Better Care Fund BCF Clinical Commissioning Group CCG Coronary Heart Disease CHD Chronic Kidney Disease CKD Chronic Obstructive Pulmonary Disease COPD Directly Age-Standardized Rate DSR Early Adopter Intervention EAI Electronic palliative care coordination systems EPaCCS Standardized EuroQol score measuring of patient health-related quality of life across five dimensions EQ5D Financial Year FY Heart Failure HF High Impact Intervention HII Long term condition, e.g., asthma, diabetes LTC National Institute of Clinical Excellence NICE Potential Years of Life Lost PYLL Quality of Life QoL Rapid Assessment Interface and Discharge (psychiatric liaison service) RAID 39