Understanding Allergies in Today's Society
Allergy is a prevalent health issue affecting a significant portion of the global population due to various factors like environmental changes, lifestyle choices, and genetic predispositions. The rise of allergic diseases, such as allergic rhinitis, conjunctivitis, and dermatitis, poses a challenge to human health in the 21st century. By exploring the different types of allergies and their symptoms, we can gain insight into the impact of allergens on our well-being.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
ALLERGY IS A SITUATION FOR HUMANITY FOR ITS INABILITY This disease is one of the most common on Earth. According to statistics, already today every fifth inhabitant of our planet suffers: every sixth American, every fourth German, from 5 to 30% of Ukrainian. And if the XX century was the century of cardiovascular diseases, then the XXI is predicted by WHO to become a century of allergy. This is facilitated by the following factors: - increased allergenic load on a person, - change its ability to respond to this load. The deteriorating ecological situation and, as a result, increased permeability for allergens of barrier tissues, inadequate nutrition, inadequate drug therapy, uncontrolled use of antibiotics, increased stress loads, sedentary lifestyle, changes in climate lead to the fact that the susceptibility of the human body to allergens, even those , which have always existed, is significantly increased. 2
In accordance with the definition of the concept of allergy, the group of allergic diseases includes such diseases, the mechanism of damaging action in which is associated with immediate-type hypersensitivity (ITH), delayed type hypersensitivity (DTH), or combinations thereof. In the group of ITH (IgE-reactive) are the following diseases: atopic bronchial asthma, infectious-allergic bronchial asthma in children, anaphylactic shock, hay fever, urticaria, Quincke's edema, allergic rhinitis and conjunctivitis, a significant part of the drug and food allergies. The group of DTH (Th1-reactin) includes: allergic contact dermatitis, infectious-allergic bronchial asthma in adults, some forms of drug and food allergies; HRT-mediated granulomatous processes: leprosy, tuberculosis, brucellosis, tularemia, iersiniosis, pseudotuberculosis, sarcoidosis, Crohn's disease, leishmaniasis.
topic dermatitis - a chronic allergic skin disease, the development of which is associated with both hereditary predisposition and the impact of a number of unfavorable environmental factors
Allergic rhinitis Allergic rhinitis is characterized by watery discharge from the nose, difficulty in nasal breathing, sneezing, itching in the nose, decreased sense of smell
Allergic conjunctivitis The main manifestations of allergic conjunctivitis include itching in the eye area, a feeling of "sand" in the eyes, lacrimation, photophobia, burning eyes, redness and swelling of the eyelids
Pollinosis The name "pollinosis" comes from the Latin word pollen - pollen, as the disease causes pollen of plants. Once, hay fever was called hay fever, believing that the cause of the disease is hay
Hives, urticaria This appearance on the skin of blisters of different sizes, similar to rashes after nettle burn, accompanied by skin itching
Food allergy People with food allergies experience a worsening of their well-being after eating certain foods that others do not cause negative reactions
Immunogenetic studies have brought the base under a hereditary predisposition to allergic diseases (atopy). The existence of a genetic system of non-specific regulation of the level of IgE, carried out by the genes of the excess immune response by Ih- genes (immune hyperresponse) is proved. These genes are associated with antigens of the main histocompatibility complex A1, A3, B7, B8, Dw2, Dw3 and a high IgE level is associated with haplotypes A3, B7, Dw2 (Marsh D.C. et al., 1982). There is evidence of a predisposition to specific allergic diseases, and this predisposition is supervised by different antigens of the HLA system, depending on nationality. So, for example, a high predisposition to pollinosis in Europeans is associated with the antigen HLA-B12; the Kazakhs - with HLA-DR7; among Azerbaijanis - with HLA-B21 (Balabolkin, 1998). At the same time, immunogenetic studies in allergic diseases can not yet be concrete guidelines for clinicians and require further development.
"As with other types of allergies, with food allergies, the quality of the allergen is crucial, but in food allergens one should not underestimate their number. The prerequisite for the development of the reaction is the excess of the threshold dose of the allergen, which happens with a relative excess of the product with respect to the digestive capacity of the gastrointestinal tract "(L. Jaeger, 1990). This is an important thesis, since it makes it possible to identify individuals with various digestive disorders in the risk group and to correct digestive disorders in curative and prophylactic programs for food allergies. Almost any food product can be an allergen, however, cow's milk, chicken eggs, seafood (cod, squid, etc.), chocolate, nuts, vegetables and fruits (tomatoes, celery, citrus fruits), seasonings and spices, yeast, flour are the most allergenic. .
According to the data of Studenikin and II Balabolkin (1998), a cross allergy within a single botanical family is possible: citrus fruits (oranges, lemons, grapefruits); pumpkin (melon, cucumber, zucchini, pumpkin); mustard (cabbage, mustard, cauliflower, Brussels sprouts); Solanaceae (tomatoes, potatoes); pink (strawberries, strawberries, raspberries); plum (plum, peaches, apricots, almonds), etc. You should also focus on meat products, especially on poultry meat. Although these products do not have a big sensitizing activity, however, antibiotics are included in the diet of birds before slaughtering, and they can cause allergic diseases associated not with food, but with drug allergies. As for flour, more often flour becomes an allergen by inhalation, and not by ingestion through the mouth.
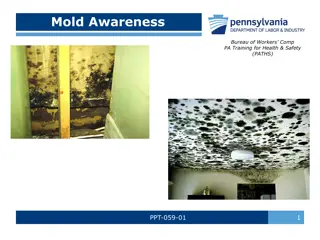
Allergens of house dust. These allergens are most significant for allergic diseases of the respiratory system, in particular, bronchial asthma. The main allergens of household dust are the chitinous cover and the products of the livelihood of Dermatophagoides pteronyssimus and Derm. Farinae. These pincers are widely distributed in beds, carpets, upholstered furniture, especially in old houses and old bedding. The second most important allergens of home dust are allergens of molds (more often Aspergillus, Alternaria, Penicillium, Candida). These allergens are most often associated with raw unventilated rooms and the warm season (April-November); they are also part of the allergen of library dust. The third most important in this group are allergens of domestic animals, and the most sensitizing ability is possessed by cat allergens (dandruff, wool, saliva).
Allergens - foreign substances, which, entering the body, become the main cause of allergic reactions
Vegetative allergens. They are primarily related to the pollen, and the main place belongs to pollen, and pollen ragweed, wormwood, swans, hemp, timothy, rye, plantain, birch, alder, poplar, hazel are the most common etiologic factor of pollinosis. According to the data of M. Ya. Studenikin and I. I. Balabolkin (1998), the common antigenic properties (cross-allergy) are pollen of cereals, mallow, polynia, ambrosia, sunflower; pollen of birch, alder, hazel, poplar, aspen. These authors also note the antigenic relationship between the pollen of birch, cereals and apples.
Since medications are usually relatively simple chemical compounds, they act as haptenes, connecting with the body's proteins to complete antigen. In this regard, the allergenicity of medicinal substances depends on a number of conditions: 1) the ability of a drug or its metabolites to be conjugated to a protein, 2) the formation of a strong bond (conjugate) with the protein, resulting in the formation of a complete antigen. It is this circumstance that determines a fairly frequent cross-sensitization of drugs. L.V. Luss (1999) cites such data: penicillin cross-reacts with all penicillin series preparations, cephalosporins, sultamycillin, sodium nucleate, enzyme preparations, a number of food products (mushrooms, yeast and products on yeast basis, kefir, kvass, champagne ); sulfanilamides cross react with novocaine, ultracaine, anesthesin, antidiabetic agents (diabeton), triampur, paraaminobenzoic acid; Analgin cross-reacts with non-steroidal anti-inflammatory drugs, acetylsalicylic acid derivatives and salicylates, food products containing tartrazine, etc.
In this connection, another circumstance is important. Simultaneous administration of two or more drugs can affect the metabolism of each of them, violating it. The violation of the metabolism of drugs that do not have sensitizing properties can cause allergic reactions to them. L. Yeager (1990) cited this observation: the use of antihistamines in some patients caused an allergic reaction in the form of agranulocytosis.
It is important to give clinical guidelines that allow differential diagnosis of drug allergy and pseudoallergia. Pseudoallergia often occurs in women after 40 years on the background of diseases that disrupt the metabolism of histamine or the sensitivity of receptors to BAS (pathology of the liver and biliary tract, gastrointestinal tract, neuroendocrine system). The background for the development of pseudoallergies are also polypharmacy, oral administration of drugs for ulcerative, erosive, hemorrhagic processes in the mucosa of the gastrointestinal tract; dose of the drug is not appropriate for the age or weight of the patient, inadequate therapy for the current disease, changes in the pH of the medium and the temperature of solutions administered parenterally, simultaneous administration of incompatible drugs (L.V. Luss, 1999).
Typical clinical signs of pseudoallergia are: the development of the effect after the initial administration of the drug, the dependence of the severity of clinical manifestations on the dose and mode of administration, the frequent absence of clinical manifestations with repeated administration of the same drug, the absence of eosinophilia.
Previously, bacterial allergy was associated with delayed type hypersensitivity, since high allergic activity of nucleoprotein fractions of the microbial cell was established. However, back in the 1940s Swineford O. and Holman J. J. (1949) showed that polysaccharide fractions of microbes can cause typical IgE-dependent allergic reactions. Thus, bacterial allergy is characterized by a combination of delayed and immediate reactions and this served as the basis for including specific immunotherapy (SIT) in the treatment of allergic diseases of the bacterial nature. At present, "neisserial" bronchial asthma, "staphylococcal" infectious-allergic rhinitis, etc. are singled out. A practical doctor should know that it is not enough to establish the infectious-allergic nature of the disease (for example, bronchial asthma), it is also necessary to decipher what kind of conditionally pathogenic flora determines allergization. Only then, applying in the complex treatment of SIT of this allergovaccine, you can get a good therapeutic effect.
Complaints typical of allergic diseases appear either in a completely healthy person, or, if the patient, then can not be explained by the peculiarities of his pathology. Common manifestations: chills, fever, agitation, weakness, dizziness, migraine-like syndrome, pallor of the skin, lowering of arterial pressure, itching, burning, sneezing, enlarged lymph nodes. Local manifestations. Most often they are manifested by complaints from the skin, gastrointestinal tract, mucous nasopharynx, bronchial tree, mouth and joints. Skin manifestation: redness and dryness of the cheeks, itching, burning, photosensitivity, sensitivity to cold, skin rashes (erythema, papules, blisters, maculopapular rashes, maculopapular eruptions, coripiform, scarlet-like, etc.). All skin rashes are often accompanied by itching and burning, however, not necessarily. Typically, this resembles a nettle burn.
Gastrointestinal tract: flatulence, pain and burning in the abdomen, unstable or frequent loose stools, constipation, nausea, vomiting, stomach or intestinal colic, reactive pancreatitis. Eye symptomatology: foreign body sensation in the eye, itching, burning, lacrimation, eyelid puffiness, eyelid dermatitis, blepharitis, conjunctivitis, keratitis, uveitis, scleritis, etc. Symptomatology from the mucous nasopharynx, bronchial tree and oral cavity: sore throat, itching, burning, sneezing, coughing or dry cough, copious watery, often foamy discharge from the nose, swelling of the nasal mucosa, nasopharynx, nasopharyngeal gland; difficulty breathing, bronchospasm, geographical language (a reliable sign of an allergic disease). Pain in the joints and muscles is quite an alarming symptom, since they testify to the systemic nature of allergic diseases. Quite often these complaints are encountered with drug and food allergies.
In the clinical picture of HIT, two phases are distinguished: early and late. The early phase is clinically manifested in a few minutes (up to 30 minutes) after contact with the allergen and also quickly stops (not more than an hour). At the heart of this phase, the above-mentioned SNT mechanisms associated with the release of BAS and the development of pathophysiological disorders (vasodilation, increased permeability, edema, mucus hyperplasia, smooth muscle spasm), which are clinically manifested by erythema, intestinal colic, bronchospasm, edema, blisters, mucous segregated, itching, burning, etc.
In the clinical picture of HIT, two phases are distinguished: early and late. The late phase begins in 2-6 hours and lasts 1-2 days. At the heart of this phase, inflammation," where the main actors are neutrophils and eosinophils, infiltrating proteolytic enzymes (extracellular cytolysis) under the influence of which the complement system is activated to form anaphylotoxins, the blood coagulation system is activated , its aggregate state (microthrombi) is disturbed. Production of activated mast cells and leukocyte-migrant cytokines (IL-1, IL-6, TNF, chemokines, GM-CSF) infiltration and maintenance of inflammation (A.A .Yarilin, 1999). the so-called "allergic the lesion, releasing kinins are formed, the promotes leukocyte
Conditionally allergic diseases can be divided into systemic and local. The main place of localization of mast cells - serous membranes, spleen, epithelium and submucosal layers of the gastrointestinal, respiratory and urogenital tracts; skin, connective tissue of capillary couplings. If the clinical symptomatology of an allergic disease comes from several places of mast cell localization, then one speaks of a systemic allergic disease. Clinically, this manifests itself in various combinations of gastrointestinal tract, etc. With local allergic diseases, clinical symptoms only occur from individual loci of fixation of mast cells (rhinitis, conjunctivitis, urticaria, gastritis, etc.). The only exception is the clinical symptomatology, which comes from the location of mast cells in the connective tissue of capillary couplings. It is always a systemic allergic disease, because it is based on vasculitis, which manifests itself in maximum expression with anaphylactic shock. the nasopharynx, skin,
Frequent objective signs of allergic diseases are eyelid hyperemia and edema of their skin, edema and congestion hyperemia, eyeballs. Almost mandatory objective signs of allergic diseases are swelling and swelling of mucous membranes; and also serous or foamy discharge (more often from the nose). Changes in mucous membranes with allergic diseases are typical: the mucous membranes are swollen with a marble shade, often cyanotic, edema of the posterior arch, tongue, posterior pharyngeal wall with multiple clusters of lymphoid tissue. For mucous membranes of the lower and middle nasal conchas, the presence of white spots (spots Voyachek). It is important to remember that in the first year of life there can not be hypertrophy of adenoids - their increase in this period is a consequence of edema accompanying allergic diseases. Once again, attention should be paid to the "geographical" language - a reliable sign of allergic diseases.
Objective signs on the part of the broncho-pulmonary system: more often dry, sometimes small- and medium-bubbling rales, an easy boxed tint of percussion sound. With palpation of the abdominal cavity tend to be soreness in the upper half of the abdomen, spasms of the jejunum, as gastrointestinal variants of allergy are more often manifested by jejunitis, duodenitis, gastritis, bulbitis, esophagitis. Reduced blood pressure, tachycardia, elevated body temperature are also frequent objective manifestations of allergic diseases. It should be emphasized again that these clinical signs are important in the diagnosis of allergic diseases only when they appear in healthy individuals or when these clinical signs can not be explained by the patient's existing disease.
There are three directions in the diagnosis of allergic diseases: - nosological diagnosis, or clinical identification of an allergic disease; - pathogenetic diagnosis, or determination of the characteristics of DIT or HIT; - etiological diagnosis, or determination of the causative factor of DIT or HIT.
At present, the problem of isolating at-risk groups of allergic diseases has not received its worthy development and the clinical guidelines for identifying at-risk groups are rather meager: -- genealogical anamnesis; -- family history; -- neonatal pathology.
Prognostic role of IgE level in children and adults (according to Humburger). Age Up to 2 weeks Level of IgE in IU/l <0.5 >0.5 6 6-15 16-60 >60 60 61-210 211-450 >450 Probability of allergic diseases in %. 12 45 5 20 35 ~100 8 22 36 ~100 Up to 3 years Children and adults
Differential diagnosis of DIT and HIT based on a comprehensive assessment of immunological tests. Immunological tests Number of eosinophils DIT + + HIT Number of basophils + + Number of monocytes +- - + + - + - - CD4 CD8 +- CD20 CD23 IgA IgE IgG IgG4
Differential diagnosis of DIT and HIT based on a comprehensive assessment of immunological tests(continuation) Immunological tests IL-2 DIT HIT + + + IL-4 + + + + + IL-5 IL-12 IF-gamma FNT-alpha FNT-beta + increase in the indicator; - decrease in the indicator
In 1952, Parrot and Urquia revealed the ability of healthy people's blood serum to bind free histamine and called this property histamine-pexy. They proposed a method for quantitatively taking into account this phenomenon, which they called a histaminopex index (HPI), and it was found that a decrease in HPI below 30% indicates an allergic condition. Later, their data were confirmed by numerous researchers and HPI became widely used in the diagnosis of allergic diseases.
In 1961, Mikol, Renoux, Merklen discovered an antihistamine factor (AHF), which reflected another side of the binding of blood serum histamine, because the histamine-serum ability of the serum was lost upon heating for two hours at a temperature of 56 C; while the ability of the blood serum to agglutinate the histamine-laden particles of latex, which is the basis of the determination of the AHF, was completely preserved. The titer of the AHF below 1/160 was characteristic for allergic diseases.
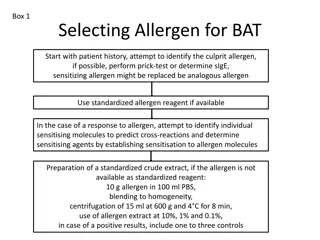
At the basis of etiological diagnostics is an attempt with paraclinical tests to establish a specific antigen causally significant for the development of this particular allergic disease. All paraclinical tests used for these purposes can be divided into two large groups: -- Diagnostic tests in vivo; -- Diagnostic tests in vitro.
Diagnostic tests in vivo. These include skin tests and provocative tests, which are conducted directly in the patient. Skin tests are divided into cutaneous (application, compress, drip, etc.), scarification tests, prick tests, modified prick test, intradermal tests. General conditions for carrying out all in vivo diagnostic tests - they should be conducted by professionals in specially equipped offices that allow for the provision of emergency care.
Diagnostic tests in vivo. Skin tests are performed only during the remission of allergic disease; they are contraindicated in the acute period of any other (non-allergic) disease, during pregnancy, breast-feeding, in the first 2-3 days of the menstrual cycle; in the absence of a convincing anamnesis and preliminary examination, indicating the presence of an allergic disease.
Provocative tests. They are used to confirm the causative significance of the allergen in cases of discrepancy in the history and skin tests. Categorically it is contraindicated to conduct provocative tests for non-specialists and in the absence of the possibility of providing emergency medical assistance, especially with inhalation provocations. Most often, the following variants of provocative samples are used: conjunctival, nasal, inhalation, oral. The indicator of a positive sample is an exacerbation of the symptoms of the corresponding allergic disease.
The opposite provocative is a test with the exception of the alleged allergen established on the basis of an allergic medical history. This test should be carried out by every doctor, as reducing the clinical manifestations of an allergic disease when excluding the putative allergen not only confirms its etiological role in this disease, but also serves as a prognosis for the effectiveness of treatment.
Diagnostic tests in vitro. From our point of view, these are the most effective and safe tests of etiologic diagnosis of allergic diseases, which in the future should replace in vivo tests except for the sample with the exception of the supposed allergen. The most widespread among these tests was a radioallergo- adsorbent test (RAAT). RAAT allows to measure the level of antibodies specific for allergens. The essence of the method is that if allergen-specific IgE antibodies are present in the blood, they bind to the corresponding allergens fixed on an inert matrix.
Diagnostic tests in vitro. After the addition of radioactive anti-IgE antibodies, they bind to the formed allergen-IgE antibody complexes and allowance for radioactivity gives the level of allergen-specific IgE antibodies. RAAT allows to carry out allergodiagnosis in the acute stage of the disease; the test results are not affected by pharmaceuticals and other factors; there is a good correlation of the test with the severity of the disease. The main disadvantage of RAAT is its rather high cost. However, the appearance of various modifications of RAST (enzyme allergoadsorbent test, fluorescent allergoadsorbent test, combined allergic adsorbent test, immunoperoxidase system, etc.) allows us to hope for overcoming this shortcoming.
Diagnostic tests in vitro. The Shelley test or an indirect basophil degranulation test was also widely used. The reaction is based on the basophilic binding of animals to Fc-fragments of IgE antibodies upon the addition of blood serum to patients with allergic diseases. After the addition of allergens specific for these IgE antibodies, the basophils sensitized in this manner and the release of BAS are degranulated. The reaction indicator is the percentage of degranulated basophils. In addition to these most common methods, passive hemagglutination (PHGA), precipitation, indirect basophil degranulation test, immunoblotting method, allergen neutralizing serum activity, allergen-specific granulocyte damage response, etc. are used.
SCHEME OF DEVELOPMENT OF ALLERGIC REACTION OF IMMEDIATE TYPE IMMUNOLOGICAL 1. INTERACTION OF LYMPHOCYT WITH NEW ANTIGENS 2. TRANSFORMATION OF LYMPHOCYT TO PLASMOCYT AND SYNTHESIS OF ANTIBODIES 3. FIXATION OF ANTIBODIES ON THE MAST CELLS PATHOCHEMICAL 1. INTERACTION OF ANTIBODIES WITH REPEATEDLY ANTIGENED ANTIGEN IN THE ORGANISM 2. DESTRUCTION OF THE MAST CELLS AND EMISSION OF MEDIATORS (HISTAMIN AND OTHER) Pathophysiological DEVELOPMENT OF GENERAL AND LOCAL MANIFESTATIONS OF ALLERGY (skin hyperemia, itching, skin rashes, heat, headache, difficulty breathing, etc.) 43
CLASSIFICATION OF ANTI-ALLERGIC DRUGS The drugs used to suppress hyperimmune reactions of immediate type: 1. Glucocorticoid preparations 2. Stabilizers of membranes of mast cells (kromolin-sodium, ketotifen) 3. Antihistamines (blockers of H1-histamine receptors): - H1-antagonists of the 1st generation, which have a noticeable sedative effect; - H1-antagonists of the 2-nd generation, not giving a sedative effect in the recommended therapeutic dose, however, with an increase in the dose showing a sedative effect; - H1-antagonists of the 3-rd generation, not causing signs of sedation and when the therapeutic dose is exceeded. 4. Leukotriene receptor antagonists (zafirlukast, montelukast), inhibitors of leukotriene synthesis (zileuton) 5. Functional antagonists of mediators of allergy: adrenomimetics, m-cholinoblokars, antispasmodics. 44
Means used to suppress hyperimmune states of delayed type. Cytotoxic agents Cyclosporin Glucocorticoids Immunoglobulins antimitocyte NSAIDs 45
HISTAMINE is the main pathophysiological agent in the development of an allergic reaction of immediate type MAIN EFFECTS OF HYSTAMINE: An increase in the tonicity of smooth muscles of the bronchi, uterus, intestine; Spasm of large arteries and dilatation of capillaries (decrease of blood pressure); Increased vascular permeability; Increased gastric secretion; Stimulation of adrenal secretion of epinephrine and glucocorticoids. 46
EXAMPLES OF DEVELOPMENT OF AN ALLERGIC REACTIONS OF IMMEDIATE TYPE Allergic reaction developing in the respiratory tract Allergic reaction, accompanied by the development of nasal symptoms 47
CLASSIFICATION OF ANTIHISTAMINE PREPARATIONS (H1-BLOCKERS) 1 generation 2 generation 3 generation Suprastin (chloropyramine) Dimedrol (diphenhydramine) Diazolin (mebhydroline) Tavegil (Clemastin) Pipolphen (diprazine) Claritin (loratadine) Zirtek (cetirizine) Kestin (ebastin) Histalong (astemizole) Semprex (acrescine) Telfast (fexofenadine) Erius (desloratadine) 10
Mechanism of action Classical H1-antagonists are competitive blockers of H1- receptors, so their binding to the receptor is reversible. To achieve the main pharmacological effect, it is necessary to use relatively high doses of such drugs, while undesirable side effects of classical H1-antihistamines are more easily and more often manifested. In addition, most of these drugs have a short-term effect, which means that they must be taken 3-4 times a day. Antihistamines of the second generation bind to H1- receptors uncompetitively. Such compounds can hardly be displaced from the receptor, and the ligand-receptor complex formed dissociates relatively slowly, which explains the longer action of these drugs. 49
The main side effects of antihistamine drugs of 1 st generation: - blockade of receptors of other mediators (for example, M- holinoretseptorov, which manifests itself in the form of dryness of the oral mucosa, nose, throat, bronchi, rarely - urination and blurred vision); - local anesthetic action; - Quinidine-like action on the heart muscle; - analgesic effect and enhancing action in relation to analgesics; - antiemetic action; - the effect on the central nervous system (sedation, impaired coordination, dizziness, lethargy, decreased ability to concentrate attention); - increased appetite; - Disorders from the digestive side (nausea, vomiting, diarrhea, loss of appetite, unpleasant sensations in epigastrium); - Tachyphylaxis (reduction of therapeutic effect with prolonged use). 50