Understanding Acute and Chronic Inflammation: Causes, Outcomes, and Resolution
Acute inflammation results in either resolution or progression to chronic inflammation, with outcomes like restoration of normalcy, fibrosis, or scarring. Chronic inflammation can be caused by viral infections, persistent microbial infections, exposure to toxic agents, or autoimmune diseases. Macrophages and lymphocytes play crucial roles in both acute and chronic inflammatory responses, releasing various mediators and growth factors. Understanding the events in inflammation resolution is key to managing inflammatory conditions effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
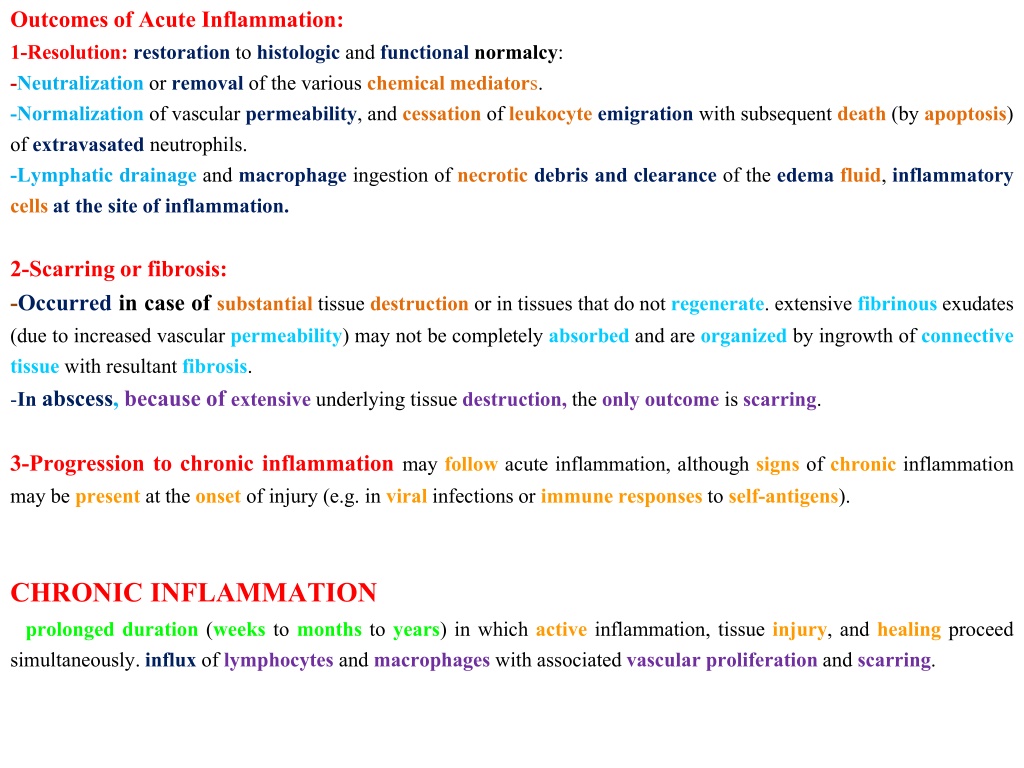
Outcomes of Acute Inflammation: 1-Resolution: restoration to histologic and functionalnormalcy: -Neutralization or removal of the various chemical mediators. -Normalization of vascular permeability, and cessation of leukocyte emigration with subsequent death (by apoptosis) of extravasated neutrophils. -Lymphatic drainage and macrophage ingestion of necrotic debris and clearance of the edema fluid, inflammatory cells at the site of inflammation. 2-Scarring or fibrosis: -Occurred in case of substantial tissue destruction or in tissues that do not regenerate. extensive fibrinous exudates (due to increased vascular permeability) may not be completely absorbed and are organized by ingrowth of connective tissue with resultant fibrosis. -In abscess, because of extensive underlying tissue destruction, the only outcome is scarring. 3-Progression to chronic inflammation may follow acute inflammation, although signs of chronic inflammation may be present at the onset of injury (e.g. in viral infections or immune responses to self-antigens). CHRONIC INFLAMMATION prolonged duration (weeks to months to years) in which active inflammation, tissue injury, and healing proceed simultaneously. influx of lymphocytes and macrophages with associated vascular proliferation and scarring.
Cauases of chronic inflammation: 1-Viral infections. 2-Persistent microbial infections. -Mycobacteria (tubercle bacilli), Treponema pallidum (causative organism of syphilis), and certain fungi. evoke an immune response called delayed hypersensitivity (granulomatous reaction). 3-Prolonged exposure to potentially toxic agents. -Exogenous nondegradable material such as Inhaledparticulate silica, which can induce (silicosis) in the lungs. -Endogenous agents such as chronically elevated plasma lipid components, which may contribute to atherosclerosis. 4-Autoimmune diseases. -Immune response to self-antigens and tissues. (e.g., rheumatoid arthritis or multiple sclerosis). Chronic inflammatory Cells and Mediators 1-Macrophages -(mononuclear phagocyte system) in different organs. -Filters for particulate matter, microbes, and senescent cells. -Sentinels to alert the specific components of the immune system (T and B lymphocytes) to injurious stimuli. -Emigrate to the site of injury within the first 24 to 48 hours after onset of acute inflammation. -Activated by bacterial endotoxin, cytokines secreted by sensitized T lymphocytes (IFN- ), mediators of acute inflammation, and extracellular matrix proteins such as fibronectin. -After activation undergo transformation into the large, flat, and pink (epithelioid macrophages). -IL-4 or IFN- (from lymphocytes) can also induce macrophages to fuse into large, multinucleated cells called giant cells.
Macrophage products include: -Proteases,plasminogen activator. -Complement components. -Reactive oxygen species and nitric oxide. -AA metabolites (eicosanoids). -Cytokines, such as IL-1 and TNF, as well as a variety of growth factors (PDGF)Platelet-derived growth factor , (FGF) fibroblast growth factors, Transforming growth factor beta (TGF-beta) that influence the proliferation of smooth muscle cells and fibroblasts and the production of extracellular matrix (as collagen). 2-Lymphocytes -Both T and B lymphocytes migrate into inflammatory sites. -T lymphocytes have a reciprocal relationship to macrophages in chronic inflammation; they are initially activated by interaction with macrophages presenting "processed" antigen fragments on their cell surface. The activated lymphocytes then produce a variety of mediators, including (IFN- ), a major stimulating cytokine for activating (monocytes and macrophages).Activated macrophages in turn release cytokines, including (IL-12, IL-1 and TNF), that further activate (lymphocytes) as well as other cell types. 3-Eosinophils -Present in inflammatory sites around parasitic infections or as part of immune reactions mediated by IgE, typically associated with allergies. -Recruited chemokines (e.g., eotaxin) derived from leukocytes or epithelial cells. -Eosinophil-specific granules contain major basic protein (MBP), that is toxic to parasites but also causes epithelial cell lysis.
4-Plasma Cells -product of B-cell activation. -produce different Abs(immunoglobulins). 5-Mast Cells -Sentinel cells in connective tissues throughout the body. -participate in both acute and chronic inflammatory responses. -Release histamines and AA metabolites. -Elaborate cytokines such as TNF, thereby participating in more chronic responses. -play a role in parasitic infections. Fibroblast -Activated by macrophages growth factors (PDGF, FGF, TGF-beta). -Produce of ECM (as collagen). -PDGF = platelet Derived Growth Factor. -FGF = Fibroblast Growth Factor. -TGF-beta = Transforming Growth Factor.
The roles of activated macrophages in chronic inflammation. Macrophages are activated by nonimmunologic stimuli such as bacterial endotoxin or by cytokines from immune-activated T cells, particularly (IFN-gamma;). The products made by activated macrophages that cause tissue injury and fibrosis are indicated. AA, Arachidonic acid; PDGF, platelet-derived growth factor; FGF, fibroblast growth factor; TGF-beta;, transforming growth factor beta.
Macrophage-lymphocyte interactions in chronic inflammation. Activated lymphocytes and macrophages stimulate each other, and both cell types release inflammatory mediators that affect other cells. IFN- gamma;, interferon-gamma; IL-1, interleukin-1; TNF, tumor necrosis factor.
Chronic Pneumonia Thickenning of alveolar septa (Fibrosis) Empty alveolar spaces
Chronic Pneumonia Lymphocytes
Chronic Pneumonia Alveolar spaces with overfilled macrophages
Chronic Pneumonia Alveolar spaces with overfilled macrophages
Chronic pneumonia Massive fibrosis with inflammatory cells
Chronic pneumonia Massive infiltration of lymphocytes Newly formed Blood vessels
Chronic myocardial infarction Necrotized myocardial cell Fibroblasts
Chronic myocardial infarction associated with angiogenesis (arrows)
Granulomatous inflammation (Granuloma) Granulomatous inflammation is a distinctive pattern of chronic inflammation characterized by aggregates of activated macrophages that assume a squamous cell-like (epithelioid) appearance. Result from persistent T-cell responses to certain microbes or foreign body such as: -Bacteria (Mycobacterium tuberculosis, Treponema pallidum causing the syphilitic gumma). -Fungi. -parasites. -Inert foreign bodies (e.g., suture, splinter, breast implant) these types called (foreign body granulomas). Tuberculosis is the archetypal granulomatous disease due to infection, where T-cell-derived cytokines are responsible for persistent macrophage activation.
Component of granuloma: 1-Central zone of necrosis (caseous necrosis). 2-Aggregates of epithelioid macrophages. 3-Activatedmacrophages. 4-Collar of lymphocytes secreting the cytokines responsible for ongoing macrophage activation. 5-Older granulomas surrounded by rim of fibroblasts and connective tissue. 6-Multinucleated giant cells 40 to 50 m in diameter: large mass of cytoplasm and multiple nuclei and derive from the fusion of 20 or more macrophages.
Grossly, a granuloma (arrow) tends to be a focal lesion. Seen here in a hilar lymp node is a granuloma. Granulomas due to infection are often "caseating" because they have prominent caseous necrosis.
Granuloma Langhans giant cell
Lung : Granuloma Langhans gaint cell Central caseous necrosis
Lung : Granuloma Epithelioid cells Lymphocytes