Understanding Acid-Base Disorders and Blood Gas Analysis
This educational content provides definitions, formulas, and explanations related to acid-base disorders, blood gas analysis, dissociation constants, the Henderson-Hasselbalch equation, and carbonic acid in clinical pathology. Learn about acids, bases, pH, ionization constants, and how these concepts apply in medical contexts.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Acid Acid- -Base Disorders & Base Disorders & Blood Blood Gas Analysis Gas Analysis (Part (Part I) I) APRIL 2018 CLINICAL PATHOLOGY FELLOWSHIP PROGRAM
Definitions Term Definition A substance that can yield a hydrogen\ hydronium ion when dissolved in water (gives off a H+). Acid (HA) Base (A-) A substance that can yield hydroxyl ions (OH-). An expression describing the [H+]. pH = - log [H+] pH Ionization constant (K) The relative strengths of acids and bases, their ability to dissociate in water, are described by their dissociation constant. pKa Equilibrium A state when there is no further change in conc. The negative log of K, is also the pH in which protonated and unprotonated forms are present in equal conc. Buffer The combination of a weak acid or weak base and its salt, is a system that resists changes in pH. The effectiveness of a buffer depends on the pKaof the buffering system and the pH of the environment in which it is placed. e.g. proteins and plasma.
Conversion between pH and [H+] for selected values within the limits compatible with life Conversion from pH to [H+ ] Conversion from pH to [H+ ] pH [H+ ] nM 56 [H+ ] nM pH 7.25 7.7 20 7.2 63 7.65 22 0.3 increase in pH 2 fold decrease 7.15 71 7.6 25 in [H+] 7.1 79 7.55 28 7.05 89 7.5 31 7 100 7.45 7.4 35 40 6.95 6.9 112 125 7.35 45 6.85 142 7.3 50
Dissociation Constants ( Dissociation Constants (K Ka a) ) In any chemical reaction, there will ultimately occur an equilibrium. For acids, this refers to the [H+] at which the acid has half dissociated. The dissociation constant (Ka) describes the concentration of the acid and base generated when the acid dissociates pKa = - log Ka If we know the dissociation constant for an acid, we can use the concentrations of any 2 of the 3 compounds (hydrogen, acid, base) to solve for the unknown conc. of the third. HA H+ + A- Weak acid proton Salt or conjugate base
The Henderson-Hasselbalch Equation It is an equilibrium equation. pH is used to express [H+] H+ + A- HA HA A- (A-) (H+) H+ Ka x = Ka = HA HA A- Taking the log and X by (-1) pH pKa - log = A- pH pKa + log = Eliminating the minus sign HA
Carbonic Acid (C.A.) For carbonic acid: Ka = 8 x 10 -7 pKa = 6.1 The source of carbonic acid in our body is dissolved CO2 (dCO2) gas, followed by hydration to form carbonic acid (H2CO3). The concentration of H2CO3 is proportional to the partial pressure excreted by dCO2. In plasma at 37 C, the value for the combination of the solubility constant for pCO2 and the factor to convert mm Hg to mmol/L is 0.0307 mmol/L/mm Hg.
C.A. CO2 + H2O H2CO3 H2CO3 H+ + HCO3- C.A. = Carbonic Anhydrase
Example: Proton = H+ conjugate base = A- Acid = HA Ka = 8 x 10 -7 pKa = 6.1 Solubility coefficient of CO2 = 0.0307 x pCO2 H+ + HCO3- H2CO3 HA A- H+ Ka x = A- pH pKa + log = HA
Buffers Buffers A buffer can be a mixture of a weak acid and its conjugate base. There must be about equal amounts of the weak acid and its conjugate base to allow the buffer to neutralize both acid and base Optimum buffering capacity is reached when the ratio of acid to its conjugate base is ~ 1 This will occur when the pH is near pKa The buffering capacity is dependent on the: relative amount of buffer components absolute amounts of buffer components
Buffers Relative amounts of buffer components A- Maximum buffering capacity: when the weak acid and its conjugate base are roughly equal B- Less, (but still working) buffering capacity: when the ratio of acid to base conc. ranged from 10:1 to 1:10 i.e. within 1 of the pKa of the weak acid. C- Ineffective buffering capacity: when the ratio of acid to base conc. is beyond 10:1 to 1:10 i.e. beyond 1 of the pKa of the weak acid.
Buffers Absolute amounts of buffer components when there is 1 mmol of the weak acid and 1 mmol of its conjugate base: the buffer is weaker (i.e. less resistant to the addition of acid or alkali) than would a solution containing 1 mol of the weak acid and 1 mol of its conjugate base . 2 mixtures of buffer (acid and its conjugate base) will have the same pH when the ratio of acid to base is the same. However, their buffering capacity would be more in the mixture having higher molar conc. of the buffer components.
Physiological Buffers in our Body Buffering agent pKa % of the blood buffering capacity Comment Hemoglobin ~ 6.8 80 Although hemoglobin is the most abundant buffer; CA/Bicarb is the most important buffer system in vivo. WHY?? The body can change the conc. of either CA (as pCO2) or bicarbonate relatively quickly, keeping CA:Bicarb relatively constant minimizing pH changes Serum protein 6-8 14 Carbonic Acid /Bicarbonate system 6.1 6
Health condition (physiological pH) In health, when the kidney and lungs are functioning properly, a 20:1 ratio of HCO3- will be maintained (resulting in a pH of 7.4) A- pH pKa + log = HA 20 24 mmol\L = (0.0307 mmol\L mm Hg) x 40 mm Hg 1 pH = 7.4 Adding the log of 20 (1.3) to the pKa (6.1)
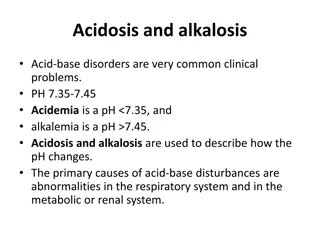
Acidosis vs. Acidosis vs. Acidemia Acidemia Acidosis Acidemia An increase in the blood [H+] and a decrease in pH A net increase in acid relative to base All individuals who are acidemic have an acidosis, but not all who are acidotic have acidemia
Changes in Changes in Simple Simple Acid Acid- -Base Parameters in Various Acid Base Parameters in Various Acid- -Base Disorders Base Disorders Disorder pH Primary change Compensation Comments HCO3- Respiratory Acidosis pCO2 Metabolic compensation works by changing HCO3- renal excretion (HCO3- retention by kidneys). It begins quickly. It does not reach maximum for 3-5 days HCO3- Metabolic Acidosis pCO2 Respiratory compensation works by changing pCO2 excretion (CO2 excretion by lungs). It begins quickly It does not reach max for 12 hr. HCO3- Respiratory Alkalosis pCO2 Metabolic compensation (HCO3- excretion by kidneys). HCO3- Metabolic Alkalosis pCO2 Respiratory compensation (CO2 retention by lungs). In simple Acid-base disorders, the change in HCO3- should be accompanied by an equal change in Cl- (equal in amount but in the opposite direction to maintain electronutrality)
Respiratory Compensation Mechanism(s) Respiratory Compensation Mechanism(s) acidosis CO2 + H2O H2CO3 H+ + HCO3- &/or Metabolic alkalosis CO2 + H2O H2CO3 H+ + HCO3- &/or
Renal Compensation Mechanism(s) Renal Compensation Mechanism(s) CO2 + H2O H2CO3 H+ + HCO3- acidosis Respiratory alkalosis CO2 + H2O H2CO3 H+ + HCO3-
Changes in Changes in Mixed Mixed Acid Acid- -Base Disorders Base Disorders Mixed Acid-base disorders are when patients have more than one disorder. They occur much more common than simple disorder Unlike in Simple Acid-Base disorders, in mixed Acid-Base disorders the change in pCO2 and HCO3- are in opposite directions It is important to be able to recognize what changes represents compensation and what changes indicate the presence of mixed acid-base disorders.
Lab Tests of Acid-Base Status: Serum electrolytes Bicarbonate, Chloride, Potassium Bicarbonate: normal Bicarb, and Anion Gap (AG) rules out all acid-base disorders except for acute respiratory abnormalities. Most instruments currently measure bicarb directly by enzymatic methods or ion-selective electrodes. Some older method report total CO2 : this overestimates bicarb by ~ 1-2 mmol/L because it also measures any dCO2 gas or that bound to protein.
Lab Tests of Acid-Base Status: Serum electrolytes Bicarbonate, Chloride, Potassium Chloride: normally changes in parallel with sodium. A change in Cl greater than any change in sodium: indicates the presence of an acid-base disorder. It changes in the opposite direction to bicarb, but by the same amount, in all acid-base disorder except increased anion gap metabolic acidosis. If chloride and bicarb change in the same direction, independent of a change in sodium, then more than one acid-base disorder is present. Potassium: Potassium (K+) is the major intracellular cation in the body, with a concentration 20 times greater inside the cells than outside. Only 2% of the body s total K+ circulates in the plasma. K+ has several functions in the body including regulation of H+ concentration.
Anion Gap Anion Gap It is the difference between the major measured cations (Na+ and K+) and the major measured anions (Cl- and HCO3-). (Na+ + K+) - (Cl- + HCO3-) Increased Anion gap: Occurs whenever there is production of a metabolic acid (e.g. lactate) that is buffered byHCO3- . What are the other major unmeasured ions? Cations: Calcium, magnesium, and IgG Anions: albumin, phosphate, Amino Acids normal state = 15 Low Anion gap is due to: increased IgG &/or Decreased albumin Low Anion gap is common in multiple myeloma, HIV*, and cirrhosis. *HIV patients may have lower serum albumin and higher serum globulin concentrations.
Lab Tests of Acid-Base Status: Arterial Blood Gas It is the first line test for acid-base disorders, although it is done in far fewer individuals than electrolytes. Should be performed by a well trained personnel and following strict guidelines: Example of pre-analytical errors: 1. The presence of excess liquid or gas in the syringe used to collect blood gas specimens diffusion of CO2 out of the specimen (quick) and diffusion of O2 into the specimen (to a lesser extent). If Arterial pO2 is high, O2 will also diffuse out of the sample. 2. Specimen is not adequately chilled glucose metabolism will take place acidic metabolites pH How to verify the results of the Arterial Blood Gas? 1. Check the bicarb calculated from the Arterial blood gas 2. Compare it with the measured bicarb. from the electrolyte tests 3. The difference should not be > 2-3 mmol/L, with the calculated bicarb. always lower.
Lab Tests of Acid-Base Status: Second Line Tests Ketone bodies, lactates, Osmotic gap Ketone bodies: Acetoacetate, beta hydroxybutyrate are acids Acetoacetate and acetone are measured by the nitroprusside test. Lactate: the end product of anaerobic metabolism of Glucose. Blood should be collected without tourniquet (because lactate accumulates in tissues if venous drainage is impaired).
Lab Tests of Acid-Base Status: Second Line Tests Osmotic gap Osmotic Gap: It is the difference in between the measured osmolality and the calculated osmolality (which is the molar conc. of the major plasma solutes (electrolytes, glucose, urea)) The osmotic pressure is measured by: 1) Decrease in freezing point (used to detect ingested toxins because they are usually volatile and will not affect the vapor pressure) 2) Decrease in vapor pressure Calculated osmolality = 2 X (Na + Glc + BUN + Ethanol) The difference between them is the Osmotic gap. Normal osmotic gap is < 10
Acidosis (due to increased acid production) 1. Endogenous acids: increased generation of normal metabolic products (Ketone bodies, LA, congenital disorders of AA metabolism) 2. Exogenous acids: addition of exogenous products that can be metabolized to acids (methanol, salicylates) Mechanisms of this type of acidosis: Metabolic acids have pKa 4-5 (& will be completely ionized at normal body pH) The released H+ will be buffered by HCO3- increased Anion gap metabolic acidosis Start by measuring the KB (hydroxylbutyrate) and LA If the increase in the AG is not equal to the measured molar conc. of the endogenous acids ingestion of exogenous products in suspected.
Acidosis (due to decreased acid excretion) Renal Failure Disorders interfering with the ability of the lungs or kidney to excrete acids. Renal failure acidosis (because organic acids (LA, AA) & inorganic acids (phosphoric, sulfuric) cannot be cleared at a normal rate With acute RF, glomerular filtration is rapidly impaired quick development of this acidosis With chronic RF, excretion of the anions is preserved till glomerular filtration is severely impaired (occurs when the S creatinine is 10-12 mg/dL i.e. 880-1000 mol/L) acidosis in the very late stages of chronic RF
Acidosis (due to decreased acid excretion) Respiratory Failure Respiratory acidosis differs from other forms of acidosis in that the serum HCO3- and pCO2 are increased rather than decreased. Causes of Respiratory acidosis: Severe pneumonia Adult and neonatal respiratory distress syndromes Decrease gas expiration with acute or chronic airway obstruction Chest wall injuries Severe muscle weakness
Case 1 A 75-year-old widow, a known heavy smoker and chronic bronchitic, and a patient in a long-stay hospital, became very breathless and wheezy. The senior nurse called the doctor who was on duty, but he was unable to come at once because he was treating another emergency. He asked the nurse to start the patient on 24% oxygen. One hour later, when the doctor arrived, he examined the patient and took an arterial specimen to determine her blood gases. The results were as shown below. (Lecture Notes, 9th ed, p 34, case 3.1) Blood gas analysis Results Ref range H+ (nM) 97 37-45 pCO2 (kPa) HCO3- (mM) pO2 21.8 4.5-6 42 21-29 22.5 12-15 How would you describe the patient's acid-base status? Do you think that she was breathing 24% O2?
Case answer: Blood gas analysis Results Ref. range Comment H+ (nM) acidosis (high [H+] and low pH). 97 37-45 Respiratory acidosis (the only acidosis where both the pCO2 and HCO3- are high) pCO2 (kPa) 21.8 4.5-6 HCO3- (mM) Because the renal compensation by retention of HCO3- requires few days to be maximum, this cannot be the reason for her high HCO3-, since her recent illness is short in time despite her long history of chest complaints. 42 21-29 pO2 22.5 12-15 Alveolar PO2 must be greater than arterial PO2, so it was possible to conclude that the patient must have been breathing O2 at a concentration of at least 40%. On checking, it was found that the wrong mask had been fitted, and that O2 was being delivered at 60%.
Case 2 A young man sustained injury to the chest in a road traffic accident. Effective ventilation was compromised by a large flail segment. Investigations: Arterial blood parameter value Reference range pO2 (kPa) pCO2 (kPa) [H+] nM 8 12-15 8 4.5-6 58 37-45 HCO3- mM 25 21-29 What is your comment?
Case answer: Arterial blood parameter value Reference range Comment pO2 (kPa) pCO2 (kPa) [H+] nM 8 12-15 hypoxemia 8 4.5-6 respiratory 58 37-45 acidosis HCO3- mM 25 21-29 No renal compensation There is severe acidosis, and the raised pCO2 indicates that it is respiratory. The magnitude of the increase in [H+] suggests that no renal compensation has occurred. Such compensation can take several days to become fully effective, in contrast to the rapid respiratory compensation in non- respiratory disorders.
Case 3 An elderly man was brought into the A&E department after collapsing in the street. He was deeply comatose and cyanosed, with unrecordable blood pressure. The results of acid base analysis were as shown below. (Lecture Notes, 9th ed, p 39, case 3.4) Arterial blood parameter value Reference range Comment pO2 (kPa) pCO2 (kPa) [H+] nM 4.8 12-15 10.4 4.5-6 124 37-45 HCO3- mM 15.4 21-29 What is you comment?
Case answer: He has combined metabolic and respiratory acidosis. Such results are seen in patients with markedly impaired circulatory and respiratory function, such as that which occurs after a cardiac arrest. The man was found to have a large abdominal aortic aneurism that had ruptured. Arterial blood parameter value Reference range Comment pO2 (kPa) pCO2 (kPa) [H+] nM 4.8 12-15 Hypoxemia 10.4 4.5-6 Respiratory 124 37-45 Acidosis HCO3- mM 15.4 21-29 Metabolic
Acidosis (due to increased base excretion) Characterized by decreased blood level of HCO3- and increased Cl- WHY? Because the kidneys are forced to reabsorb increased amounts of Cl- along with sodium to maintain electroneutrality (since this acidosis is due to increased net excretion of HCO3-)
Followed in Part II of The Lecture Followed in Part II of The Lecture