The Pituitary Gland: Implications in Psychiatry
This presentation by Dr. Alexsandra Urhi delves into the anatomy, function, and psychiatric implications of the pituitary gland. It explores the interplay between endocrine structures, the CNS, and psychotropic drugs' effects on the pituitary gland.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
THE PITUITARY GLAND AND PSYCHIATRY PRESENTED BY DR. ALEXSANDRA URHI FEDERAL NEUROPSYCHIATRIC HOSPITAL, USELU, BENIN CITY 22nd MARCH, 2023 1
OUTLINE Objectives Introduction The anatomy of the pituitary gland The function of the pituitary gland The implication in psychiatry The effects of psychotropic drugs on the pituitary gland Conclusion/Recommendation References 2
OBJECTIVES To give an overview of the pituitary gland and associated structures. To give the psychiatric implications of pathologies of the pituitary gland and associated structures. 3
INTRODUCTION The pituitary gland serves as an intermediary between endocrine structures in executing several bodily functions. There is an interplay between the hypothalamus, pituitary and other structures in bringing about these functions. The study of these interactive process is known as Psychoneuroendocrinology . A term which encompasses the structural and functional relationships between hormonal systems and the central nervous system (CNS). 4
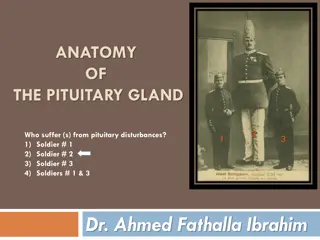
THE ANATOMY OF THE PITUITARY GLAND 5
THE ANATOMY OF THE PITUITARY GLAND THE PITUITARY GLAND [1,2]: Also called as hypophysis is a pea-sized endocrine gland with a mean weight of 0.5g. It is located in the bony cavity- sella turcica, at the base of the skull between the optic nerves. The pituitary gland is divided into two parts: - The anterior pituitary (front lobe) - The posterior pituitary (back lobe) It is connected to the hypothalamus by the pituitary stalk (also known as the infundibulum). 6
THE FUNCTION OF THE PITUITARY GLAND 7
THE FUNCTION OF THE PITUITARY GLAND The anterior pituitary produces the following hormones [3,4]: Adrenocorticotropic hormone (ACTH): - It plays a role in how the body responds to stress. - It stimulates the adrenal glands to produce cortisol (the stress hormone) - Cortisol has many functions including regulating metabolism, maintaining blood pressure, regulating blood glucose levels and reducing inflammation, among others. Follicle stimulating hormone(FSH): - FSH stimulates the testes to produce sperm and the ovaries to produce estrogen that is implicated in the development of the oocyte. 8
THE FUNCTIONOF THE PITUITARY GLAND Luteinizing hormone (LH): - It stimulates ovulation in females and testosterone in males Growth hormone (GH): - It stimulates growth Prolactin: - It stimulates breast milk production (lactation) after childbirth Thyroid-Stimulating hormone (TSH): - It stimulates the thyroid to produce thyroid hormones that control metabolism, energy and nervous system. 9
THE PHYSIOLOGY OF THE PITUITARY GLAND The posterior pituitary gland produces the following hormones [3,4]: Antidiuretic hormone (ADH or Vasopressin): - This hormone regulates the water balance and sodium levels in the body. Oxytocin: - The hypothalamus produces oxytocin and the posterior pituitary stores and releases it. - It assist in labor progression during childbirth by sending signals to the uterus to contract. - It is also involve in milk let down during breastfeeding. 10
IMPLICATION IN PSYCHIATRY The hypothalamic-pituitary-adrenal axis The hypothalamic-pituitary-thyroid axis The hypothalamic-pituitary-gonadal axis Prolactin Oxytocin 11
HYPOTHALAMIC-PITUITARY- ADRENAL AXIS (HPA) 12
CORTISOL Pathological alterations in HPA function resulting in hypercortisolemia have been associated primarily with mood disorders in Cushing's syndrome. It has been found that major depression is a life threatening complication, which may affect 50-60% of patients with Cushing s syndrome [5]. Alterations in HPA function associated with depression include: - Elevated cortisol concentrations - Failure to suppress cortisol in response to dexamethasone - Increased adrenal size and sensitivity to ACTH. - A blunted ACTH response to CRH 13 - Elevated CRH concentrations in the brain.
CORTISOL While depression is one of the most important psychological symptoms associated with cushing s syndrome, other symptoms such as mania, hypomania, suicidal thought generalized anxiety or panic disorders [6, 7, 8] have also been noticed. Significant improvement or even complete resolution of anxiety , hypomania, mania, depression and mood irritability have been found after correction of the hypercortisolism [9,10]. Reduced cortisol levels normalize mood and mental status. 14
CORTISOL In Addison s disease (characterized by adrenal insufficiency) symptoms include; Apathy, social withdrawal, impaired sleep, decreased concentration and prominent fatigue [11] Anglin et al. [12] brings up the point that psyhiatric symptoms may even be the only symptoms present in Addison s disease patients, hence, it is important when seeing these symptoms to maintain a high index of suspicion for this potentially fatal condition. Replacement of glucocorticoid resolves behavioral symptoms [11]. Similarly, HPA abnormalities are reversed in persons who are treated successfully with antidepressant medications. Failure to normalize HPA abnormalities is a poor prognostic sign. 15
HYPOTHALAMIC-PITUITARY- THYROID AXIS 16
THYROID HORMONE Stern et al found in their study of 137 patients with Grave s disease, that the psychiatric symptoms of anxiety and irritability were strongly associated with the disease [13]. Kathol and Delahunt reported that 60% of their hyperthyroid patients were found to have an anxiety disorder [14]. Other symptoms such as hypomania, mania, depression, psychosis, insomnia, attention and over activity problems, restlessness, fatigue, and delirium have also been associated with Grave s disease [14]. 17
THYROID HORMONE Ittermann et al found substantial evidence that untreated hypothyroidism is significantly associated with depression [15]. Observed additional psychological problems associated with hypothyroidism including attention deficits and cognitive disturbances [16] 18
HYPOTHALAMIC-PITUITARY- GONADAL AXIS 19
TESTOSTERONE Dabbs et al measured the free testosterone levels in saliva of 89 prisoners and found a strong association with higher testosterone levels in the prisoners who committed violent crimes versus those who committed non-violent crimes [17]. Other studies have also found that androgens have been associated with other psychiatric symptoms including anger, impulsivity, competitive traits, and violence [18]. 20
ESTROGEN AND PROGESERONE In women, the transition to menopause and its hormonal alterations has been associated with increased depression. In a study of 376 women near menopause, Mauas et al [19], found a high prevalence of a newly depressed mood among these women, who had no history of depression before menopause, and this was attributed to the ever changing hormonal setting seen during menopause. The exact cause is still unknown 21
ESTROGEN AND PROGESERONE Estrogen and Progesterone also influence the psychological behavior of an individual. In a study of 48 menopausal women, Sherwin [20] gave treatments to her patients and found that sexual desires and arousal were significantly higher in her treatment group compared with her plaecebo group. 22
PROLACTIN [18] The secretion of prolactin is increased by antipsychotic medications Hyperprolactinemia is associated with low testosterone in men and reduced libido in men and women. Patients with hyperprolactinemia often complain of depression, decreased libido, stress intolerance, anxiety, and increased irritability. These behavioral symptoms usually resolve in parallel with decrements in serum prolactin when surgical or pharmacological treatments are used. In psychotic patients, prolactin concentrations and prolactin- related sexual disturbances have been positively correlated with the severity of tardive dyskinesia . Prolactin levels are also positively correlated with negative symptoms in schizophrenia 23
OXYTOCIN [20] Oxytocin, also a posterior pituitary hormone, is involved in osmoregulation, the milk ejection reflex, food intake, and female maternal and sexual behaviors. Oxytocin is theorized to be released during orgasm, more so in women than in men, and is presumed to promote bonding between the sexes. It has been used in autistic children experimentally in an attempt to increase socialization 24
THE EFFECTS OF PSYCHOTROPIC DRUGS ON THE PITUITARY GLAND 25
THE EFFECTS ON PITUITARY GLAND VOLUME A pilot study was done to examine the effect of antipsychotics on pituitary volume in schizophrenic subjects. Pituitary volumes were measured in 16 patients with schizophrenia at baseline and 12 months after treatment with an antipsychotic medication using magnetic resonance imaging (MRI) [21]. A group of 12 healthy controls was evaluated at baseline and after 12 months. Pituitary volume significantly increased in the schizophrenic subjects after treatment (12% increase) [21]. This appeared to be specific to the prolactin-elevating drugs. In controls, pituitary volume did not change significantly (3% decrease) [21]. Pituitary volume may be a useful biomarker for treatments that affect neuroendocrine function [21]. 26
THE EFFECTS ON PITUITARY GLAND Dopamine acts on the pituitary as an inhibitor of prolactin secretion. Blockade of dopamine D2 receptors antipsychotics can cause hyperprolactinaemia in males and females [22]. Symptoms of hyperprolactinaemia include amenorrhoea, galactorrhoea, infertility, loss of libido and erectile dysfunction [22]. 27
THE EFFECTS ON PITUITARY GLAND Lithium at therapeutic serum levels main effect is inhibition of thyroid hormone release from the gland. The fall in circulating thyroid hormone levels causes an increase in serum thyroid- stimulating hormone (TSH), which can stimulate thyroid growth, resulting in goiter and nodularity. These effects of lithium on the thyroid gland are usually reversible when the drug is discontinued or when thyroid hormone replacement therapy is initiated [23] 28
CONCLUSION/ RECOMMENDATION As outlined in this presentation, I have been able to discuss my objectives and we have seen that psychological symptoms are found in a variety of endocrine conditions. I recommend that as clinicians, we should be very conscious of taking a detailed history and physical examination in order to identify these endocrine pathologies, and to refer appropriately for investigations and treatment. It is my hope that we will be more aware of these psychological issues so we can treat our patients in a more concise and effective way. 29
REFERENCES 1. Chin BM, Orlandi RR, Wiggins RH. Evaluation of the sellar and parasellar regions. Magn Reson Imaging Clin N Am. 2012 Aug;20(3):515-43. [PubMed] 2. Larkin S, Ansorge O. Development And Microscopic Anatomy Of The Pituitary Gland. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, Dungan K, Hershman JM, Hofland J, Kalra S, Kaltsas G, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferr re B, Levy M, McGee EA, McLachlan R, Morley JE, New M, Purnell J, Sahay R, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, editors. Endotext [Internet]. MDText.com, Inc.; South Dartmouth (MA): Feb 15, 2017. [PubMed] 30
REFERENCES 3. Al-Chalabi M, Bass AN, Alsalman I. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 25, 2022. Physiology, Prolactin. [PubMed]. 4. Nedresky D, Singh G. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Sep 26, 2022. Physiology, Luteinizing Hormone. [PubMed] 5. Sonino N, Fava GA (1998) Psychosomatic aspects of Cushing's disease. Psychother Psychosom 67: 140-146. 6. Starkman MN, Schteingart DE, Schork MA (1981) Depressed mood and other psychiatric manifestations of Cushing's syndrome: relationship to hormone levels. Psychosom Med 43: 3-18. 7. Haskett RF (1985) Diagnostic categorization of psychiatric disturbance in Cushing's syndrome. Am J Psychiatry 142: 911-916. 8. Kelly WF (1996) Psychiatric aspects of Cushing's syndrome. QJM 89: 543-551. 31
REFERENCES 9. Kelly WF, Kelly MJ, Faragher B (1996) A prospective study of psychiatric and psychological aspects of Cushing s syndrome. Clin Endocrinol (Oxf) 45: 715-720. 10. Sonino N, Fava GA, Belluardo P, Girelli ME, Boscaro M (1993) Course of depression in Cushing's syndrome: response to treatment and comparison with Graves' disease. Horm Res 39: 202-206. 11. Williams RH (1970) Metabolism and mentation. J Clin Endocrinol Metab 31: 461-479. 12. Anglin RE, Rosebush PI, Mazurek MF (2006) The neuropsychiatric profile of Addison's disease: revisiting a forgotten phenomenon. J Neuropsychiatry Clin Neurosci 18: 450-459. 32
REFERENCES 13. Stern RA, Robinson B, Thorner AR, Arruda JE, Prohaska ML, et al. (1996) A survey study of neuropsychiatric complaints in patients with Graves' disease. J Neuropsychiatry Clin Neurosci 8: 181-185. 14. Kathol RG, Delahunt JW (1986) The relationship of anxiety and depression to symptoms of hyperthyroidism using operational criteria. Gen Hosp Psychiatry 8: 23-28. 15. Ittermann T, V lzke H, Baumeister SE, Appel K, Grabe HJ (2015) Diagnosed thyroid disorders are associated with depression and anxiety. Soc Psychiatry Psychiatr Epidemiol 50: 1417-1425. 16. Almeida C, Brasil M, Costa AJL, Reis FAA, Reuters V, et al. (2007) Subclinical hypothyroidism: psychiatric disorders and symptoms. The Revista Brasileira de Psiquiatri 29: 157-159. 33
REFERENCES 17. Dabbs JM, Frady RL, Carr TS, Besch NF (1987) Saliva testosterone and criminal violence in young adult prison inmates. Psychosom Med 49: 174-182. 18. Sadock, B. J., Kaplan, H. I., & Sadock, V. A. (2015). Kaplan & Sadock s synopsis of psychiatry: Behavioral sciences / clinical psychiatry (11th ed. ). Philadepia: Wolter Kluwer / Lippincott Williams & Wilkins. 19. Mauas V, Kopala-Sibley DC, Zuroff DC (2014) Depressive symptoms in the transition to menopause: the roles of irritability, personality vulnerability, and self-regulation. Arch Womens Ment Health 17: 279-289. 20. Sherwin BB (1991) The impact of different doses of estrogen and progestin on mood and sexual behavior in postmenopausal women. J Clin Endocrinol Metab 72:336-343. 34
REFERENCES 21. Frank P. MacMaster, Rhonda El-Sheikh, Ameet R. Upadhyaya, Jeffrey Nutche, David R. Rosenberg, Matcheri Keshavan (2007) Effect of antipsychotics on pituitary gland volume in treatment- na ve first-episode schizophrenia: A pilot study. Schizophrenia Research, 9:21 3. 22.Hyperprolactinaemia With Antipsychotics [Internet]. www.medsafe.govt.nz. Available from: https://www.medsafe.govt.nz/profs/puarticles/hyperpro.htm 23. Bocchetta A, Cherchi A, Loviselli A, Mossa P, Velluzzi F, Derai R, Del Zompo M (1996), Six-year follow-up of thyroid function during lithium treatment. Acta Psychiatr Scand 94:45 Y 48. 35